Abstract
Background
Type IV dual left anterior descending artery (LAD) is a rare congenital coronary anomaly. Though benign with most of the patients being asymptomatic, knowledge of its existence and identification during coronary angiography is important during coronary interventions and surgical revascularization.
Case presentation
We present a rare case of type IV dual left anterior descending artery (LAD) with anomalous origin of one of the two vessels from the right coronary sinus. A 49-year-old female presented with inferior wall infarction and she underwent coronary angiography. Coronary angiogram showed triple vessel coronary artery disease. This rare variant of dual LAD was identified and was confirmed intra-operatively. The patient underwent coronary revascularization with grafts to both the LAD systems.
Conclusions
Proper assessment of the angiogram and knowledge of the coronary anomalies is required during surgical revascularization and percutaneous coronary interventions. This rare anomaly can be missed due to the anomalous origin of the LAD from the right coronary sinus. The identification of the dual LAD and grafting of both the LAD systems is required to achieve complete revascularization.
Similar content being viewed by others
Case presentation
A 49-year-old female presented to the cardiology department with complaints of chest pain. She was a diabetic and hypertensive of 10 years duration. Electrocardiogram was taken and she was diagnosed to have inferior wall myocardial infarction. Echocardiogram showed inferior wall hypokinesia and the ejection fraction was 47%. After stabilization coronary angiogram was planned. Coronary angiogram showed significant stenoses in left anterior descending artery (LAD), left circumflex artery (LCX), and right coronary artery (RCA) territories. The mid LAD seemed to be occluded and there was no retrograde filling of the distal LAD through collaterals. The patient did not have any wall motion abnormalities in the anterior segments. The patient was planned for coronary artery bypass grafting.
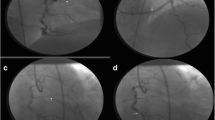
On further perusal of the angiogram, it was noted that an aberrant vessel was originating from the right coronary sinus running towards the interventricular groove and mimicking the course of the left anterior descending artery (Supplementary Video 1). The septals and diagonals seemed to arise from the presumed diagonal (Supplementary Video 2). This was consistent with the anatomy that has been described as type IV dual LAD. The aberrant vessel was the long LAD which entered the anterior interventricular groove and the presumed diagonal was in fact the short LAD. These findings were confirmed after pericardiotomy. The RIMA was harvested as she had significant proximal left subclavian artery stenosis. Saphenous veins were harvested from the left leg. After systemic heparinization Octopus stabilizer was used to immobilize the heart. Distal anastomosis of the RIMA was done to the long LAD using 8-0 propylene. Saphenous vein grafts were anastomosed to the short LAD, major Obtuse Marginal artery and Posterior Descending Artery using 7-0 propylene sutures. After completion of the distal anastomoses, partial clamp was applied to the aorta and proximal anastomoses were completed with 6-0 propylene sutures. The entire procedure was completed off-pump (Fig. 1). Protamine reversal was given and hemostasis was achieved. The post-operative course was uneventful and the patient is on regular follow-up for the past 2 years.
Post operatively the patient underwent computed tomography with contrast to clearly visualize the coronary anatomy and the same findings were observed with patents grafts in situ (Fig. 2). The patient is on regular follow-up and is symptom-free.
Discussion
Coronary artery anomalies are often observed on angiography. Their incidence ranges from 0.6% to 1.3% in various case series [1, 3]. Most of these anomalies are benign and do not necessitate any form of intervention [4].
Dual LAD is a rare coronary anomaly. Spindola-Franco et al. first described and classified dual LAD into four types [5]. With newer anomalies being reported it was reclassified into six types by Lee et al. [6, 7]. The classification is based on the origin and course of the short and long LAD and gives details with regards to the origin of the septal perforators and diagonals. Types IV, V, and VI have one of the LADs arising from the right coronary circulation.
Identifying the presence of these anomalous arteries is integral in the planning for myocardial revascularization. Type IV variant of dual LAD is very rare and can be missed on angiography [8, 9]. As the short LAD may give rise to the diagonals and septals the long LAD may be mistaken for an aberrant vessel/collateral. If both the short and long LADs are severely stenosed, grafts to both the vessels may be needed because the major supply to the septum and the anterior ventricular wall may come from both the vessels.
