Abstract
Background
Owing to significant morbidity and mortality with the development of vascular complications in patients with acute invasive fungal rhinosinusitis (AIFRS), early identification, and rapid medical or surgical interventions that are essential for improving patients’ outcomes. For the purpose of presurgical mapping and management planning, magnetic resonance imaging (MRI) is essential for the early identification and improved delineation of disease extent.
Objective
To evaluate variable MRI manifestations in the detection of the vascular complications in patients with AIFRS and its impact on patients’ survival.
Methods
A retrospective study, included 24 patients with histopathological proven AIFRS to review the para nasal sinus MRI findings. MRI were evaluated for the sinus involvement and the extrasinus extension into the orbit and/or the brain. Vascular structures were assessed for the development of vascular complications, like ICA for thrombosis, attenuation or pseudoaneurysm, cavernous sinus and superior ophthalmic veins for thrombosis.
Results
Of the reviewed 24 patients, 16 had cavernous sinus thrombosis, 15 had ICA thrombosis, 10 had ophthalmic vein thrombosis, 4 had ICA attenuation and only two cases had pseudoaneurysm of the ICA. Vascular thrombosis was more common with mucormycosis with cavernous sinus and ophthalmic vein thrombosis which were significantly increased among non survivor patients (90%, 70%), as compared to the survivor patients (50%, 14.29%), with P = 0.04 and 0.005 respectively.
Conclusions
Vascular complications are common in patients with AIFRS. MRI is helpful in accurate detection of vascular complications in patients with AIFRS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Acute invasive fungal rhinosinusitis (AIFRS) is among the most severe illnesses that have reemerged in the COVID-19 era [1]. It is a rare and severe disease that primarily affects people who are immunocompromised. Neutropenia represents a significant risk factor specially in hematological malignancies [2].
The Acute invasive fungal rhinosinusitis is the worst type of fungal sinusitis, due to its high mortality [3]. Owing to significant morbidity and mortality with the development of vascular complications in patients with AIFRS, early identification, and rapid medical or surgical interventions are essential for improving patients’ outcomes [4].
Aspergillus and zygomycetes (rhizopus, mucor, and rhizomucor) are among the most often found fungi in AIFRS [5, 6]. Mucor has an angioinvasive characteristic, causing extensive tissue necrosis, severe mortality of about 50 to 80%, and high morbidity in patients who survive [7].
In computed tomography (CT), osseous erosions and extra-sinonasal extension which are suggestive of an invasive nature, are late features with restricted treatment window [8, 9].
In contrast, it has been shown that MRI is more sensitive in early detection of AIFRS [10]. Contrast enhanced T1WI with fat saturation are better for the evaluation of intracranial spread and development of vascular complications [11, 12]. The vascular manifestations include vascular mural thickening and enhancement, intraluminal arterial thrombosis, and dural venous sinus thrombosis [13].
Infection of ethmoid sinus entails a significant risk of extension of the inflammation into orbital apex, and cavernous sinus thrombosis. Another possibility is direct disease dissemination into the orbital apex with involvement of sphenoid sinus [14, 15].
Vascular complications in AIFRS are linked to significant morbidity and mortality. The sole means of reducing morbidity and improving patient outcomes are prompt diagnosis and urgent medical and surgical interventions. MRI is essential in the diagnosis and delineation of the disease extent [16].
This study purpose was to assess the MRI value in the early identification of vascular complications in patients with AIFRS and the effects of this early detection on patients’ outcomes.
Methods
This is an Institutional Review Board (IRB) approved retrospective study, with registration number 00412/2022, that was carried out on 32 patients, admitted to the radiology department from January 2021 to December 2021, their ages ranged between 40 and 65 years, eight patients have been excluded from the study as they underwent surgical debridement before doing MRI examination, the remaining 24 patients (12 males and 12 females) have been classified into 2 groups, based on the pathological findings, Group I that comprised 13 patients with mucormycosis, and Group II that comprised 11 patients with aspergillosis (Fig. 1). All the patients underwent paranasal sinus MRI. Follow up of the patients was done clinically for the next 4weeks.
