Abstract
Background
The Ki-67 is a beneficial marker of tumor aggressiveness. It is proliferation index that has been used to distinguish luminal B from luminal A breast cancers. By fast progress in quantitative radiology modalities, tumor biology and genetics can be assessed in a more accurate, predictive, and cost-effective method. The aim of this study was to assess the role of dynamic contrast-enhanced magnetic resonance imaging, diffusion-weighted imaging and diffusion tensor imaging in prediction of Ki-67 status in patients with invasive breast carcinoma estimate cut off values between breast cancer with high Ki-67 status and those with low Ki-67 status.
Results
Cut off ADC (apparent diffusion co-efficient) value of 0.657 mm2/s had 96.4% sensitivity, 75% specificity and 93.8% accuracy in differentiating cases with high Ki67 from those with low Ki67. Cut off maximum enhancement value of 1715 had 96.4% sensitivity, 75% specificity and 93.8% accuracy in differentiating cases with high Ki67 from those with low Ki67. Cut off washout rate of 0.73 I/S had 60.7% sensitivity, 75% specificity and 62.5% accuracy in differentiating cases with high Ki67 from those with low Ki67. Cut off time to peak value of 304 had 71.4% sensitivity, 75% specificity and 71.9% accuracy in differentiating cases with high Ki67 from those with low Ki67.
Conclusions
ADC, time to peak and maximum enhancement values had high sensitivity, specificity and accuracy in differentiating breast cancer with high Ki-67 status from those with low Ki-67 status.
Similar content being viewed by others
Background
Breast cancer is the most commonly diagnosed cancer and the main cause of death among female patients, the incidence of breast cancer is increasing year by year and younger female patients have been diagnosed with it [1,2,3]. According to gene expression pattern, there are four different molecular subtypes of breast cancer: luminal A (LA), luminal B [(LB; HER2−), LB (HER2+)], human epidermal growth factor receptor 2 (HER2)-enriched, and basal-like (triple-negative) [4,5,6,7,8,9,10]. The molecular subtyping of breast cancer turns out a fundamental requirement for treatment design and disease prognosis [11, 12].
The Ki-67 is a beneficial marker of tumor aggressiveness [7, 8, 13]. It is a proliferation index that has been used to distinguish LB from LA breast cancers [13]. LA breast cancers are those with ER- and/or PR-positive and low Ki-67 index, while LB breast cancers are those with ER- and/or PR-positive and high Ki-67 index [14]. Patients with the LB breast cancer had a higher proliferation rate and a worse prognosis than those with the LA breast cancer [15,16,17]. The Ki-67 expression determination rule is follows: the proportion of positive cancer cells in the sample is counted, and the percentage more than 14% is defined as high expression; otherwise, it is low expression [18].
Dynamic contrast-enhanced breast MRI (DCE-MRI) is the most sensitive imaging modality for detection of breast cancer. It permits precious localization of suspicious breast masses, permits accurate estimation of pectoral muscle and chest wall invasion by breast cancer and also permits detection of lymphatic metastasis [19]. Recently, diffusion tensor imaging (DTI), an extension of diffusion-weighted imaging (DWI), has been utilized to distinguish benign from malignant breast lesions and shows favorable results in increasing diagnostic specificity. It can calculate the anisotropy and directionality of water diffusion in tissues by encoding the diffusion in six or more directions. The DTI parameters include fractional anisotropy (FA), mean diffusivity (MD), and three orthogonal diffusion coefficients (λ1, λ2, λ3) [20, 21].
By fast progress in quantitative radiology modalities, tumor biology and genetics can be assessed in a more accurate, predictive, and cost-effective method [22]. Several previous studies investigated the relationship between quantitative MRI parameters and molecular subtypes of breast cancer [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]; however, there is still no evident data about cut off values between breast cancers with low Ki-67 proliferation index and those with high Ki-67 proliferation index.
Aim of the study
The aim of this study was to assess the role of DCE-MRI, DWI & DTI in prediction of Ki-67 status in patients with invasive breast carcinoma and estimate cut off values between breast cancer with high Ki-67 status and those with low Ki-67 status.
Methods
Patient's demographic data
This prospective study was conducted during the period from May 2020 to October 2022. Approval from our institution’s ethics committee was obtained and informed consent was obtained from all female patients before inclusion in this research work. This study included 96 female patients with pathologically proven breast cancer of different molecular subtypes. Their mean age (years) ± SD was 46.41 ± 9.55 years with age range from 31 to 69 years.
Inclusion criteria patients suspected to have breast cancer on basis of sonomammography (patients with BI-RADS 5 lesions on sonomammography).
