Abstract
Background
Because different gene receptors might cause each case of breast cancer, the disease is classified as a heterogeneous form because it can be subdivided into molecular subtypes. These molecular subtypes are different in disease manifestation, therapeutic response, and prognosis. Magnetic resonance imaging (MRI) has many applications in breast cancer's initial diagnosis and assessment of treatment response. The purpose of this research was to determine whether or not there is a correlation between specific morphological aspects of breast MRI in breast cancer and specific breast cancer subtypes and their impact on treatment decisions.
Results
There was an insignificant difference between different mass shapes and different molecular subtypes (P > 0.05). One hundred percent of triple-negative breast cancers (TNBC) were rounded. Molecular subtypes and the spiculated mass border diverged significantly statistically (P = 0.023). The percentage of the hormonal receptor (HR)-positive breast cancers with a spiculated border (80%) was greater than TNBC (0%) and distinctively different (P = 0.044). Surgical alternatives were observed to correlate significantly with the MRI mass border type (P = 0.030). There was an insignificant difference between molecular subtypes and tumor size (P = 0.602), lymph nodes (P = 0.283), multicentricity (P = 0.386), and curve type (P = 0.107).
Conclusions
MRI breast imaging has an important role in diagnostic and prognostic settings. The morphological results of MRI can be a helpful tool in distinguishing between the various subtypes of breast cancer. There was a statistically significant difference between different molecular subtypes and the spiculated mass border (P = 0.023). There was a statistically significant difference between the type of breast cancer surgery and the mass border (P = 0.030).
Similar content being viewed by others
Background
Breast cancer, often known as BC, is regarded as one of the most significant health issues in Egypt as well as the rest of the globe. It is the most frequent cancer in Egyptian women, accounting for 33 percent of all malignancies, and it is the second most common cause of cancer-related fatalities [1, 2].
On the basis of the expression of the estrogen receptor (ER), the progesterone receptor (PR), and the human epidermal growth factor receptor-2 (HER2), breast cancer molecular subtypes are classified as either luminal A, luminal B, HER2, or TNBC. Different illness manifestations, responses to treatment, and rates of patient survival are associated with each of these subtypes [3]. Patients with the luminal A subtype have the best prognosis, followed by patients with the luminal B subtype, who have a prognosis that falls somewhere in the middle, and finally the TN subtype, which is associated with a poor prognosis. There is a correlation between HER2-enriched subtypes and responsiveness to targeted therapy [4]. As a result, breast cancer is recognized as a distinct disease, and the practice of customized treatment is becoming increasingly common [5].
Differences in response to treatment and prognosis can occur between patients with breast cancer, as evidenced by the observed heterogeneity across patients and within individual tumors [6].
For the treatment of breast cancer, radiological diagnostic technologies that may anticipate how tumors will behave are becoming an increasingly important component [7]. Because it is possible to obtain high-resolution images based on morphological and functional characteristics using modern MRI technology, MRI is regarded as a potent instrument for the diagnosis of breast cancer. This is due to the fact that MRI may be used to do an assessment of the entire breast [6, 8].
In addition, MRI is a useful method for detecting breast cancer at an early stage, as other modalities like mammography and ultrasonography have low specificity and sensitivity. Early diagnosis of breast cancer becomes an effective key to successful treatment [9].
In addition to mammography and ultrasonography, the use of various MRI techniques has emerged as an essential adjunctive method [10]. Dynamic contrast enhancement (DCE) images, diffusion-weighted imaging (DWI), and other MRI sequences make up multi-parametric MRI, an indispensable imaging modality [11].
Studies on MRI's efficacy in diagnosing breast cancer have revealed a sensitivity of about 100%, although specificity varies depending on whether the morphological aspects or the enhancement pattern are being evaluated [12].
Breast MRI can be used for a wide variety of diagnostic and therapeutic purposes, including the detection of occult primary tumors and lymph nodes, the examination of nipple lesions and suspicious discharge, and the assessment of response to neoadjuvant therapy [13].
Lesions are categorized by the BI-RADS lexicon as foci, masses, and non-mass enhancement. The form, borders, and pattern of internal augmentation of masses allow for additional differentiation. Both the early and late stages of improvement are outlined so that a more accurate diagnosis may be made [14].
