Abstract
Background
Hydatid disease is a parasitic infection which is endemic in multiple regions across the globe including Indian subcontinent. Although it commonly affects the liver and other solid organs, isolated involvement of the heart is relatively uncommon. Cardiac hydatidosis can be confidently diagnosed on echocardiography, but cross-sectional imaging by computed tomography (CT) or magnetic resonance imaging (MRI) provides accurate information about its location, extent, and multiplicity. Multiple case studies of cardiac hydatid disease have been reported in the literature. However, cardiac hydatidosis with extension into pulmonary vasculature has not been reported commonly. This case report highlights this rare association, with stress upon the altered surgical management.
Case presentation
A 50-year-old patient presented with atypical chest pain to the cardiology department of a tertiary care hospital where he underwent multiple blood tests as well as electrocardiography (ECG) and echocardiography as part of the routine examination. Echocardiography revealed a large, multicystic mass invading the posterolateral wall of left ventricle (LV) with no internal vascularity and was provisionally diagnosed as hydatid disease. Subsequent CT study confirmed a large multicystic lesion with the presence of another smaller lesion invading the left atrial appendage (LAA). In order to evaluate the vascular and mediastinal invasion, cardiac MRI was then performed which revealed invasion of right pulmonary artery (PA), right superior pulmonary vein (PV) as well as compression of superior vena cava (SVC) by the smaller lesion. A final diagnosis of cardiac hydatidosis with invasion into right PA and right superior PV was made. Treatment plan for the patient changed, who then underwent an additional reconstruction of right PA and right superior PV after cyst removal.
Conclusions
Cardiac hydatid disease is a rare but potentially lethal condition, which tends to show slow growth and local invasion. The diversity of findings in such rare cases makes individual surgical approach extremely valuable with preoperative radiological imaging becoming indispensable for correct localization and appropriate planning. Our case report highlights rare association of cardiac hydatidosis with invasion of both pulmonary artery and vein, which eventually altered the surgical management of patient.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Hydatid disease is a parasitic infection caused by Echincococcus granulosus, and is still endemic in multiple regions across the globe including India. Although it commonly affects the liver and various other organs, isolated involvement of the heart is relatively uncommon. It can be confidently diagnosed on echocardiography but cross sectional imaging by computed tomography (CT) or magnetic resonance imaging (MRI) provides accurate information about its location, extent, and multiplicity. Accurate localization and detailed reporting upon the invasion of surrounding vascular structures is crucial for deciding upon the appropriate treatment protocol of the patient. Multiple case studies of cardiac hydatid disease have been reported in literature but cardiac hydatidosis with extension into pulmonary vasculature has not been reported commonly. This case report highlights this rare association, with stress upon the altered surgical management.
Case presentation
A 50-year-old male presented to the cardiology outpatient department of a tertiary care hospital with complaints of malaise, fatigue as well as atypical chest pain for the past six months. As part of routine examination, he underwent multiple blood tests as well as electrocardiography which were within normal limits. Further, a transthoracic echocardiography (TTE) was performed which revealed a large multicystic mass with internal septations invading the posterolateral wall of the left ventricle (LV). No internal vascularity was detected on colour Doppler imaging. A provisional diagnosis of hydatid cyst was therefore formulated, and the patient was sent for a cardiac computed tomography (CT) for better anatomical evaluation of the lesion.
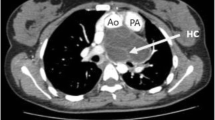
Cardiac CT revealed a large, well-demarcated, non-enhancing, multicystic, intramyocardial lesion, arising from the posterolateral wall of LV with mass effect on the ventricular cavity. It was also causing extreme thinning of the LV free wall and was seen extending to the apex of heart as well as along the left lateral chest wall. Smooth posterior displacement of left inferior pulmonary vein (PV) was also noted. Additionally, another similar but smaller lesion was seen in the left atrial appendage, with extension into the right branch of pulmonary artery (PA), just prior to its bifurcation. However, normal distal contrast opacification of the vessel was seen (Fig. 1).
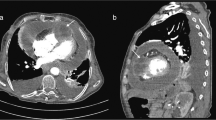
In order to establish the involvement of the pulmonary vessels as well as other mediastinal structures, a cardiac MRI was performed for the patient which, in addition to the above findings (Figs. 2, 3B), also showed invasion of right superior PV (Fig. 3A) along with compression of SVC. Subsequent to imaging, a final diagnosis of cardiac hydatidosis with extensive invasion into LV myocardium and right pulmonary vessels was made.
Patient underwent surgical exploration, wherein after injecting hypertonic saline (5%), cysts were punctured and both the fluid content and daughter cysts were aspirated (Fig. 4). Enucleation could not be performed for the lesion involving LV due to extreme thinning of its lateral wall and negligible residual myocardium to support the ventricular cavity. Extensive invasion into pulmonary vasculature further averted enucleation of lesion involving the LAA. After aspiration of the lesions, reconstruction of right PA and right superior PV was performed following which the patient was discharged after a short hospital stay.