Exclusion criteria patients who were lost and their pathological results were not available, patients with improper imaging techniques (motion artifact and magnetic susceptibility artifact), patients who received NAC before performing breast MRI patients with recurrent breast carcinoma after performing conservative breast surgery and patients who had general contraindications to do MRI as patients with cardiac pace maker, patients with cochlear implant and ocular foreign body.
MRI technique
MR images were obtained by using a 1.5 T MR imaging unit (Ingenia. Philips, Best, Netherlands). All studies were performed with the patients in a prone position by using a dedicated breast coil. All patients underwent the following. Localizing scout view (sagittal plane), axial nonfat saturated TIWI was obtained by FSE with the following imaging parameters: TR 450 ms, TE 14 ms, slice thickness 3 mm, field of view (FOV) 300–360 mm, axial T2WI was obtained using FSE with the following imaging parameters TR 2000 ms, TE 80 ms, slice thickness 3 mm, FOV 300–360 mm, axial STIR images was obtained with the following parameters: TR 7000–9000 ms, TE 70 ms & inversion time (TI) was 150 ms, slice thickness was 3–4 mm with inter slice gap 1 mm and FOV 300–360 mm.
DCE-MRI was obtained in the axial plane with fat suppression by applying fat saturated pulse (FLASH 3 D GRE-T1W1) with the following parameters: TR 4–8 ms, TE 2 ms, flip angle 20–25 degrees, slice thickness 3 mm with no inter-slice gap, FOV 300–360 mm and matrix was 38 × 384. After the pre-contrast study, a bolus of gadopentetate dimeglumine (gadolinium) in a dose of 0.2 mmol/kg was injected using an automated injector at a rate of 3–5 ml/s. This was followed by a bolus injection of saline (total of 20 ml at 3–5 ml/s). Dynamic study consisted of one pre contrast and 3 post contrast series, each of them took about 1.15 min., the first two contrast-enhanced acquisitions (wash-in rate) represented early contrast-enhanced phase while the delayed images (washout kinetics) represented delayed-phase enhancement. Image subtraction was obtained by subtracting each of pre-contrast images from each post-contrast series images. Time to signal intensity curves were created for suspicious enhancing lesions by placing ROI within the most enhancing portion of the lesion. The horizontal axis of the curve represented the series number or time and the vertical axis represented signal intensity that was automatically calibrated by the machine according to the SI (enhancement) of the lesion.
DWI was done before dynamic images, by acquiring conventional T2-weighted images with addition of strong diffusion gradients using single shot spin echo EPI sequence with TR/TE/NEX: 5800/139 ms/1 with b values = 0, 500, and 1000 mm2/s. The diffusion gradients were applied sequentially in the three orthogonal directions (X, Y & Z directions). Sections of 4 mm thickness, inter-slice gap of 1 mm, a 300–360 mm FOV, and a 128 × 256 matrix were used for all images. The total acquisition time was 120 s. Orthogonal (DWI) images & ADC maps were obtained in all cases.
DTI was performed using an axial two-dimensional spin-echo echo planar imaging sequence, b value = 0 and 800 s/mm2, diffusion gradient directions = 12, TR = 4000 ms, TE = 101 ms, diffusion gradient directions = 12, slice-thickness = 2.5 mm with no inter-slice gap, NOE = 4, FOV = 380 × 285 mm2, matrix = 256 × 256, acquisition time = 4 min. DTI was performed before the contrast-enhanced study. All DTI data were post-processed using (extended MR 130Workspace 2.6.3.5, Philips Medical Systems Netherland). The slice with the maximum diameter of the lesion was selected for the image analysis.
Image interpretation
Quantitative analysis of MR images was carried out by 2 radiologists (DM, DE) with 20 and 11 years of breast imaging experience. Analysis of enhancement kinetics based on evaluation of the data obtained by the time signal intensity curve. The analysis and determination of the profile of the signal to time curve was based on a protocol as follows: Wash in rate: In which the initial signal increase from the pre-contrast measurement to the maximum value increase within the first 3 min after administration of contrast medium. It was classified into slow (> 50%), intermediate (50–90%) or rapid (≥ 90%). Wash out rate: It is the post-initial behavior of the signal curve from the maximum peak to the end of the examination. Three types of curves were defined: Type I “persistent curve”, Type II “plateau curve” and Type III “wash out curve”.
ADC maps were automatically reconstructed using Philips's extended workspace (EWS) release 2.6 workstation. Mean ADC values of suspicious lesions were measured. Firstly, a slice from the axial ADC maps where the lesion was adequately apparent was chosen. Then a circular region of interest (ROI) measuring about 10 mm2 was located within the center of the lesion by using an electronic cursor (corresponding to the enhanced portion of the lesion on dynamic MR images excluding areas of hemorrhage and necrosis).