Unifocal breast cancer is defined as having only one separate lesion. Multicentric breast cancer is where two or more tumors are present in more than one quadrant of the same breast, or those separated by > 4–5 cm from each other. Multifocal breast cancer is defined as two or more tumors found in the same quadrant of the breast [15].
In order to better define prognosis and individualized treatment strategies for breast cancer patients, researchers have investigated the association between morphological and kinetic MRI findings and breast cancer subtypes [16, 17].
The purpose of this study was to establish whether or not the findings of MRIs can accurately predict the molecular subtypes of breast cancer. Specifically, we wanted to evaluate the link between certain morphological aspects of breast MRI in breast cancer and breast cancer subtypes and their impact on treatment decisions.
Methods
Our study was cross-sectional and observational with a single group at the Clinical Oncology, Radiodiagnosis, and General Surgery departments. Thirty women who had just received a true-cut biopsy diagnosis of invasive breast cancer were enrolled in the trial; their ages ranged from twenty-two to sixty-five years; and their stages ranged from I to III. Serum creatinine was tested and should be < / = 1.3 and GFR > 40. The study was from February 2021 to February 2023. An initial MRI breast examination was obtained for initial staging before any active treatment to assess the impact of MRI on treatment decisions. Patients whose ages are less than 18 years, pregnant, not pathologically proven breast cancer, patients contraindicated to gadolinium chelate contrast agents, metal items in patients, pacemakers, or Claustrophobia were excluded from our study.
MRI protocol
All of the breast MRI examinations were carried out using a high-field system that contained a 1.5-T magnetic resonance imaging system (Achieva; Philips Medical Systems, Best, The Netherlands) and a dedicated four-channel breast array coil. Each patient was positioned in a prone position. The pulse sequence parameters were as follows:
-
1.
T1-weighted gradient-echo MRI(5.5/2.7; flip angle 100; field of view, 360 mm; matrix, 480 * 480; section thickness, 2 mm; section gap, 1 mm).
-
2.
T2-weighted imaging (4684/130; echo train length, 15; field of view, 360 mm; matrix, 480 * 480; slice thickness, 2 mm; section gap, 0 mm).
-
3.
DCE axial T1-weighted imaging with fat suppression after an intravenous bolus injection of 0.1 mmol/kg gadolinium.
Sixteen years experienced radiologist interpreted MRI images.
Pathological molecular subtypes assessment
Molecular subtypes were determined depending on immunohistochemistry (IHC) for ER, PR, HER2 expression, and the Ki-67 index. Initial true-cut biopsy specimen sections were immunostained using a Ventana BenchMark GX autostainer. The Ventana UltraView DAB detection system was used. ER, PR, and HER2 were performed using the methodology outlined in the latest ASCO/CAP testing guidelines [18, 19].
If the HER2 IHC was 3 + , it was termed positive. If IHC was 2 + , the test was reflexed by fluorescence in situ hybridization. Cancers with 1%–100% of cells positive for ER and PR expression are considered HR (hormonal receptor) positive.
-
Luminal A subtype: ER- and/or PR-positive, HER2-negative, and Ki-67 < 20%.
-
Luminal B subtype: either ER- and/or PR-positive, HER2-negative, and Ki-67 ≥ 20%) or ER- and/or PR-positive and HER2-positive.
-
HER2-enriched type (HER2): ER- and PR-negative and HER2-positive.
-
Triple-negative type (TN): ER, PR, and HER2-negative [20].
Data collection
Medical records of patients were revised for history, physical examination, and initial breast sonomammography. Histopathology reports of the initial biopsy of the mass included pathological type, tumor grade, Ki-67%, and hormonal receptor status (ER, PR, Her 2 neu).
Ethical considerations
-
1.
Approving study: After receiving approval from the Committee of Clinical Oncology department, the study was also given permission to proceed by the ethics committee. The ethical approval code is MED-ONM027-1–21-2–138.
-
2.
Patient Consent: The purpose of the work, as well as its specifics, was explained to all of the participants in the current investigation, and each subject gave their informed consent to take part in the research in written form and for publication.