Patients included in this study had immunocompromise states. The patients had clinical features suggestive of acute invasive fungal sinusitis, in addition to clinical features suspecting development of vascular complications such as neurological deficits, ophthalmoplegia, chemosis, vision loss, and involvement of the maxillary (V2) and mandibular (V3) divisions of trigeminal nerve, third or fourth cranial nerves.
All the patients were pathologically confirmed to have acute invasive fungal rhinosinusitis and underwent MRI evaluation.
Patients who performed surgical debridement before doing MRI evaluation, patients who are immunocompetent, who did not have clinical features suggesting vascular complications of invasive fungal sinusitis and patients who did not undergo MRI evaluation or the MRI studies were significantly degraded due to motion were excluded.
All included patients in our study were reviewed as regard to the following: patients’ demographics, clinical data, surgical type (endoscopic surgical debridement, or combined), pathology confirmation of the pathogen (mucormycosis, versus aspergillosis), presence of COVID-19, and patients’ survival.
The MRI was performed on 1.5T MRI Scanner (Optima 450 W GEM suite MRI; GE Healthcare, Seattle, Washington, USA) using an eight-channel head coil. Multiplanar, Multi Echo MRI of the paranasal sinuses’ sections were acquired.
For anatomical assessment and signal characterization, the sinus protocol included axial T1WI, axial and coronal T2WI fat-saturated sequences. Diffusion-weighted imaging (DWI) was obtained with b value of 0, and 1000 mm2/sec. To distinguish true diffusion from such pitfalls as T2 shine through, the apparent diffusion coefficient (ADC) maps were automatically generated. ADC value of all cases reported was determined in ADC map considering a 5 cm region of interest (ROI) as central as possible and in the most significant part of the vascular complication. ROI was manually positioned in full concordance with 3 observers with experience in sinonasal evaluation by MRI. Mean ADC values generated by the ROIs in each ADC map positioning was addressed to the respective case report. With the exception of four individuals with compromised renal function, postcontrast fat-saturated T1WIs were obtained 20–30 s after intravenous injection of 0.1 mmol/kg of gadopentetate dimeglumine (Magnevist; Schering, Berlin, Germany), injected manually at a rate of 2 mL/sec. The orbit cuts were covered in the field of view. To detect intracranial extension, axial T2WI, axial Fluid-attenuated inversion recovery (FLAIR), and postcontrast T1WI fat-saturated sequences of the whole brain were obtained. Imaging parameters are shown in (Table 1).
Experienced two neuroradiologists, with 10 and 5 years of experience, separately and blinded from the patients' clinical data and pathological findings assessed MR images on a workstation using Horos DICOM viewer. The sinuses were evaluated separately to determine the extent and site of disease i.e., maxillary, frontal, sphenoid, anterior and posterior ethmoid sinuses, and side of disease involvement i.e., right, left, or bilateral. Then each subsite has been evaluated for the presence of: mucosal thickening, and enhancement, signal of the sinus contents on T1 and T2WIs, and signal on diffusion weighted imaging. Special attention was paid for the involvement of the sinonasal walls, and periantral fat spaces. Pre- and post-septal cellulitis were observed as the spread into the orbit; post-septal cellulitis is often characterized by soft tissue stranding posterior to the orbital septum with varying degrees of proptosis. DWI sequence, which displays restricting wall and the endocavitary projections, sparing the lesion core, is high specific for fungal abscess. Vascular structures were assessed carefully to determine development of vascular complications. The ICA involvement has been determined according to the following findings: ICA attenuation which is noted as mural thickening, luminal narrowing and enhancement of the vessel wall on black blood postcontrast T1WIs fat-saturated images. Evaluation of the ICA also included determination of the presence of intraluminal thrombosis, seen as lack of signal void on T2 WI or filling defects on contrast enhanced sequence; and the development of ICA pseudoaneurysm. Cavernous sinus has been evaluated for the presence of thrombosis which manifests as changes in the size, contour, the signal intensity of cavernous sinus as well as the increased dural enhancement along the cavernous sinus lateral border. Other vascular issues such as ophthalmic vein thrombosis was evaluated, and it may manifest as a dilated intra-orbital cord-like structure above the optic nerve with loss of the normal flow void in the thrombosed vein.