DTI parametric colored maps were automatically generated for FA, FA parametric map were overlaid on DCE-MRI images, which was used as a reference to define the lesion allowing accurate ROI placement. A free-hand ROI was drawn to include the largest solid area of the lesion in a single slice, excluding the necrotic, hemorrhagic, and cystic areas. The DTI parameter was automatically calculated including FA: FA ranges between 0 (isotropic diffusion) to 1 (free diffusion in one direction).
Final diagnosis
The results of the histopathological examination were considered our standard of reference. The interval between the MRI examination and trucut biopsies was 10–15 days. Final pathological data were revised by an experienced pathologist (12 years' experience in breast pathology). Regarding the analysis of Ki-67, immunohistochemical, staining was conducted and the proportion of the malignant cells staining positive for the nuclear antigen Ki-67 was evaluated in a quantitative and visual way using light microscopes. The proportion of positive cancer cells in the sample is counted, and the proportion greater than 14% is defined as high expression; otherwise, it is low expression.
Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Qualitative data were described using number and percent. Quantitative data were described using median (minimum and maximum) for non-parametric data and mean, standard deviation for parametric data after testing normality using Kolmogrov-Smirnov test. Significance of the obtained results was judged at the (0.05) level. Mann–Whitney U test was used to compare 2 independent groups. Kruskal Wallis test was used to compare more than 2 independent groups with Mann–Whitney U test to detect pair-wise comparison. In order to evaluate the diagnostic accuracy or the diagnostic performance of a test, we performed an analysis of the Receiver Operating Characteristic (ROC) curve. Sensitivity and specificity were tested at different cutoff points by the ROC curve. Positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated through cross-tabulation.
Results
This prospective study included 96 female patients with pathologically proven breast cancer with age range from 31 to 69 with mean age 46.41 ± 9.55. Out of the 96 patients, 90 patients were pathologically proven invasive ductal carcinoma, 3 patients pathologically proven invasive lobular carcinoma and the remaining 3 patients were pathologically proven mucinous carcinoma. According to the tumor grade among the studied cases, the majority of the cases were grade II representing about 72% of cases. According to the expression of biological markers among the studied cases; ER & PR were positive in 78.1% of cases, HER2 + 1 was found in 44.7% of the cases and Ki67 was high in 87.5% of cases. According to the molecular subtypes among the studied cases, 9 cases were luminal A, 81 cases were luminal B (HER2-ve), 6 cases were HER2 enriched and remaining 15 cases were triple negative (Table 1).
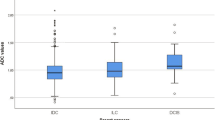
When correlating the Ki-67 status with maximum enhancement, washout ratio and time to peak values, maximum enhancement values were significantly higher in cases with high Ki-67 (1873.05 (1023.4–2032)) (Fig. 1) compared to cases with low Ki-67 (1547.9 (699–1727)) (P value < 0.001) (Fig. 2). Washout ratio was significantly higher in cases with high Ki-67 (0.875 (0.71–1.4)) compared to cases with low Ki-67 (0.65 (0–10.2)) (P value = 0.045). While time to peak was significantly lower in cases with high Ki-67 (266 (97–677)) compared to those with low Ki-67 (331.5 (210.7–454.2)) (P value = 0.046) (Table 2).
Female patient aged 42 years old presented by palpable left breast mass. A Axial early subtraction MR image shows irregular shaped soft tissue mass with speculated margin and heterogeneous enhancement within the lower outer quadrant of the left breast. B, C Axial DWI and ADC show high SI in DWI and low SI on ADC map (restricted diffusion) with mean ADC value = 0.32 × 10–3 mm2/s. D Axial DTI image shows FA value 0.18. E, F Time intensity curve shows Type III curve (wash out curve) with maximum enhancement 2248.6, Time to peak 137.2swith wash out ratio 1.5 s. G Pathological diagnosis was grade III invasive ductal carcinoma luminal B her2 positive (ER and PR positive with high Ki-67 index (Ki-67 = 80%) and HER2-positive)
Female patient aged 35 years old presented by palpable left breast mass. A axial early subtraction MRI image shows Irregular shape, heterogeneously enhanced soft tissue mass with speculated margin within the upper inner quadrant of the left breast, B, C axial DWI and ADC show high signal intensity within DWI and low signal intensity in ADC map (restricted diffusion) with mean ADC value = 0.9 × 10–3 mm2/s. D axial DTI image shows FA value = 0.5. E, F Time Intensity curve shows Type II curve (plateau curve) with maximum enhancement about 1636, time to peak 426 s without washout. G Pathological diagnosis was grade II invasive ductal carcinoma, luminal A (ER and PR positive and low Ki-67 index (ki-67 = 5%)
When correlating the Ki-67 status with ADC & FA values, we found that ADC value was significantly lower in cases with high Ki-67 (0.502 (0.20–0.68)) (Fig. 1) comparing to those with low Ki-67 (0.88 (0.3–0.92)) (P value = 0.002) (Fig. 2). Regarding FA value there was no significant difference in FA values in cases with high Ki-67 (0.2 (0.09–0.7)) and cases with low Ki-67 (0.245 (0.15–0.50)) (P value = 0.689) (Table 2).