Data management and statistical analysis
The IBM Social Science Package (IBM SPSS) version 26 was used to collect, code, and modify the acquired data before entering it into the program. For the categorical variables, the data were given as numbers and percentages, and for the numerical variables, they were presented as means, standard deviations, and ranges according to the parametric distribution.
Results
Eleven (36.7%) patients had a unicentric tumor, while nineteen (63.3%) patients had a multicentric tumor. In terms of tumor size, two (6.7%) patients were T1, sixteen (53.3%) patients were T2, four (13.3%) patients were T3, and eight (26.7%) patients were T4. Twenty-five (83.3%) patients had positive lymph nodes. Regarding the lesion site, twenty (66.7%) patients had an upper quadrant lesion, fourteen (46.7%) patients had a lower quadrant lesion, and twelve (40%) patients had a central lesion. Four (13.3%) patients had a contralateral breast lesion. Five (16.7%) patients had a benign lesion. Regarding the mass shape, 15 (50%) patients had a rounded mass, 12 (40%) patients had an irregular mass, and only two (6.7%) patients had an oval one (Fig. 1). Nineteen (63.3%) patients had a spiculated mass border, eight (26.7%) patients had an irregular border, two (6.7%) patients had an angulated border, and only one (3.3%) patient had a well-defined border (Fig. 2). Twenty (66.7%) patients had a type 2 curve, nine (30%) patients had a type 3 curve, and only one (3.3%) patient had a type 1 curve (Table 1).
Molecular subtypes
Twenty (66.7%) patients were ER (estrogen receptor) positive; eighteen (60%) patients were PR (progesterone receptor) positive; twelve (40%) patients were HER2 (human epidermal growth factor receptor-2) positive; and only three (10%) patients were TNBC. For the tumor subtypes of 30 breast cancers, 15 (50%) were luminal A, 7 (23.3%) were luminal B, 5 (16.7%) were HR-HER2 + , and 3 (10%) were TNBC (Table 2).
There was an insignificant difference between different mass shapes and different molecular subtypes (P > 0.05); 100% of TNBC were rounded (Fig. 3), 46.7% of HR-positive tumors were irregular, 40% were rounded, and only 6.7% were oval. Forty-one and seven-tenths percent of HER-2-positive tumors were both rounded and irregular, while 6.7% were oval (Fig. 4). There was a difference that could be considered statistically significant between the various molecular subtypes and the hypothesized mass boundary (P = 0.023). Post hoc testing using Bonferroni correction was done to determine the nature of the difference between those subtypes. This analysis revealed that the percentage of HR-positive breast cancers with a spiculated border (80%) was greater than TNBC (0%); however, there is a major distinction (P = 0.044) (Figs. 5, 6). There was an insignificant difference between molecular subtypes and tumor size (P = 0.602), lymph nodes (P = 0.283) (Fig. 7), multicentricity (P = 0.386) (Figs. 8, 9), and curve type (P = 0.107) (Table 3).
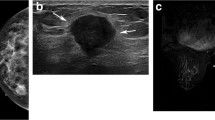
A 26-year-old female patient, presented clinically with right breast cancer. Initial MRI revealed: a unifocal mass in the lower outer quadrant of the right breast, round to oval shape, well-defined border, and infiltrating chest wall. Pathological analysis revealed: infiltrating duct carcinoma (IDC), grade (G) 2, TN subtype. a T1WI, b contrast-enhanced T1WI, c type I curve
A 58-year-old female patient, presented clinically with left breast cancer. Initial MRI revealed unifocal mass in lower outer quadrant of the left breast with irregular shape, speculated border and equivocal level I lymph nodes. Pathological analysis revealed IDC, G 2, ER + , PR + , HER 2 neu. a T2W1, b T1W1, c contrast-enhanced T1W1
A 41-year-old female patient, presented clinically with left breast cancer. Initial MRI revealed: unifocal mass in the upper inner quadrant of the left breast with an irregular shape, speculated border and pathological level I and II lymph nodes. Pathological analysis revealed IDC, grade (G) 2, ER + , PR + , and HER 2 neu + . a T2W1, b T1WI, c contrast-enhanced T1WI
A 43- year-old female patient, presented clinically with right breast cancer. Initial MRI revealed multicentric masses, rounded shape, irregular border, and mainly axillary tail mass infiltrating the chest wall. Pathological axillary lymph node infiltrating the lateral pectoral margins. Pathological analysis revealed IDC, G2, ER + , PR + , and HER 2 neu + . a T1WI, b contrast-enhanced T1WI, c type III curve
Regarding surgical treatment, twenty-one (72.4%) patients had MRM (modified radical mastectomy), and eight (27.6%) patients had BCS (breast conservative surgery). When comparing BCS with MRM, the mass border differed in a statistically significant way (P = 0.030): 3 patients (16.7%) of those with a speculated mass border were exposed to BCS, compared to 83.3% with MRM; 2 (25%) patients of those with an irregular mass border were exposed to BCS, compared to 75% with MRM; all patients with an angulated mass border had BCS, compared to nobody with MRM; and all patients with a well-defined mass border had BCS, compared to nobody with MRM. There was an insignificant difference between BCS and MRM regarding mass shape (P = 0.575) and multicentricity (P = 0.408) (Table 4).
