Abstract
Background
The relationship between sarcopenia and the consequences of COVID-19 is not yet fully understood. It is noteworthy that information about muscle status can be easily retrieved by segmenting specific regions of skeletal muscles on CT scans. Our aim in this study was to investigate the relationship between sarcopenia and the consequences of COVID-19.
Methods
In this analytical cross-sectional study, 338 patients with COVID-19 who had a positive PCR test for COVID-19 and underwent chest CT scan in Loghman-e-Hakim Hospital from July to September 2021 were evaluated. Age, sex, background diseases, mechanical ventilation, duration of hospitalization, as well as lab tests, ICU admission and mortality were extracted from patient records. The severity of COVID-19 disease and the area and density of paraspinal muscles at the level of T5 and T12 vertebrae were evaluated through chest CT scans.
Results
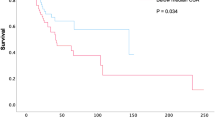
Length of stay had significant relationship with T5 density (1.15 (< 0.001)) and T12 density (1.24 (< 0.001). The mean of T12 area (3.35 (P = 0.005) and T12 density 4.59 (P = 0.012) were significantly lower in ICU admitted. There was a significant relationship between mortality and age, cardiovascular disorders, COPD, underlying disease, length of stay, WBC and lymphocyte levels, as well as the severity of the disease.
Conclusions
Based on the results of this study, we can infer that the use of CT scan in patients with COVID-19 and the determination of muscle area and density can predict the consequences of COVID-19, such as a longer duration of hospitalization, the need for admission to the ICU, and mortality.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The COVID-19 disease is caused by the acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and was first identified in Wuhan, China, in December 2019 [41]. Every day, people around the world are getting infected with this virus. According to various studies, many comorbidities have been identified that increase the probability of the disease progressing to a severe type, such as chronic obstructive respiratory disease (COPD), cardiovascular disease (CVD), obesity, and other conditions that suppress the immune system [19, 22,23,24,25,26,27], Obesity, diabetes mellitus (DM), and high blood pressure are among the comorbidities seen in hospitalized patients following COVID-19 [21, 52].
Identifying these factors can be beneficial for disease risk assessment and balancing hospital resources. Correlations have been seen between obesity and poor infection recovery outcomes in patients admitted to the intensive care unit (ICU), especially when sarcopenia is seen in association with overweight [13, 31, 34]. Obese patients have a higher risk of hospital and ICU admission, mechanical ventilation, and death [30, 48]. It has been shown that, in addition to weight, muscle volume reduction, especially in the chest, is associated with poor outcomes in the management of Covid-19 infection [17]. Sarcopenia is an age-related clinical syndrome characterized by progressive loss of skeletal muscle mass and strength [12].
Sarcopenia can be a cause for different courses of the Covid-19 disease between patients or a symptom of other diseases that lead to different courses of the disease. The relationship between sarcopenia and the consequences of Covid-19 is not yet fully understood [43]. It is noteworthy that information about muscle status can be easily retrieved by segmenting specific regions of skeletal muscles [3, 8, 18, 46]. Our aim in this study was to investigate the relationship between sarcopenia and the consequences of Covid-19 disease in patients with Covid-19 admitted to Loghman-e-Hakim Hospital from July to September 2021.
Methods
This study was conducted using a cross-sectional analytical method on patients with COVID-19 who were admitted to Loghman-e-Hakim Hospital from July to September 2021. Patients who were admitted to the hospital with a positive polymerase chain reaction (PCR) test for COVID-19 and underwent a chest CT scan in the first 24 h of admission, were included in the study. Patients with underlying neurological diseases, malignancies, and those under the age of 18 were excluded from the study.
While the COVID-19 disease outbreak took place in Iran, our tertiary referral center, encountered daily rises in the number of chest CT scan requests. A remarkable number of cases were younger than 40 years old and according to the Iranian Radiology Society (ISR) consensus [38], we applied a low-dose chest CT protocol mainly adjusted from lung cancer screening CT protocol [10]. Therefore, patients presenting in earlier days, underwent standard-dose CT scan; whereas, more recent cases underwent the low-dose protocol. Scanning parameters are presented in Table 1. Images were obtained with one of two CT scanners (Activion 16, Toshiba, Japan and Somatom scope power 16, Siemens Healthineers, Germany). The CT scan results were instantly transferred to picture archiving and communication system (PACS). Preliminary reports where available within 2 h.
