Abstract
Background
Surgical repair of total anomalous venous drainage (TAPVD) is lifesaving. The operative mortality is reported between 4 and 35%. Anatomical type, obstructed presentation, associated single ventricle, and heterotaxy syndromes are thought to influence short- and long-term outcomes. The effect of simple versus sutureless repair for primary surgery is unclear. This study reports the outcomes of the surgical repair and the effect of these variables in a contemporary setting.
Results
Between 2011 and 2019, all patients undergoing surgical repair for TAPVD were included. Operative mortality, length of hospital stay, and long-term survival were reported. The effect of anatomical type, surgical technique, obstruction, and associated lesions was assessed. Pearson’s test, Wilcoxson’s test, and generalized linear regression with Poisson distribution were used.
Forty-nine patients from two centers underwent TAPVD repair. The operative mortality was 4%. Postoperative pulmonary vein stenosis occurred in three patients, and reoperation was done in one patient. Survival free from reoperation was 98%, 98%, and 90% at 1, 24, and 60 months in the absence of pulmonary vein stenosis. However, all three patients who developed pulmonary vein stenosis died, at 0.5, 2.7, and 6.3 months of follow-up, respectively. We were unable to detect a significant effect of anatomical type, preoperative obstruction, associated single ventricle, or heterodoxy syndrome on operative mortality or long-term freedom from death or reoperation. Patients who presented with obstruction and infracardiac or supracardiac TAPVD had longer hospital stay.
Conclusion
TAPVD repair outcomes are excellent except for patients who develop postoperative pulmonary venous stenosis. Anatomical type, obstructed presentation, associated single ventricle, or heterotaxy are not significant predictors of survival.
Similar content being viewed by others
Background
Surgical correction is a lifesaving treatment for total anomalous pulmonary venous drainage (TAPVD). The operative mortality of surgery varies widely in the literature between 4 and 35% [1,2,3,4]. Anatomical type [5], stenosis of the drainage pathway [6], surgical technique [6,7,8,9,10,11,12], and time era all are reported to have an important effect of short- and long-term outcomes. Associated single ventricle anomalies carry a particularly poor prognosis [13]. The advent of the so-called sutureless techniques is thought to prevent stenosis and have an impact on long term outcomes [14, 15]. Pulmonary vein stenosis is a dreaded and relentless complication reported with all types of surgical techniques [9]. The use of modern postoperative measures including high-frequency jet ventilation (HFJV) and extracorporeal membrane oxygenation (ECMO) is thought to be helpful in some cases with obstructed TAPVD [16,17,18]. However, air embolism has been reported as a complication of aggressive ventilation that may be specific to sutureless repair [19].
This study describes the outcomes of surgical repair of TAPVD and the effect of anatomical and surgical factors.
Methods
Patients who underwent surgical repair of TAPVD from September 1, 2011, to December 13, 2019, were included. The data were collected retrospectively using an encrypted online database [20]. Five surgeons in two centers contributed to this cohort of patients. Follow-up was obtained by review of electronic records and direct contact of the treating physicians and the parents if recent data were not available in the records. The diagnosis was established by detailed echocardiographic studies and augmented with computed tomography and magnetic resonance imaging when the diagnosis and anatomical type was not clear by echocardiography.
The surgical methods included the use of cardiopulmonary bypass (CPB) with antegrade blood or Del Nido cardioplegia [21], and occasional periods deep hypothermic circulatory arrest. Direct suture technique between the posterior wall of the left atrium and the pulmonary venous confluence was the preferred technique. In the presence of small pulmonary veins or multiple venous confluences, sutureless techniques by suturing the incised left atrial wall to in situ pericardium around the incised pulmonary veins were used [14]. The draining vertical vein was ligated or divided when possible. In cases of infracardiac TAPVD or where the drainage vein was stenotic, it was left untouched. In cases of cardiac TAPVD, the dilated coronary sinus was completely unroofed and the atrial septation was recreated with a patch of autologous pericardium. If the pulmonary veins were small or stenotic, sutureless technique was applied. ECMO and HFJV were used only when necessary. Delayed sternal closure was also utilized if needed [22].