It is important that surgeons have a clear perspective about the origin and course of the LAD when these anomalies are observed. This will ensure that the surgeon avoids an incorrectly placed arteriotomy and that no territory is left without revascularization [10]. It is also emphasized that when there is a disparity between the angiographic anatomy and the coronary course seen intra-operatively, the angiogram should be reviewed again and a second perspective should be sought.
Careful review of the angiogram prior to surgery helped us to identify this coronary anomaly. The long LAD was visualized running an abnormal course and found lying in the mid to distal anterior interventricular groove. The short LAD was seen running lateral to the groove almost mimicking the course of a diagonal artery. Both the LADs were grafted separately and the myocardial revascularization was complete.
Conclusions
Proper assessment of the angiogram and knowledge of the coronary anomalies is required during surgical revascularization and percutaneous coronary interventions. This rare anomaly can be missed due to the anomalous origin of the LAD from the right coronary sinus. The identification of the dual LAD and grafting of both the LAD systems is required to achieve complete revascularization.
Availability of data and materials
Not applicable
Abbreviations
- LAD:
-
Left anterior descending artery
- LCX:
-
Left circumflex artery
- RCA:
-
Right coronary artery
- OM:
-
Obtuse marginal artery
- PDA:
-
Posterior descending artery
- RIMA:
-
Right internal mammary artery
References
Yamanaka O, Hobbs RE (1990) Coronary anomalies in 126,595 patients undergoing coronary arterigraphy. Catheter Cardiovasc Diagn 21:28–40
Subban V, Murdoch D, Pincus M (2014) Dual left anterior descending coronary artery with origin of short left anterior descending coronary artery from left main shaft: a rare coronary anomaly. J Invasive Cardiol 26:E59–E60
Angelini P, Villason S, Chan AV, Diez JG (1999) Normal and anomalous coronary arteries in humans. In: Angelini P (ed) Coronary artery anomalies: A comprehensive approach. Lippincott Williams and Wilkins, Philadelphia, pp 27–150.2
Shriki JE, Shinbane JS, Rashid MA, Hindoyan A, Withey JG, DeFrance A, Cunningham M, Oliveira GR, Warren BH, Wilcox A (2012) Identifying, characterizing, and classifying congenital anomalies of the coronary arteries. Radiographics. 32:453–468
Spindola-Franco H, Grose R, Solomon N (1983) Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Am Heart J 105:445–455
Lee Y, Lim YH, Shin J et al (2012) A case report of type VI dual left anterior descending coronary artery anomaly presenting with non-ST-segment elevation myocardial infarction. BMC Cardiovasc Disord 12:101
Maroney J, Klein LW (2012) Report of a new anomaly of the left anterior descending artery: Type VI dual LAD. Catheter Cardiovasc Interv 80(4):626–629
Kosar F (2006) An unusual case of double left anterior descending artery originating from the left and right coronary artery. Heart Vessel 21:385–387
Erbay AR, Turhan H, Senen K (2003) Double left anterior descending artery arising from the left main stem and right sinus of Valsalva: an extremely rare coronary artery anomaly. Acta Cardiol 58:417–419
Sajja LR, Farooqi A, Shaik MS, Yarlagadda RB, Baruah DK, Pothineni RB (2000) Dual left anterior descending coronary artery: surgical revasculazisation in 4 patients. Tex Heart Inst J 27:292–296
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
All the authors contributed to the editing and publishing of this case report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Angio sketch diagram 1–The position of the short LAD as seen in the angiogram.
Additional file 2: Figure S2.
Angio sketch diagram 2—A pictorial representation of position of normal LAD in the anterior interventricular groove which is not seen in the angiogram of this patient.
Additional file 3: Video 1. Coronary angiogram RAO cranial view showing the short LAD. Due to the anomalous long LAD running in the distal interventricular groove the proximal LAD seems to be cut-off at the mid segment.
Additional file 4: Video 2. Coronary angiogram of the right coronary artery shows the anomalous long LAD arising from the right coronary sinus running towards anterior interventricular groove.
Additional file 5. Left coronary injection showing the position of the short LAD running lateral to the anterior interventricular groove.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nedumaran, B., Krishnasamy, A., Ramasamy, M. et al. Surgical revascularization of a rare type IV dual left anterior descending artery—a case report. Cardiothorac Surg 30, 3 (2022). https://doi.org/10.1186/s43057-021-00062-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-021-00062-3