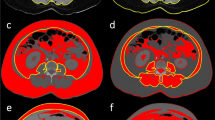
Demographic information of patients, including age, sex, and underlying diseases such as DM, CVD, respiratory disease (asthma and COPD), chronic kidney disease (CKD), immune system deficiency, mechanical ventilation, the hospitalization time, as well as laboratory tests including white blood cell (WBC) and lymphocytes count, ICU admission, and mortality, was extracted from patient records. Additionally, the severity of COVID-19 disease and the area and density of paraspinal muscles at the level of T5 and T12 vertebrae (Figs. 1, 2, 3, 4) were evaluated by two experienced radiologists through observation and evaluation of chest CT scans of patients. In case of disagreement, a third person with more experience made the decision.
The severity of COVID-19 disease was quantitatively classified as follows: [4]
Illness severity: Score 1: No ground glass or consolidation/ Score 2: The presence of ground glass opacities without consolidation Score/ 3: Simultaneous presence of ground glass opacities and consolidation/ Score 4: Presence of consolidation without ground glass opacities (Figs. 5, 6, 7, 8).
The data was analyzed using SPSS statistical analysis software. Independent sample T test, ANOVA, univariate and multivariate linear or logistic regression were used for analysis based on dependent variable. In Table 5, we ran a multiple linear regression with all of the variables (mortality, hospitalization time, ICU admission, mechanical ventilation, severity), and in Table 6, association between mortality and variables, was adjusted for T5 area and density and T12 area and density. In this study, written consent was obtained from the patients. All information was kept confidential, and all provisions of the Declaration of Helsinki were observed at every stage of the research.
Results
In this article, which examines the relationship between sarcopenia and the consequences of Covid-19 disease, 383 patients with Covid-19 were examined, of whom 199 (52%) were men and 184 (48%) were women. The average age of these patients was 53.85 (SD = 18.61) years.
Tables 2 and 3 describe the frequency of underlying diseases and other studied variables. In order to analyze the data, the distribution of quantitative variables was checked. All items except WBC had a normal distribution. Non-parametric tests were used for WBC.
The area and density of the paraspinal muscles at the level of T5 and T12 vertebrae were investigated and compared separately by demographic variables and are shown in Table 4.
In order to predict the consequences of disease and mortality based on sarcopenia criteria, linear regression and logistic regression models were used, respectively, and the results are shown in Tables 5 and 6.
Table 5 shows the association between the studied variables and the outcome, including T5 muscular area, T5 muscular density, T12 muscular area and T12 muscular density, which are shown both in Unadjusted and Adjusted analysis. About the association between mortality with muscle loss, we showed mass of muscle was losses Compared with patients who were alive, we saw same results in T5 area and density and T12 area and density. All outcomes in the unadjusted analysis were significant, but in the adjusted state for the variables shown in Table 6, it can be said that the longer the length of stay in the hospital, the average T5 muscular density and T12 muscular density decrease by 1.15 and 1.24 units, respectively. This amount was statistically significant (P < 0.001). It can also be said that the average T12 area and T12 density were significantly lower in people admitted to the ICU (3.35 (P = 0.005) and 4.59 (P = 0.012) units, respectively).
Considering that the association of mortality with mechanical ventilation and ICU admission was not precise and was overestimated, we did not include these two variables in the model.
Table 6 shows the association of mortality with the studied variables, including age, sex, DM, cardiovascular disorders, COPD, CKD, immunodeficiency, underlying disease, the hospitalization time, WBC and lymphocyte count, as well as the severity of the disease. It is shown in four modes: Unadjusted mode and then Adjusted mode for T5 muscular area and T5 muscular density, and T12 muscular area and T12 muscular density.
Based on the results shown in the Unadjusted mode, there was a significant association between mortality and age, cardiovascular disorders, COPD, underlying disease, the hospitalization time, WBC and lymphocyte counts, as well as the severity of the disease.