Statistical methods
The data were described as frequency and percent for categorical variables, and median and quartiles for continuous variables. The normality and linearity or continuous variables were assessed, and transformation or statistical methods suitable for such variables was used when necessary. The outcome measures of interest were operative mortality (OM) defined as death due to any cause during the index admission, postoperative length of stay (LOS) in the hospital, and long-term survival. The need for reoperation for pulmonary vein stenosis was recorded. The effect of anatomical type, simple versus sutureless repair technique, associated single ventricle lesions, and heterotaxy syndromes as well as demographic variables was assessed. For OM, due to its rarity, Pearson chi-square with continuity correction or Wilcoxon test was used for categorical and continuous variables, respectively. For LOS, the analysis was limited to survivors and a multivariable generalized linear regression model with Poisson distribution was used. For long-term survival, Kaplan-Meier survival analysis was used for the graphical description of freedom from death or reoperation. Log-rank test was used to test for significant associations. All statistical analyses were done using the R statistical system with Hmisc and rms packages [23,24,25].
Results
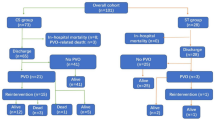
In the study period, 49 patients underwent primary TAPVD repair. The anatomical type distribution was supracardiac in 51% (25), cardiac in 18% (9), infracardiac in 16% (8), and mixed in 14% (7) of the patients. Single ventricle lesions and heterotaxy syndromes were each present in 12% (6) of the patients. According to risk adjustment in congenital heart surgery (RACHS-1) risk categorization, patients who underwent surgery before 30 days of age were classified as category 4, 22% (11), and those who were 30 days of age or older were classified as category 2, 78% (39) regardless of anatomical type or associated lesions [24]. Approximately one third of the patients, 29% (14), presented with obstructive symptoms and required emergency surgery. The frequency of presentation with obstruction was significantly higher in infracardiac TAPVD (87.5%) compared to the other types (11–12%), P value < 0.001. Moreover, the median age at operation was significantly younger in patients with infracardiac TAPVD, P value = 0.01. There were two main surgeons contributing 67% (33) and 16% (8) of the patients, respectively. The remaining three surgeons contributed less patients. Table 1 shows the details of the patient demographics grouped by anatomical type of TAPVD.
The CPB and aortic cross-clamp times were higher for mixed type TAPVD, P value < 0.001. However, delayed sternal closure was highest in infracardiac TAPVD, P value < 0.001. There were two deaths during the hospital stay, one for infracardiac and one for cardiac TAPVD, and overall OM was 4% (2/49) and was not significantly different between neonates and older children, P value = 0.9; the anatomical TAPVD types, P value 0.55; or presentation with obstruction, P value 0.8. Completeness of follow-up was 96%, and there were two late deaths at 6 and 49 months. One of the late deaths was related to pulmonary vein stenosis in a patient who presented 6 months after surgery to the emergency department at a peripheral hospital and was not fit for transport to a cardiac surgical facility. The cause of death in the other patient who died at 49-month follow-up is unknown. Three patients were diagnosed with postoperative pulmonary vein stenosis at 2 weeks, 6 months, and 49 months after the primary surgery. The patient diagnosed at 2 weeks postoperatively was a patient with supracardiac TAPVD who was discovered to have retroesophageal course of the venous confluence draining vein [26]. She underwent reoperation during the same hospital admission and remains asymptomatic at 5 months’ follow-up after the reoperation. The patient who was diagnosed at 6 months is the same patient who was reported above as a late death and did not undergo reoperation. The third patient with presumed pulmonary vein stenosis had infracardiac TAPVD. Her initial presentation was with obstructed TAPVD and had a complicated postoperative course and was not fit to undergo reoperation (Table 2).