Discussion
Breast cancer heterogenicity is related to the presence of a wide variety of molecular subtypes. Each molecular subtype has different phenotyping, risk factors, presentation, prognosis, therapeutic responses, and patient outcomes[10].
The aim of our study was the assessment of the morphological criteria of breast cancer lesions and their relation to molecular subtypes as a promising addition in the era of personalized medicine. Morphological features of breast lesions in breast MRI in our study included shape, border, multicentricity, tumor size, and lymph node status.
According to the BI-RADS lexicon, there are four possible categories for shape: round, oval, lobulated, and irregular. The outline of lobulated masses has an undulating quality. Irregular masses have an uneven shape that cannot be described as round, oval, or lobulated, and so the term "irregular" is applied to them [22].
In our study, 15 (50%) patients had a rounded mass, 12 (40%) patients had an irregular mass, and only two (6.7%) patients had an oval one. There was an insignificant difference between different mass shapes and different molecular subtypes (P > 0.05). One hundred percent of TN breast cancers were rounded. Forty-six and seven-tenths percent of HR (hormonal receptor) positive breast cancers were irregular, while 40% were rounded, and only 6.7% were oval. TN breast cancer is mostly presented and masked with benign morphological criteria, indicating a poor prognosis. These benign criteria may be explained by the rapid growth of the tumor, leading to central necrosis. Mohammed et al. [23] reported that TN tumors displayed a non-irregular shape more often than other tumors, such as a round, oval, or lobulated shape, with the round shape being the most common. However, the majority of lumen A and lumen B tumors are believed to be irregularly shaped. HER2-positive tumors typically take the shape of spherical lumps. The study of Du et al. [24] demonstrated significant differences in mass shape (P = 0.001) for molecular subtypes.
Regarding the margin of breast lesions in breast MRI scans, they can be described as smooth, uneven, or spiculated depending on their appearance. Spiculated margins are a common hallmark of malignant cancers of the breast [25]. Throughout this investigation, nineteen (63.3%) patients had a speculated mass margin, eight (26.7%) patients had an irregular margin, two (6.7%) patients had an angulated margin, and only one (3.3%) patient had a well-defined margin. Variations in molecular types and the predicted mass margin were statistically distinct (P = 0.023). We found that HR-positive breast cancers with a speculated border (80%) were greater than TNBC (0%), with a significant difference (P = 0.044). Consistent with Johnson et al. [5], who said that luminal A and B tumors often present with spiculated margins.
Boria et al. [26] also found that positive ER and PR expression was correlated with spiculated margins (P = 0.001), indicating a good prognostic factor. The study of Algazzar et al. [27]showed that when compared to HR-positive breast cancers, HR-negative breast tumors had a much higher likelihood of presenting with circumscribed margins (46.2% vs. 8.3%, respectively).
Not-circumscribed margins are mostly associated with luminal breast cancer, which is explained by the lack of desmoplastic reaction and the relatively slow growth rate [17].
As far as we're able to tell, in our study, we present the first evidence linking MRI mass border type with subsequent surgical intervention (P = 0.030). We found that 83.3% of patients with a speculated border underwent MRM, 75% with an irregular border underwent MRM, and all patients with a well-defined mass border underwent BCS. This may be explained by the attention of our surgeons to achieve a negative surgical margin.