Discussion
The aim of the present study was to investigate whether sarcopenia can predict the consequences of COVID-19 disease, such as a longer hospitalization time, the need for ICU admission, intubation, and mortality related to this disease. Sarcopenia is a condition of severe muscle failure that is common in the hospitalized population and is associated with an increased risk of side effects, including increased length of hospital stay and mortality [14, 28, 37, 40]. In previous studies, the relationship between sarcopenia and COVID-19 has been discussed, and the relationship between the hospitalization time and acute changes in the sarcopenia status of the elderly has been shown [20, 45]. In studies of hospitalized patients with COVID-19 during the pandemic, biochemical evidence of muscle wasting has been reported [49], and it is thought that patients with COVID-19 are at risk of developing acute sarcopenia. This condition is characterized by a decrease in muscle mass and strength [9, 32]. These muscle changes predict poor prognosis in patients, longer hospitalization and ICU admission [1, 5, 29, 50], more ICU admissions [2], failure of extubation [29], a worse situation [7, 16, 44], and more mortality [29, 39]. The results of our study are consistent with several studies in this field that have shown the importance of sarcopenia in the adverse outcomes of patients in many diseases [6, 33, 36, 51]. Low muscle mass can affect the function of the respiratory system and the pectoralis and intercostal muscles [15, 35, 47]. Respiratory muscles, along with pharyngeal muscles, play an important role in causing coughs. Coughing itself is a defense mechanism against lung infections. Therefore, respiratory muscle disorders in patients with sarcopenia, can cause difficulties in the normal course of the cough reflex and cause failure in ventilation and acceleration of lung infections [11, 42].
If the relationship between low muscle mass and the negative consequences of COVID-19 is confirmed, the role of CT scan in diagnosis, monitoring, and prediction of prognosis will be more prominent. The strength of our study is the large sample size. One of the limitations of this study is that the evaluation is limited to hospitalized patients. Also, due to the fact that this study was a retrospective study, the patient’s information was not complete, and we did not have access to some important variables such as the weight and height of some patients. Furthermore, other risk factors such as habits and lifestyle, nutrition, physical activity, etc. related to patients before contracting COVID-19 and being hospitalized are effective in changing muscle condition, which were not investigated in this study. In this study, sarcopenia was investigated based on the density and area of muscle mass, and due to the limitations of the pandemic time in hospitals, measures such as grip strength, dual-energy X-ray absorptiometry (DXA), chair stand tests, and 400-m walk tests were not performed. It is suggested that longitudinal and prospective studies be conducted, considering these variables as well as the initial muscle condition, to determine whether sarcopenia occurs before or after the infection with COVID-19.
Conclusions
Based on the results of this study, it can be inferred that the use of CT scan in patients with COVID-19 and the determination of muscle area and density can predict the consequences of the disease of COVID-19, such as a longer hospitalization, the need for ICU admission, and mortality.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The material is fully explained in the “Methods” section.
Abbreviations
- COVID-19:
-
Coronavirus- 19
- CT scan:
-
Computed Tomography
- ICU:
-
Intensive Care Unit
- WBC:
-
White blood cell
- SARS-CoV-2:
-
Acute Respiratory Syndrome Coronavirus 2
- COPD:
-
Chronic Obstructive Respiratory Disease
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- PCR:
-
Polymerase chain reaction
- CKD:
-
Chronic kidney disease
- SPSS:
-
Statistical Package for the Social Sciences
- ANOVA:
-
Analysis of variance
- SD:
-
Standard deviation
References
Ahmed S et al (2021) ‘A five-day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Diseases: IJID 103:214–216. https://doi.org/10.1016/j.ijid.2020.11.191
Chachar AZK (2020) Effectiveness of ivermectin in SARS-CoV-2/COVID-19 patients. Int J Sci 09:31–35
Albano D et al (2020) ‘Imaging of sarcopenia: old evidence and new insights. Eur Radiol 30(4):2199–2208. https://doi.org/10.1007/s00330-019-06573-2
Albano D, et al (2021) CT-derived chest muscle metrics for outcome prediction in COVID-19 patients. In: 28th Annual Scientific Meeting of the European Society of Musculoskeletal Radiology (ESSR), Virtual Edition, June 2021, vol 25(10). https://doi.org/10.1055/s-0041-1731545