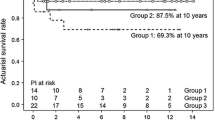
Over long-term follow-up, pulmonary vein stenosis was significantly associated with death or reoperation, Fig. 1, P value < 0.001. However, the anatomical type of TAPVD and repair technique were not significantly associated with freedom from death or reoperation, Figs. 2 and 3, respectively. The presence of preoperative obstructed TAPVD also did not affect the long-term freedom from death or reoperation, P value 0.5.
Obstructed presentation was significantly associated with prolonged hospital stay in survivors, P value = 0.002, Fig. 4. The prolonged hospital stay was also significantly associated with infracardiac and supracardiac TAPVD types and with body surface area in a non-linear fashion, Fig. 4. Single ventricle anomalies, heterotaxy syndrome, and age at operation were not significant predictors of postoperative hospital stay, Fig. 4.
Predictors of postoperative length of stay using a generalized linear model with Poisson distribution. Test shown is Wald statistic of model analysis of variance. SV: single ventricle anomalies, TAPVDtype: anatomical TAPVD type, Crdc: cardiac TAPVD, Infr: infracardiac TAPVD, Mixd: mixed TAPVD, Sprc: supracardiac TAPVD, BSA: body surface area
Discussion
In a recent meta-analysis of 26 studies involving over 2700 patients, Wu et al. concluded that primary sutureless repair was associated with less post-operative pulmonary vein stenosis and need for reoperation; however, there was no difference in early late or overall survival [10]. In line with that, we did not find any significant association between the repair technique and freedom from death or reoperation; the determination of whether the type of surgical technique is associated with postoperative stenosis and long-term outcomes is in need for prospective randomized trials and cannot be made from retrospective studies.
There were only two deaths before hospital discharge and two late deaths; therefore, we were not able to perform a multivariable analysis for survival. However, in univariable analysis, we did not find that neonatal age, weight, TAPVD anatomical type, or presentation with obstruction were significantly associated with operative or long-term death. This contrasts with the findings of the larger and more long-term studies like Yong et al. [13] and Sakamoto et al. [4] which showed that neonatal age, weight less than 2 kg, and mixed TAPVD were factors associated with reduced survival.
The current study has shown that pulmonary vein stenosis is an important predictor of long-term freedom from death or reoperation. It is our current belief that if surgery can be done avoiding postoperative pulmonary vein stenosis, then the outcomes should be very good regardless of other factors [27, 28].
The presence of TAPVD in association with heterotaxy syndromes and single ventricle anomalies is believed to be a poor prognostic indicator, and some would deny such patients’ surgical care. In the current study, we did not find that to be justifiable. This is consistent with the reporting of outcomes of patients who underwent TAPVD repair with single ventricle anomalies and then went on to receive a Fontan operation, Yong et al. [13]. The outcomes of patients who had TAPVD repair then Fontan operation were comparable to Fontan patients without TAPVD repair.
The present study is limited by its retrospective nature and small number of patients and outcomes. However, it represents the complete experience of two surgical centers over an 8-year period with near-complete follow-up.
Conclusion
Surgical correction of TAPVD is a lifesaving operation and is applicable to patients who present with this anomaly regardless of age, weight, anatomical type, heterotaxy, or single ventricle anomalies. Preoperative obstruction of the pulmonary venous pathway is likely a significant factor in the patient reaching or failing to reach the operative setting; however, once the repair is performed, preoperative obstruction does not affect long-term outcome but may prolong the hospital stay. It is the development of postoperative pulmonary vein stenosis that significantly reduces freedom from death and reoperation.
Availability of data and materials
Data are available with the author upon request.