One unanticipated finding in this study was that there was an insignificant difference between molecular subtypes and tumor size (P = 0.602), lymph nodes (P = 0.283), multicentricity (P = 0.386), and curve type (P = 0.107). A possible explanation for this might be the comparatively low number of individual patients participating in our study. This contradicted the findings of Galati et al. [28], who stated that the absence of axillary adenopathy was significantly associated with luminal A-like tumors which confirmed that this BC subtype is characterized by less aggressive behavior and a better prognosis. They also discovered a significant correlation between cancers with a luminal A subtype and lesion sizes smaller than 2 cm. Consistent with our results, they found no statistical association between tumor size assessed by MRI and other molecular subtypes.
In the study of Ozturk et al. [29], there was a significant difference in the frequency of axillary lymph node metastases among the various subtypes of breast cancer (P = 0.039). Although multifocality and multicentricity were observed more frequently in the luminal and HER2 ( +) subtypes than in the TN group, the difference did not meet the criteria for statistical significance, as indicated by our findings. In addition, the study could not find any statistically significant correlation between different molecular subtypes and tumor size (P = 0.14).
Youk et al. [30] study indicated that the node-positive rate was not different among subtypes in this study (P = 0.807), but tumor size was significant with them (P < 0.0001). Navarro et al. [31] evaluated MR imaging findings in molecular subtypes of breast cancer and found that tumor size and axillary lymph node positivity are not significantly correlated with molecular subtypes (P = 0.205, P = 0.474, respectively). Navarro et al. [31] also found that there were no statistically significant differences between the dynamic curve type in MRI and the different subtypes (P = 0.607). Unsimilar to our results, Algazzar et al. [27] found that HR-negative breast cancers were significantly associated with type III kinetic curves (p = < 0.001).
Limitations
However, our research had a few limitations. This is a single-center study that only had a limited number of participants overall. The study didn't include all possible patients, as they underwent excisional biopsy before MRI. Furthermore, the limited patient population made the distribution of molecular subtypes unbalanced. The cost of an MRI examination was high in our ongoing department. Finally, MRI images were evaluated by only one radiologist.
Conclusions
MRI morphological features could help in forecasting the molecular subtypes of breast cancer. There was a statistically significant difference between different molecular subtypes and the speculated mass border. There was a statistically significant difference between the type of breast cancer surgery and the mass border. Therefore, MRI breast imaging has an important role in diagnostic and prognostic settings. We may recommend incorporation in multicenter studies. We also recommend further research on the relationship between the findings of MRI and high-penetrance susceptibility genes in breast cancer in the era of radiogenomics and personalized medicine.
Availability of data and materials
Data will be available upon request via contacting the corresponding author.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- TNBC:
-
Triple-negative breast cancers
- HR:
-
Hormonal receptor
- BC:
-
Breast cancer
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor-2
- DCE:
-
Dynamic contrast enhancement
- DWI:
-
Diffusion-weighted imaging
- IDC:
-
Infiltrating duct carcinoma
- G:
-
Grade
References
Azim HA, Elghazawy H, Ghazy RM, Abdelaziz AH, Abdelsalam M, Elzorkany A, et al (2023) Clinicopathologic features of breast cancer in Egypt-contemporary profile and future needs: a systematic review and meta-analysis. Available from: https://ascopubs.org/go/authors/open-access