Statistical Package for the Social Sciences (SPSS) (version 21) (SPSS Inc.- Chicago, IL) was used to compile and analyze our data. Age and other continuous variables are shown as means (± deviation [SD]), and percentages and relative frequency distributions are used to present categorical variables. To test for normality, the Shapiro–Wilk test was used. As a result, the Mann–Whitney (t) test or the Student's t-test were used to compare the continuous variables. The Chi-squared test (X2) was performed to determine the percentage of participants with opacification for categorical variables (e.g., sex, vascular complications, surgery type, COVID-19 status, and mortality). To determine whether there was a difference between any two groups that was statistically significant, the one-way ANOVA (F) test was utilized. The threshold for the statistical significance was set at p ≤ 0.05.
Results
The 32 patients with histopathological proven Acute invasive fungal rhinosinusitis (AIFRS) had different symptoms such as facial pain or loss sensation, visual loss, nasal congestion, epistaxis, cavernous sinus thrombosis and cranial nerve involvement, history of other comorbidities, like COVID-19 (was the risk factor in 54.17% of the cases) and other immunocompromise states like diabetes mellitus, complete clinical examination, laboratory and histopathological findings were collected and analyzed retrospectively. The mean age of the patients was 54.67 ± 5.26 years, and half of them were males (12 patients, 50%). There was no significant correlation between surgical types nor presence of COVID-19 with age and sex among the studied groups (P = 0.895) (Table 2).
Involvement of the bilateral maxillary, sphenoid, ethmoid sinuses were most frequent among patients with mucormycosis by 23.08% of mucormycosis cases. While the right maxillary and sphenoid sinuses were the most frequently involved among patients with aspergillosis by 18.18% of aspergillosis cases, with a significant level of 0.023 (Fig. 2).
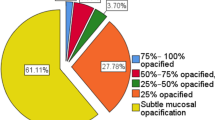
The degree of paranasal sinus mucosal disease ranged between subtle mucosal thickening (15%), sinus opacification (75%), sinus opacification and expansion (10%). The sinus contents showed T1WI intermediate to hypointense signal, T2WI variably hyperintense signal with fungal hyphae of hypointense signal, associated with fluid or hemorrhagic changes in 12% of cases. Fat suppressed post contrast enhanced T1WI showed loss of normal sinus mucosal enhancement “denoting necrosis” (55%), enhancing extra-sinus soft tissue (70%). Some cases showed peripheral mucosal enhancement. In most cases (90%) the sinus contents showed restricted diffusion on DWI. All cases showed variable degrees of extra-sinus extension to different anatomical zones, to the pterygopalatine fossa (64%), periantral fat (preantral and retromaxillary) (92%), to the orbit as postseptal cellulitis (44%), and to the brain as meningitis and cerebritis (35%).
Out of the mentioned 13 cases of mucormycosis; 4 (33.33%) cases had ICA attenuation, 8 (61.54%) cases had ICA thrombosis, only one (7.69%) case had ICA pseudoaneurysm, 7 (53.85%) cases had cavernous sinus thrombosis and 4 (33.33%) cases had ophthalmic vein thrombosis.
Out of the mentioned 11 cases of aspergillosis; no (0%) cases had ICA attenuation, 7(63.64%) cases had ICA thrombosis, only one (1.09%) case had ICA pseudoaneurysm, 9 (81.82%) cases had cavernous sinus thrombosis and 5 (45.45%) cases had ophthalmic vein thrombosis.