Abbreviations
- CPB:
-
Cardiopulmonary bypass
- ECMO:
-
Extracorporeal membrane oxygenation
- HFJV:
-
High-frequency jet ventilation
- LOS:
-
Length of stay
- OM:
-
Operative mortality
- RACHS-1:
-
Risk adjustment in congenital heart surgery
- TAPVD:
-
Total anomalous venous drainage
References
Harada T, Nakano T, Oda S, Kado H (2019) Surgical results of total anomalous pulmonary venous connection repair in 256 patients. Interact Cardiovasc Thorac Surg. 28(3):421–426. https://doi.org/10.1093/icvts/ivy267
Kogon B, Fernandez J, Shashidharan S, Kanter K, Alsoufi B (2017) A 30-year experience with mixed-type total anomalous pulmonary venous connection: a word of caution. Cardiol Young. 27(5):870–876. https://doi.org/10.1017/S1047951116001414
Lemaire A, DiFilippo S, Parienti J-J et al (2016) Total anomalous pulmonary venous connection: a 40 years’ experience analysis. Thorac Cardiovasc Surg. 65(01):009–017. https://doi.org/10.1055/s-0036-1588007
Sakamoto T, Nagashima M, Umezu K et al (2018) Long-term outcomes of total correction for isolated total anomalous pulmonary venous connection: lessons from 50-years’ experience†. Interact Cardiovasc Thorac Surg. 27(1):20–26. https://doi.org/10.1093/icvts/ivy034
Edwards JE, Helmholz HF (1956) A classification of total anomalous pulmonary venous connection based on developmental considerations. Proc Staff Meet Mayo Clin. 31(6):151–160
Nabar A, Dalvi B (1998) Obstructive total anomalous pulmonary venous drainage. Indian J Pediatr. 65(1):35–45. https://doi.org/10.1007/bf02849692
Alsoufi B (2014) Modified primary sutureless repair technique of total anomalous pulmonary venous connection. World J Pediatr Congenit Heart Surg. 5(2):302–305. https://doi.org/10.1177/2150135113519452
Kim H, Sung SC, Choi KH, Lee HD, Kim G, Ko H (2018) Primary sutureless repair of total anomalous pulmonary venous connection: suture-and-open technique. Ann Thorac Surg. 106(5):e273–e276. https://doi.org/10.1016/j.athoracsur.2018.05.026
Tremblay C, Yoo S-J, Mertens L et al (2018) Sutureless versus conventional pulmonary vein repair: a magnetic resonance pilot study. Ann Thorac Surg. 105(4):1248–1254. https://doi.org/10.1016/j.athoracsur.2017.11.015
Wu Y, Wu Z, Zheng J et al (2018) Sutureless technique versus conventional surgery in the primary treatment of total anomalous pulmonary venous connection: a systematic review and meta-analysis. J Cardiothorac Surg. 13(1):69. https://doi.org/10.1186/s13019-018-0756-z
Yun T-J, Coles JG, Konstantinov IE et al (2005) Conventional and sutureless techniques for management of the pulmonary veins: evolution of indications from postrepair pulmonary vein stenosis to primary pulmonary vein anomalies. J Thorac Cardiovasc Surg. 129(1):167–174. https://doi.org/10.1016/j.jtcvs.2004.08.043
Yanagawa B, Alghamdi AA, Dragulescu A et al (2011) Primary sutureless repair for “simple” total anomalous pulmonary venous connection: midterm results in a single institution. J Thorac Cardiovasc Surg. 141(6):1346–1354. https://doi.org/10.1016/j.jtcvs.2010.10.056
Yong MS, Zhu MZL, du Plessis K et al (2019) Long-term outcomes of the Fontan operation in patients with total anomalous pulmonary venous drainage. Ann Thorac Surg. 108(4):1234–1241. https://doi.org/10.1016/j.athoracsur.2019.04.073
Najm HK, Caldarone CA, Smallhorn J, Coles JG (1998) A sutureless technique for the relief of pulmonary vein stenosis with the use of in situ pericardium. J Thorac Cardiovasc Surg. 115(2):468–470. https://doi.org/10.1016/S0022-5223(98)70294-6
Lacour-Gayet F, Rey C, Planché C (1996) Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ. Arch Mal Coeur Vaiss. 89(5):633–636
Ross FJ, Joffe D, Latham GJ (2017) Perioperative and anesthetic considerations in total anomalous pulmonary venous connection. Semin Cardiothorac Vasc Anesth. 21(2):138–144. https://doi.org/10.1177/1089253216672012
ElMahrouk AF, Ismail MF, Hamouda T, Shaikh R, Mahmoud A, Shihata MS, Alradi O, Jamjoom A (2019) Extracorporeal membrane oxygenation in postcardiotomy pediatric patients-15 years of experience outside Europe and North America. Thorac Cardiovasc Surg. 67(1):28–36. https://doi.org/10.1055/s-0037-1608962 Epub 2017 Dec 12
Dohain AM, Abdelmohsen G, Elassal AA, ElMahrouk AF, Al-Radi OO (2019) Factors affecting the outcome of extracorporeal membrane oxygenation following paediatric cardiac surgery. Cardiol Young. 20:1–9. https://doi.org/10.1017/S1047951119002634 [Epub ahead of print]
Alghamdi AA, Coles JG, Holtby H, Al-Radi OO (2010) Massive air embolism after the repair of obstructed total anomalous pulmonary venous drainage: an unusual complication. J Card Surg. 25(5):582–584. https://doi.org/10.1111/j.1540-8191.2010.01065.x
Williams WG. CCSDB: Congenital Cardiac Surgery Database. ccsdb.org.