Abdelaziz A, Shawki M, Shaaban A, Albarouki S, Rachid A, Alsalhani O et al (2020) Breast cancer awareness among Egyptian women and the impact of caring for patients with breast cancer on family caregivers’ knowledge and behaviour. Res Oncol 22:1–8
Grimm LJ, Zhang J, Baker JA, Soo MS, Johnson KS, Mazurowski MA (2017) Relationships between MRI breast imaging-reporting and data system (BI-RADS) lexicon descriptors and breast cancer molecular subtypes: internal enhancement is associated with luminal B subtype. Breast J 23(5):579–582
Reig B, Heacock L, Geras KJ, Moy L (2020) Machine learning in breast MRI. J Magnet Reson Imag 52:998–1018
Johnson KS, Conant EF, Soo MS (2021) Molecular subtypes of breast cancer: a review for breast radiologists. J Breast Imag 3:12–24
Lee JY, Lee KS, Seo BK, Kyu RC, Cho R, Woo OH et al (2022) Radiomic machine learning for predicting prognostic biomarkers and molecular subtypes of breast cancer using tumor heterogeneity and angiogenesis properties on MRI. Eur Radiol 32:650–660. https://doi.org/10.1007/s00330-021-08146-8
Kitajima K, Yamano T, Fukushima K, Miyoshi Y, Hirota S, Kawanaka Y et al (2016) Correlation of the SUVmax of FDG-PET and ADC values of diffusion-weighted MR imaging with pathologic prognostic factors in breast carcinoma. Eur J Radiol 85(5):943–949
Yin H, Bai L, Jia H, Lin G (2022) Noninvasive assessment of breast cancer molecular subtypes on multiparametric MRI using convolutional neural network with transfer learning. Thorac Cancer 13(22):3183–3191
Alaref A, Hassan A, Sharma KR, Mishra R, Gautam J, Jahan N (2021) Magnetic resonance imaging features in different types of invasive breast cancer: a systematic review of the literature. Cureus 13(3):13854. https://doi.org/10.7759/cureus.13854
Li YZ, Huang YH, Su XY, Gu ZQ, Lai QQ, Huang J, Li ST, Wang Y (2022) Breast MRI segmentation and Ki-67 high- and low-expression prediction algorithm based on deep learning. Comput Math Methods Med 2022:1770531. https://doi.org/10.1155/2022/1770531
Huang Y, Wei L, Hu Y, Shao N, Lin Y, He S, Shi H, Zhang X, Lin Y (2021) Multi-parametric MRI-based radiomics models for predicting molecular subtype and androgen receptor expression in breast cancer. Front Oncol 11:706733. https://doi.org/10.3389/fonc.2021.706733
Caiazzo C, Di MR, Esposito E, Sollazzo V, Cervotti M, Varelli C, Forestieri P, Limite G (2018) The role of MRI in predicting Ki-67 in breast cancer: preliminary results from a prospective study. Tumori 104(6):438–443. https://doi.org/10.5301/tj.5000619
Wekking D, Porcu M, De SP, Saba L, Scartozzi M, Solinas C (2023) Breast MRI: clinical indications, recommendations, and future applications in breast cancer diagnosis. Curr Oncol Rep 25(4):257–267. https://doi.org/10.1007/s11912-023-01372-x
Mann RM, Cho N, Moy L (2019) Breast MRI: state of the art. Radiology 292(3):520–536. https://doi.org/10.1148/radiol.2019182947
Zhang Y, Liu F, Gao Q, Chai Y, Ren Y, Tian H, Ma B, Song A (2022) Comparing the outcome between multicentric/multifocal breast cancer and unifocal breast cancer: a systematic review and meta-analysis. Front Oncol 12:1042789. https://doi.org/10.3389/fonc.2022.1042789
Kazama T, Takahara T, Hashimoto J (2022) Breast cancer subtypes and quantitative magnetic resonance imaging: a systemic review. Life (Basel, Switzerland) 12(4):490. https://doi.org/10.3390/life12040490
Galati F, Trimboli RM, Pediconi F (2021) Special issue advances in breast MRI. Diagnostics 11(12):2297. https://doi.org/10.3390/diagnostics11122297
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, Hayes DF, Lakhani SR, Chavez-MacGregor M, Perlmutter J, Perou CM, Regan MM, Rimm DL, Symmans WF, Torlakovic EE, Varella L, Viale G, Weisberg TF, McShane LM, Wolff AC (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38(12):1346–1366. https://doi.org/10.1200/JCO.19.02309
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, Jenkins RB, Press MF, Spears PA, Vance GH, Viale G, McShane LM, Dowsett M (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American pathologists clinical practice guideline focused update. J Clin Oncol 36(20):2105–2122. https://doi.org/10.1200/JCO.2018.77.8738