Babalola OE et al (2022) ‘Ivermectin shows clinical benefits in mild to moderate COVID19: a randomized controlled double-blind, dose-response study in Lagos. QJM: Mon J Assoc Physic 114(11):780–788. https://doi.org/10.1093/qjmed/hcab035
Baracos VE, Arribas L (2018) Sarcopenic obesity: hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann Oncol Off J Eur Soc Med Oncol 29(suppl_2):ii1–ii9. https://doi.org/10.1093/annonc/mdx810
Beltran Gonzalez JL et al (2022) Efficacy and safety of ivermectin and hydroxychloroquine in patients with severe COVID-19: A randomized controlled trial. Infect Disease Rep 14(2):160–168. https://doi.org/10.3390/idr14020020
Boutin RD et al (2020) Association of adipose tissue and skeletal muscle metrics with overall survival and postoperative complications in soft tissue sarcoma patients: an opportunistic study using computed tomography. Quant Imaging Med Surg 10(8):1580–1589. https://doi.org/10.21037/qims.2020.02.09
Caly L et al (2020) The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiv Res 178:104787. https://doi.org/10.1016/j.antiviral.2020.104787
American Association of Physicists in Medicine (2023) Lung cancer screening CT protocols version 6. AAPM's working group on standardization of CT nomenclature and protocols. AAPM (updated November 2023), pp 1–19
Chang AB (2006) The physiology of cough. Paediatric Respirat Rev 7(1):2–8. https://doi.org/10.1016/j.prrv.2005.11.009
Chianca V et al (2022) Sarcopenia: imaging assessment and clinical application. Abdoml Radiol (New York) 47(9):3205–3216. https://doi.org/10.1007/s00261-021-03294-3
Dietz W, Santos-Burgoa C (2020) Obesity and its implications for COVID-19 mortality. Obesity (Silver Spring, Md). https://doi.org/10.1002/oby.22818
Du Y et al (2014) ‘Sarcopenia is a predictor of outcomes in very elderly patients undergoing emergency surgery. Surgery 156(3):521–527. https://doi.org/10.1016/j.surg.2014.04.027
Ekiz T et al (2020) Sarcopenia and COVID-19: a manifold insight on hypertension and the renin angiotensin system. Am J Phys Med Rehabil 99(10):880–882. https://doi.org/10.1097/PHM.0000000000001528
Elgazzar A et al (2020) Efficacy and safety of Ivermectin for treatment and prophylaxis of COVID-19 pandemic. Res Square 3(1):1–9
Fang Y et al (2020) Sensitivity of Chest CT for COVID-19: comparison to RT-PCR. Radiology 296(2):E115–E117. https://doi.org/10.1148/radiol.2020200432
Giraudo C et al (2020) Established paths and new avenues: a review of the main radiological techniques for investigating sarcopenia. Quant Imaging Med Surg 10(8):1602–1613. https://doi.org/10.21037/qims.2019.12.15
Gold MS et al (2020) COVID-19 and comorbidities: a systematic review and meta-analysis. Postgraduate Med 132(8):749–755. https://doi.org/10.1080/00325481.2020.1786964
Götz V et al (2016) Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import. Sci Rep 6:23138. https://doi.org/10.1038/srep23138
Guan W-J et al (2020) Clinical Characteristics of Coronavirus Disease 2019 in China. New Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Hariyanto TI, Halim DA et al (2021) Colchicine treatment can improve outcomes of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Clin Exp Pharmacol Physiol 48(6):823–830. https://doi.org/10.1111/1440-1681.13488
Hariyanto TI et al (2021) Human immunodeficiency virus and mortality from coronavirus disease 2019: a systematic review and meta-analysis. Southern Afr J HIV Med 22(1):1220. https://doi.org/10.4102/sajhivmed.v22i1.1220
Hariyanto TI, Intan D et al (2021) Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): a systematic review, meta-analysis, and meta-regression. Diabetes Res Clin Pract 179:109031. https://doi.org/10.1016/j.diabres.2021.109031
Hariyanto TI et al (2022) Ivermectin and outcomes from Covid-19 pneumonia: a systematic review and meta-analysis of randomized clinical trial studies. Rev Med Virol. https://doi.org/10.1002/rmv.2265
Hariyanto TI, Kurniawan A (2021) Obstructive sleep apnea (OSA) and outcomes from coronavirus disease 2019 (COVID-19) pneumonia: a systematic review and meta-analysis. Sleep Med 82:47–53. https://doi.org/10.1016/j.sleep.2021.03.029
Hariyanto TI, Kurniawan A (2021) Statin and outcomes of coronavirus disease 2019 (COVID-19): A systematic review, meta-analysis, and meta-regression. Nutr Metab Cardiovasc Diseases: NMCD 31(6):1662–1670. https://doi.org/10.1016/j.numecd.2021.02.020
Huang D-D, et al (2015) Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Colorectal Disease: Off J Assoc Coloproctol Great Britain Ireland 17(11):O256–64. https://doi.org/10.1111/codi.13067
Huang J et al (2016) Perioperative antibiotics to prevent acute endophthalmitis after ophthalmic surgery: a systematic review and meta-analysis. PLoS ONE 11(11):e0166141. https://doi.org/10.1371/journal.pone.0166141