del Nido PJ (1997) Myocardial protection and cardiopulmonary bypass in neonates and infants. Ann Thorac Surg. 64(3):878–879. https://doi.org/10.1016/s0003-4975(97)00696-6
Elassal AA, Eldib OS, Dohain AM, Abdelmohsen GA, Abdalla AH, Al-Radi OO (2019) Delayed sternal closure in congenital heart surgery: a risk-benefit analysis. Heart Surg Forum. 22(5):E325–E330. https://doi.org/10.1532/hsf.2471
Core R (2019) Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical. Computing https://www.R-project.org/
Jr FEH (2019) Dupont with contributions from C, others many. Hmisc, Harrell Miscellaneous. https://CRAN.R-project.org/package=Hmisc
Jr FEH. Rms: regression modeling strategies.; 2019. https://CRAN.R-project.org/package=rms.
Rodriguez ML, Caldarone CA, Toeg H, Maharajh G (2019) Retroesophageal infracardiac total anomalous pulmonary venous drainage. World J Pediatr Congenit Heart Surg. 10(3):367–369. https://doi.org/10.1177/2150135117731893
Mohamed Fouad Ismail, Amr A. Arafat, Tamer E. Hamouda, Amira Esmat El Tantawy, Azzahra Edrees, Abdulbadee Bogis, Nashwa Badawy, Alaa B. Mahmoud, Ahmed Farid Elmahrouk & Ahmed A. Jamjoom : Junctional ectopic tachycardia following tetralogy of fallot repair in children under 2 years Journal of Cardiothoracic Surgery volume 13, Article number: 60 (2018)
Ismail MF, Elmahrouk AF, Arafat AA, Hamouda TE, Alshaikh BA, Shihata MS, Jamjoom AA, Al-Radi OO Evolution of the Norwood operation outcomes in patients with late presentation. The Journal of Thoracic and Cardiovascular Surgery https://doi.org/10.1016/j.jtcvs.2019.07.154
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
OOA conducted the literature search; designed the study; performed the data collection, analysis, and interpretation of data; conducted the statistical analysis; and drafted the manuscript. AE supervised the study and conducted the review of data, involved in the study design, analyzed and interpreted the data, and drafted the manuscript. MI designed the study, analyzed and interpreted the data, and drafted the manuscript. AH conducted the statistical analysis, performed the data collection, conducted the literature search, and interpreted the data. TH conducted the literature search, analyzed and interpreted the data, performed the data collection, and drafted the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local institutional review board (IRB), at King Abdulaziz University, with reference number (713/19), and the patients’ consent was waived for this retrospective observational study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Al-Radi, O.O., Elmahrouk, A., Ismail, M. et al. Total anomalous pulmonary venous drainage repair: the effect of anatomical type and pulmonary vein stenosis on outcomes. Cardiothorac Surg 28, 7 (2020). https://doi.org/10.1186/s43057-020-0016-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-020-0016-6