Regarding the vascular complications, involvement of the ICA was noticed in 21 out of 24 cases; 15 cases had ICA thrombosis (Fig. 3), 4 cases had ICA attenuation while only two cases had ICA pseudoaneurysm (Fig. 4), and the cavernous sinus thrombosis was reported in 16 out of 24 cases (Fig. 5), while the superior ophthalmic vein thrombosis was noticed in 9 out of 24 cases (Fig. 6). Combined involvement of both cavernous sinus and ICA thrombosis, cavernous sinus and superior ophthalmic vein thrombosis was noticed in 10 cases for each (Fig. 7). The ICA attenuation was found in patients with mucormycosis by (33.33%), with a significant difference (P = 0.044). While there was no significant correlation between pathology findings with ICA thrombosis, pseudo aneurysm, cavernous sinus thrombosis, ophthalmic vein thrombosis, surgery types,
A 46-year-old female patient presenting after 2 weeks of COVID-19 infection with AIFS, histopathological proven to be mucormycosis. A, B axial T2W MRIs revealed loss of the signal void in the cavernous segment of the left ICA denoting thrombosis. C coronal T2WI, D coronal contrast enhanced T1W MRI showed left superior ophthalmic vein thrombosis (orange arrow), enhancing left intra-orbital soft tissue infiltration (white arrow), mucosal thickening of left maxillary sinus and left inferior nasal turbinectomy. E, F axial non-contrast enhanced T1W MRIs with fat suppression showed thrombosis of the petrous and cavernous segments of the left ICA. G, H axial contrast enhanced T1W MRIs with fat suppression showed heterogenous enhancement of the left ICA thrombosis. I DW MRI, J ADC map revealed mild restricted diffusion at the left ICA thrombosis
A 41-year-old male patient presenting with AIFS, histopathological proven to be aspergillosis. A axial, B coronal T2W MRIs revealed pseudoaneurysmal dilatation in the cavernous segment of the right ICA, right spheno ethmoidal sinusitis. C axial non-contrast enhanced T1W MRI revealed hypointense signal within the pseudoaneyrysm. D axial contrast enhanced T1W MRI with fat suppression showed partial heterogenous enhancement of the ICA pseudoaeurysm denoting partial thrombosis. E DW MRI, F ADC map revealed free diffusion at the right ICA pseudoaneurysm
A 45-year-old male patient presenting with AIFS, histopathological proven to be aspergillosis. A, B axial T2W MRIs revealed left ICA and left cavernous sinus thrombosis (orange arrow), fungal sphenoid sinusitis (yellow arrow) and soft tissue infiltration of the left upper eyelid by extension along the left ophthalmic nerve (white arrow). C coronal T2W MRI showed left ophthalmic nerve involvement (arrow), left middle and inferior nasal turbinectomy. D axial non-contrast enhanced T1W MRI revealed loss of the signal void within the left ICA and left cavernous sinus denoting thrombosis. E DW MRI, F ADC map revealed restricted diffusion at the left cavernous sinus thrombosis
A 53-year-old female patient presenting after 3 weeks of COVID-19 infection with AIFS, histopathological proven to be mucormycosis. A axial T2WI, B coronal T2W MRI revealed thrombosis in the cavernous segment of the right ICA (orange arrow) and thrombosis in the right superior ophthalmic vein (yellow arrow), right posterior ethmoid sinusitis. C axial non-contrast enhanced T1W MRI revealed loss of the signal void within the right ICA cavernous segment denoting thrombosis. D DW MRI, E ADC map revealed restricted diffusion at the right ICA and right superior ophthalmic vein thrombosis
A 62-year-old female patient presenting with AIFS, histopathological proven to be mucormycosis. No history of COVID-19 infection. A axial T2WI, B, C coronal T2W MRIs revealed thrombosis in the cavernous segment of the left ICA, left cavernous sinus thrombosis and left superior ophthalmic vein thrombosis, left sphenoid sinusitis and bilateral middle and inferior nasal turbinectomy. D DW MRI, E ADC map revealed restricted diffusion at the left ICA thrombosis
COVID-19, and mortality (P = 0.774) (Table 3). Cavernous sinus thrombosis and ophthalmic vein thrombosis were significantly increased among non-survivor patients (90.00%, 70.00%), as compared to survivor patients (50.00%, 14.29%) respectively, with P = 0.04 and 0.005 respectively (Table 4). We did not find statistically significant correlation of the other involved vascular structures to the patient’s survival.