Szymiczek A, Lone A, Akbari MR (2021) Molecular intrinsic versus clinical subtyping in breast cancer: a comprehensive review. Clin Genet 99(5):613–637. https://doi.org/10.1111/cge.13900
Hortobagyi GN, Connolly JL, D’Orsi CJ, Edge SB, Mittendorf EA, Rugo HS, et al (2017) Breast. In: AJCC cancer staging manual. Springer International Publishing, Cham, pp 589–636. https://doi.org/10.1007/978-3-319-40618-3_48
Meyer-Base A, Morra L, Tahmassebi A, Lobbes M, Meyer-Base U, Pinker K (2021) AI-enhanced diagnosis of challenging lesions in breast MRI: a methodology and application primer. J Magnet Reson Imaging: JMRI 54(3):686–702. https://doi.org/10.1002/jmri.27332
Mohammed EA, Tharwat M, Solyman M, Nabil Omar N, Mohamed N, Hasan A (2022) Imaging features of breast cancer molecular subtypes: an updated review of the Literature. vol 5, SVU-IJMS
Du S, Gao S, Zhang L, Yang X, Qi X, Li S (2021) Improved discrimination of molecular subtypes in invasive breast cancer: comparison of multiple quantitative parameters from breast MRI. Magn Reson Imaging 77:148–158. https://doi.org/10.1016/j.mri.2020.12.001
Erguvan-Dogan B, Whitman GJ, Kushwaha AC, Phelps MJ, Dempsey PJ (2006) BI-RADS-MRI: a primer. AJR Am J Roentgenol 187(2):W152–W160. https://doi.org/10.2214/AJR.05.0572
Boria F, Tagliati C, Baldassarre S, Ercolani P, Marconi E, Simonetti BF, Santinelli A, Giuseppetti GM (2018) Morphological MR features and quantitative ADC evaluation in invasive breast cancer: correlation with prognostic factors. Clin Imaging 50:141–146. https://doi.org/10.1016/j.clinimag.2018.02.011
Algazzar MA, Elsayed EE, Alhanafy AM, Mousa WA (2020) Breast cancer imaging features as a predictor of the hormonal receptor status, HER2neu expression and molecular subtype. Egypt J Radiol Nuclear Med 51(1)
Galati F, Rizzo V, Moffa G, Caramanico C, Kripa E, Cerbelli B, D’Amati G, Pediconi F (2022) Radiologic-pathologic correlation in breast cancer: do MRI biomarkers correlate with pathologic features and molecular subtypes? Eur Radiol Exp 6(1):39. https://doi.org/10.1186/s41747-022-00289-7
Öztürk VS, Polat YD, Soyder A, Tanyeri A, Karaman CZ, Taşkın F (2020) The relationship between MRI findings and molecular subtypes in women with breast cancer. Curr Probl Diagn Radiol 49(6):417–421. https://doi.org/10.1067/j.cpradiol.2019.07.003
Youk JH, Son EJ, Chung J, Kim JA, Kim EK (2012) Triple-negative invasive breast cancer on dynamic contrast-enhanced and diffusion-weighted MR imaging: comparison with other breast cancer subtypes. Eur Radiol 22(8):1724–1734. https://doi.org/10.1007/s00330-012-2425-2
Navarro Vilar L, Alandete Germán SP, Medina García R, Blanc García E, Camarasa Lillo N, Vilar Samper J (2017) MR imaging findings in molecular subtypes of breast cancer according to BIRADS system. Breast J 23(4):421–428. https://doi.org/10.1111/tbj.12756
Acknowledgements
Not applicable.
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
ST and MM gave the idea, collected the patients’ data, and analyzed them as well as wrote the manuscript with revision. SA contributed to the evaluation of radiological findings and revised the results and manuscript. MY analyzed and interpreted the patients’ data regarding the surgical aspects. ME shared in manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical committee of the Faculty of Medicine, South Valley University. The ethical approval code is SVU-MED-ONM027-1–21-2–138. Data were collected after obtaining informed written consent from all cases.
Consent for publication
Each patient gave their informed consent to take part in the research in written form.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Temerik, S.M., Elwahab, S.M.A., Wahman, M.M. et al. Relation between morphological features of initial breast MRI and breast cancer molecular subtypes. Egypt J Radiol Nucl Med 54, 147 (2023). https://doi.org/10.1186/s43055-023-01087-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01087-w