Huang Y et al (2020) Obesity in patients with COVID-19: a systematic review and meta-analysis. Metab: Clin Exp 113:154378. https://doi.org/10.1016/j.metabol.2020.154378
Hussain A et al (2020) Obesity and mortality of COVID-19. Meta-analysis. Obesity Res Clin Pract 14(4):295–300. https://doi.org/10.1016/j.orcp.2020.07.002
Jadad AR et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Ji Y et al (2018) Impact of sarcopenic obesity on 30-day mortality in critically ill patients with intra-abdominal sepsis. J Crit Care 46:50–54. https://doi.org/10.1016/j.jcrc.2018.03.019
Kassir R (2020) ‘Risk of COVID-19 for patients with obesity. Obes Rev: Off J Int Assoc Study Obes. https://doi.org/10.1111/obr.13034
Kottlors J et al (2020) Body composition on low dose chest CT is a significant predictor of poor clinical outcome in COVID-19 disease - A multicenter feasibility study. Eur J Radiol 132:109274. https://doi.org/10.1016/j.ejrad.2020.109274
Kroenke CH et al (2018) Muscle radiodensity and mortality in patients with colorectal cancer. Cancer 124(14):3008–3015. https://doi.org/10.1002/cncr.31405
Lieffers JR et al (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936. https://doi.org/10.1038/bjc.2012.350
Mahdavi A, et al (no date) Radiologic management of COVID-19: preliminary experience of the Iranian Society of Radiology COVID-19 Consultant Group (ISRCC). Iran J Radiol 17(2):e102324. https://doi.org/10.5812/iranjradiol.102324
Military C, et al (2021) Efficacy of ivermectin in COVID-19 patients with mild to
Reisinger KW et al (2015) Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg 261(2):345–352. https://doi.org/10.1097/SLA.0000000000000628
Richardson S et al (2020) Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 323(20):2052–2059. https://doi.org/10.1001/jama.2020.6775
Shakerian N et al (2020) Potential prophylactic and therapeutic effects of respiratory physiotherapy for COVID-19. Acta bio-medica: Atenei Parmensis 92(1):e2021020. https://doi.org/10.23750/abm.v92i1.10289
Siahaan YMT et al (2022) Coronavirus disease 2019 (Covid-19) outcomes in patients with sarcopenia: a meta-analysis and meta-regression. Clin Nutr ESPEN 48:158–166. https://doi.org/10.1016/j.clnesp.2022.01.016
Taiub A, Mohiuddin M, Guo D (2020) A randomized trial of ivermectin-doxycycline and hydroxychloroquine-azithromycin therapy on background
Tay MYF et al (2013) Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin. Antiviral Res 99(3):301–306. https://doi.org/10.1016/j.antiviral.2013.06.002
Troschel AS et al (2020) Computed tomography-based body composition analysis and its role in lung cancer care. J Thoracic Imaging 35(2):91–100. https://doi.org/10.1097/RTI.0000000000000428
Ufuk F et al (2020) The prognostic value of pneumonia severity score and pectoralis muscle area on chest CT in adult COVID-19 patients. Eur J Radiol 131:109271. https://doi.org/10.1016/j.ejrad.2020.109271
Vepa A et al (2020) COVID-19 and ethnicity: a novel pathophysiological role for inflammation. Diabetes Metabolic Syndrome 14(5):1043–1051. https://doi.org/10.1016/j.dsx.2020.06.056
Wagstaff KM et al (2012) Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J 443(3):851–856. https://doi.org/10.1042/BJ20120150
Wan X et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Xiao J et al (2020) Association of low muscle mass and low muscle radiodensity with morbidity and mortality for colon cancer surgery. JAMA Surg 155(10):942–949. https://doi.org/10.1001/jamasurg.2020.2497
Xie J et al (2020) Clinical characteristics of patients who died of coronavirus disease 2019 in China. JAMA Netw Open 3(4):e205619. https://doi.org/10.1001/jamanetworkopen.2020.5619
Acknowledgements
Not applicable.
Funding
No financial support was used in this study.
Author information
Authors and Affiliations
Contributions
AA collected de data and was a major contributor in writing the manuscript. MH was in charge of the conception and design of the work, MT analyzed and interpreted the patient data, MN participated in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In this study, written consent was obtained from the patients. All information was kept confidential, and all provisions of the Declaration of Helsinki were observed at every stage of the research.
Consent for publication
Patients were given permission to publish the results of the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmadzadeh Nanva, A., Haghighi-Morad, M., Taheri, M. et al. Association between thoracic density and area with COVID-19 outcomes. Egypt J Radiol Nucl Med 55, 63 (2024). https://doi.org/10.1186/s43055-024-01232-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01232-z