There was no significant correlation between surgical types with vascular complications, COVID-19, and mortality (P > 0.05). Likewise, there was no significant relation between COVID-19 with vascular complications (p > 0.05), and mortality (p = 0.188) among the studied patients (Table 5).
There was an almost perfect inter-observer agreement between the two expert neuroradiologists (Fleiss’ K with 95% confidence interval).
Discussion
The vascular complications in AIFRS are the most terrifying ones because they are associated with high morbidity and mortality rates, as vascular invasion by fungi can result in hemorrhagic or ischemic strokes with cerebral infarction calling for increased awareness. It is important to recognize these issues as joint surgical and medical emergencies [17].
This study purpose was to assess the MRI value in the early identification of vascular complications in patients with AIFRS and the effects of this early detection on patients’ outcomes.
In our study, regarding ICA complications, we found that ICA thrombosis was the most frequent ICA complication (71.4% of the cases), the cavernous sinus thrombosis and ophthalmic vein thrombosis were significantly increased among the non survivor patients, as compared to the survivor patients. Other vascular complications did not have significant correlation with mortality of studied groups. There is a significant propensity for the arterial invasion in mucorales' infection [18, 19]. Cavernous sinus thrombosis is a fatal condition that may call for a neurosurgeon's assistance. It frequently results from a hematogenous spread. It often becomes involved because of how close it is to the sphenoid sinus [20].
The least frequent ICA complication was found to be ICA pseudoaneurysm, representing only 9.5% of the cases. A small number of cases of the uncommon mycotic aneurysms have been documented thus far. They virtually always result in death, with high fatality rates ranging from 85 to 100%. The aspergillus fungus is mostly the cause. They have a propensity of invading blood vessels, resulting in aneurysmal dilatations, cerebral infarction, subarachnoid haemorrhage, and eventually death [21].
The present study showed that, mucormycosis pathology was more common among the studied patients (n = 13, 54.17%), than aspergillosis (n = 11, 45.83%) with a borderline significant difference (P = 0.050). Our study was close to the study of Shaban et al. [22] who found that the most isolated fungal pathogens were Mucor species (77.8%), followed by the aspergillus fumigatus (22.4%). Raab et al. [23] noted, Aspergillus spp. can also cause invasive fungal sinusitis, making Mucorales not the only fungal pathogens that can infect the paranasal sinuses.
In our study the mortality rate was 41.66% and the survival rate was 58.33% which are comparable with the findings of Shaban et al. [22] where the overall mortality was 40.7%, and also comparable with the findings of Turner et al. [5] who reported overall survival rate of 49.7%, and Allensworth et al. [24] who reported a survival rate of (68%) that was nearly identical to that reported in Malleshappa et al. [25] which stated an overall survival rate of 68.2%.
This study had some limitations, first, it was a single institutional study with a retrospective study design, second, lack of data in the literature discussing the entity of vascular complications in AIFRS, also the contraindication to contrast material injection in some patients, limits the optimal evaluation of vascular structures in those patients. Finally, there were only limited long-term clinical outcomes available.