Discussion
Hydatid disease is a parasitic infection caused by the larvae of Echinococcus granulosus. It uncommonly involves the heart (0.5–2%), with left ventricle being the first in order (60%), owing to the dominance of left coronary artery and its greater myocardial mass [1]. Cardiac contractions usually prevent involvement by the viable daughter cyst, which if ineffective rarely leads to myocardial invasion [2]. Other sites such as interventricular septum (10–20%) or right ventricle (5–15%) [3] can be involved as well with infection spreading either through blood circulation or as a direct extension from the surrounding structures. Arterial involvement by hydatid is thought to be either secondary to rupture and embolization of membranes, which presents acutely or due to the intravascular growth of hydatid, which may cause chronic occlusion.
Once invasion occurs, cyst grows slowly with tendency to grow sub-epicardially on the left side and intracavitary or sub-endocardially on the right side of the heart. Once large enough, it presents clinically depending upon the location, with symptoms such as dyspnoea, conduction defects and palpitations. It also poses the risk of compression of the surrounding structures or sudden rupture causing anaphylaxis, embolization or even death. Pericardial involvement is another uncommon feature, where rupture can lead to pericarditis or cardiac tamponade. Involvement of left atrial appendage with associated invasion of pulmonary vasculature though extremely rare can cause frightful complications such as acute pulmonary hypertension or systemic arterial embolization [1].
Echocardiography is a sensitive tool in diagnosing cardiac hydatid cyst, which appears as an anechoic lesion with or without multiple daughter cysts. However, echocardiography is limited by multiple factors most important being small field of view and poor acoustic window in certain patients. Cardiac CT and MRI hold great significance in providing detailed characterization as well as assessment of the lesion particularly its location, multiplicity and relation to the surrounding structures. While CT reliably depicts wall calcification and local extension, MRI due to its better tissue characterization properties can assess for risk of rupture, involvement of vascular structures and impact on myocardial contraction [3]. Cardiac MRI is also the modality preferred for post-treatment follow-up.
Treatment in cases of cardiac hydatid cyst is essentially surgical where prior to enucleation, an anti-helminthic solution (2% formalin, 20% hypertonic saline, 0.5% silver nitrate solution or 5% cetrimonium bromide solution) is injected into the lesion, to reduce the risk of anaphylaxis due to sudden rupture [4]. Anti-helminthic drugs are continued post operatively to reduce the recurrences. In our case, enucleation could not be performed due to the invasiveness of the lesion with only aspiration and removal of both the daughter cysts and fluid content.
Conclusions
Cardiac hydatid disease with involvement of pulmonary vasculature is an extremely rare condition which requires detailed anatomical reporting to help decide surgical management. Pulmonary artery involvement of hydatid is thought to be either secondary to rupture and embolization of germinating membranes, which can lead to acute presentation or due to the intravascular growth of hydatid, which if undiagnosed can lead to chronic occlusion. Imaging studies play a crucial role and therefore should be appropriately utilized in assessing the multiplicity and complete extension of such lesions pre-operatively. Cardiac hydatidosis with multiple lesions invading both PA and PV has not been previously described and needs to be actively ruled out as failure to recognize and treat these may lead to incomplete resection and relapse of disease in the future.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- ECG:
-
Electrocardiography
- LAA:
-
Left atrial appendage
- LV:
-
Left ventricle
- MRI:
-
Magnetic resonance imaging
- PA:
-
Pulmonary artery
- PV:
-
Pulmonary vein
- TTE:
-
Transthoracic echocardiography
- SVC:
-
Superior vena cava
References
Dursun M, Terzibasioglu E, Yilmaz R, Cekrezi B, Olgar S, Nisli K et al (2008) Cardiac hydatid disease: CT and MRI findings. AJR 190:226–232
Shojaei E, Yassin Z, Rezahosseini O (2016) Cardiac hydatid cyst: a case report. Iran J Public Health 45(11):1507–1510
Nasri S, Aichouni N, Lokman S, Ouafi NE, Kamaoui I, Skiker I (2021) Cardiac hydatid cyst: 2 case reports. Radiol Case Rep 3829–33.
Prasad K, Kumar R, Halder V, Raju M, Negi SL, Naganur S (2021) Multimodality imaging of an interventricular septum hydatid cyst. Egypt Heart J 73:23
Acknowledgements
We are thankful to senior radiographer Mr. Dinesh Mishra for providing the images.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
VG involved in substantial contributions to the conception provided, design of the work, interpretation of the data and manuscript draft. PG involved in substantial contributions to the conception provided, design of the work, interpretation of the data and substantial revision of the manuscript. KB involved in substantial contributions to analysis of the data and interpretation and revision of the manuscript. NS involved in substantial contributions to the conception provided and analysis of the data and interpretation. SEHN involved in substantial contributions to the analysis of the data and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patient included in this study provided the written informed consent to participate in this research.
Consent for publication
The patient included in this research gave a written and informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, V., Bansal, K., Gupta, P. et al. Cardiac hydatidosis complicated by vascular involvement: a case report. Egypt J Radiol Nucl Med 54, 165 (2023). https://doi.org/10.1186/s43055-023-01080-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01080-3