Conclusions
Mortality of AIFRS is still high in spite of improvements in medical and surgical treatment. COVID-19 is a major risk factor of getting AIFRS. Contrast-enhanced MRI plays a crucial role in detecting and diagnosing AIFRS, assessing the extent of involvement, guiding treatment protocols, predicting and identifying the complications especially, the vascular complications that are common and devastating complications in AIFRS patients with higher risk morbidity and mortality.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIFRS:
-
Acute invasive fungal rhinosinusitis
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MSCT:
-
Multi-slice computed tomography
- ICA:
-
Internal carotid artery
- DWI:
-
Diffusion weighted imaging
- ADC:
-
Apparent diffusion coefficient
- ROI:
-
Region of interest
- FLAIR:
-
Fluid-attenuated inversion recovery
- SPSS:
-
Statistical Package for the Social Sciences
References
Nagesh CP (2021) The “black fungus” through a gray lens: Imaging COVID-19-associated mucormycosis. Indian J Ophthalmol 69(7):1648–1649. https://doi.org/10.4103/IJO.IJO_1506_21
Chen CY, Sheng WH, Cheng A et al (2022) Invasive fungal sinusitis in patients with hematological malignancy: 15 years experience in a single university hospital in Taiwan. BMC Infect Dis. https://doi.org/10.1186/1471-2334-11-250
Jiang N, Zhao G, Yang S et al (2016) A retrospective analysis of eleven cases of invasive rhino-orbito-cerebral mucormycosis presented with orbital apex syndrome initially. BMC Ophthalmol. https://doi.org/10.1186/s12886-016-0189-1
Gavito-Higuera J, Mullins CB, Ramos-Duran L et al (2016) Sinonasal fungal infections and complications: a pictorial review. J Clin Imag Sci. https://doi.org/10.4103/2156-7514.184010
Turner JH, Soudry E, Nayak JV et al (2013) Survival outcomes in acute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope 123(5):1112–1118. https://doi.org/10.1002/lary.23912
Monroe MM, Mclean M, Sautter N et al (2013) Invasive fungal rhinosinusitis: a 15-year experience with 29 patients. Laryngoscope 123(7):1583–1587. https://doi.org/10.1002/lary.23978
Nair AG, Adulkar NG, D’Cunha L et al (2021) Rhino-orbital mucormycosis following COVID-19 in previously non-diabetic, immunocompetent patients. Orbit 40(6):499–504. https://doi.org/10.1080/01676830.2021.1960382
Delgaudio JM, Swain RE, Kingdom TT et al. (2003) Computed tomographic findings in patients with invasive fungal sinusitis. Available from https://jamanetwork.com/. (Online)
Howells RC, Ramadan HH (2001) Usefulness of computed tomography and magnetic resonance in fulminant invasive fungal rhinosinusitis. Am J Rhinol 15(4):255–261
Lagos AE, García-Huidobro FG, Sepúlveda V et al (2021) Determination of variables for a more accurate diagnostic approach in suspected acute invasive fungal rhinosinusitis: a non-concurrent cohort study. Clin Otolaryngol 46(4):775–781. https://doi.org/10.1111/coa.13734
Mathur S, Karimi A, Mafee MF (2007) Acute Optic Nerve Infarction Demonstrated by Diffusion-Weighted Imaging in a Case of Rhinocerebral Mucormycosis. Available from www.ajnr.org. (Online)
Mohindra S, Mohindra S, Gupta R et al (2007) Rhinocerebral mucormycosis: the disease spectrum in 27 patients. Mycoses 50(4):290–296. https://doi.org/10.1111/j.1439-0507.2007.01364.x
Idowu OO, Soderlund KA, Laguna B et al (2022) Magnetic resonance imaging prognostic findings for visual and mortality outcomes in acute invasive fungal rhinosinusitis. Ophthalmology 129(11):1313–1322. https://doi.org/10.1016/j.ophtha.2022.06.020
Sreshta K, Dave TV, Varma DR et al (2021) Magnetic resonance imaging in rhino-orbital-cerebral mucormycosis. Indian J Ophthalmol 69(7):1915–1927. https://doi.org/10.4103/ijo.IJO_1439_21
Agrawal A, Tripathi PS, Shukla P et al (2022) Intracranial manifestations of rhinocerebral mucormycosis: a pictorial essay. Egypt J Radiol Nucl Med. https://doi.org/10.1186/s43055-022-00765-5
de Moura FL, Altemani A, Adolfo da Silva N et al (2019) Teaching neuroimages: mucormycosis-associated vasculitis: a new sequence to show an old invasive infection. Neurology 92(15):e1796–e1797. https://doi.org/10.1212/WNL.0000000000007275
Sharma RR, Sharma A (2016) Paranasal invasive fungal sinusitis and its central nervous system complications: current understanding and their management. Austin J Otolaryngol 3(2):1077
John TM, Jacob CN, Kontoyiannis DP (2021) When uncontrolled diabetes mellitus and severe covid-19 converge: the perfect storm for mucormycosis. J Fungi. https://doi.org/10.3390/jof7040298
Pai V, Khan I, Sitoh YY et al (2020) Pearls and pitfalls in the magnetic resonance diagnosis of dural sinus thrombosis: a comprehensive guide for the trainee radiologist. J Clin Imaging Sci 10:77. https://doi.org/10.25259/jcis_187_2020
Rathore A, Shah NJ (2009) Intracranial extension of fungal sinusitis. Int J Otorhinolaryngol Clin 1(1):55–62. https://doi.org/10.5005/jp-journals-10003-1008
Ahsan H, Ajmal F, Saleem MF et al (2009) Cerebral fungal infection with mycotic aneurysm of basilar artery and subarachnoid haemorrhage. Singap Med J 50(1):E22–E25
Shaban E, Saleh RA, Ammar MI et al (2022) Post-COVID-19 acute invasive fungal rhinosinusitis: a systematic radiological approach in the light of clinico-surgical characteristics. Egypt J Radiol Nucl Med. https://doi.org/10.1186/s43055-022-00880-3
Raab P, Sedlacek L, Buchholz S et al (2017) Imaging patterns of rhino-orbital-cerebral mucormycosis in immunocompromised patients: when to suspect complicated mucormycosis. Clin Neuroradiol 27(4):469–475. https://doi.org/10.1007/s00062-017-0629-1
Allensworth JJ, Troob SH, Weaver TS et al (2021) Secondary free-flap reconstruction following ablation for acute invasive fungal sinusitis. Laryngoscope 127(4):815–819. https://doi.org/10.1002/lary.26298
Malleshappa V, Rupa V, Varghese L et al (2020) Avoiding repeated surgery in patients with acute invasive fungal sinusitis. Eur Arch Otorhinolaryngol 277(6):1667–1674. https://doi.org/10.1007/s00405-020-05879-y
Acknowledgements
Not applicable.
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
HSA: Conceptualization and Data curation: SA, Formal analysis: SA, AN, HAA Investigation: SA, HA Formal analysis SA, AY, AN, Methodology: SA, Project administration and resources: SA, AN, Software: SA, Supervision: SA, Validation and Visualization: SA, AY, AN, writing original draft: SA, HAA Writing review, revised & editing: SA, AY, AN. “All authors read and approved the final manuscript”.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Institutional Review Board (IRB)” of National Liver Institute Menoufia University and with the Helsinki Declaration of 1964 and later versions. Committee’s reference number is (00412/2022). No consent was obtained from the patients since it was a retrospective study.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abokoura, S., Youssef, A., Nada, A. et al. Magnetic resonance imaging manifestations of vascular complications in patients with acute invasive fungal rhinosinusitis. Egypt J Radiol Nucl Med 54, 133 (2023). https://doi.org/10.1186/s43055-023-01081-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01081-2