According to ROC curve analysis, cut off maximum enhancement value of 1715 had 96.4% sensitivity, 75% specificity and 93.8% accuracy in differentiating cases with high Ki-67 from those with low Ki-67. Cut off washout rate of 0.73 I/S had 60.7% sensitivity, 75% specificity and 62.5% accuracy in differentiating cases with high Ki-67 from those with low Ki-67. Cut off time to peak value of 304 had 71.4% sensitivity, 75% specificity and 71.9% accuracy in differentiating cases with high Ki-67 from those with low Ki-67. Cut off ADC value of 0.657 mm2/s had 96.4% sensitivity, 75% specificity and 93.8% accuracy in differentiating cases with high Ki-67 from those with low Ki-67 (Table 3).
Discussion
Ki-67 is the most commonly utilized immunohistochemical marker in breast cancer detection, and its expression level is related closely to tumor type, invasiveness, prognosis and effect of treatment. In clinical practice, the expression of Ki-67 in breast cancer is acquired through pathological tissue staining and immunohistochemical analysis [23]. Breast MRI provide data on not only about the morphological features of the tumor but also about the functional features of the tumor [24,25,26]. In this study, we tried to investigate the role of breast MRI (DCE-MRI, DWI & DTI) in differentiating breast cancers with low Ki-67 status from those with high Ki-67 status.
In our study tumors with high Ki-67 showed lower time to peak compared to those with lower Ki-67 with cut off time to peak value of 304 had 71.4% sensitivity, 75% specificity and 71.9% accuracy in differentiating cases with high Ki-67 from those with low Ki-67. This is in agreement with Fernández-Guinea et al. [27] who stated that tumors with high Ki-67 had lower time to peak compared to those with low Ki67. Also our results are in agreement with Shin et al. [28] who stated that the median time to maximum enhancement of cancers with high Ki-67 was shorter than that of cancers with low Ki-67 (p < 0.001). Also our results are in agreement with Onishi et al. [29] who stated that aggressive invasive breast cancers as those with high Ki-67 tend to have shorter bolus arrival time compared to those with low Ki-67.
Regarding maximum enhancement and washout rate we found that tumors with high Ki-67 had higher values compared to tumors with low Ki-67, with cut off maximum enhancement value of 1715 showed 96.4% sensitivity and 75% specificity in differentiating cases with high Ki-67 from those with low Ki-67. Cut off washout rate of 0.73 I/S had 60.7% sensitivity and 75% specificity in differentiating cases with high Ki-67 from those with low Ki-67. This could be explained by the overexpression of the vascular endothelial growth factor (VEGF) in tumors with high Ki-67 proliferation index [8]. This is in agreement with other studies [30, 31], they stated that there was positive correlation between Ki-67 and maximum enhancement values, where tumors with high Ki-67 showed higher maximum enhancement values compared to those with low Ki-67. Also our results are in agreement with other studies [32, 33], they stated that tumors with high Ki-67 usually demonstrate type III time signal intensity curve with high wash out rates.
In this study we found that tumors with high Ki-67 had lower mean ADC value compared to those with low Ki-67, we found that cut off ADC value of 0.657 mm2/s had 96.4% sensitivity, 75% specificity and 93.8% accuracy in differentiating cases with high Ki-67 from those with low Ki-67. Our results are in agreement with several previous studies [34,35,36,37,38,39,40], all these studies stated that tumors with high Ki-67 had significantly lower ADC values compared to those with low Ki-67. Shen et al. [41] estimated that cut off mean ADC value of 0.97 × 10−3 mm2/s had 100% sensitivity in differentiating tumors with high Ki67 proliferation index from those with low Ki 67. Also Li et al. [23] stated that there was inverse relationship between mean ADC value and Ki-67 status. The mean ADC value was 0.820 × 10–3 mm2/s for tumors with high Ki-67 versus 0.980 × 10–3 mm2/s, for tumors with low Ki-67 proliferation index (P = 0.001). The lower ADC value in tumors with high Ki-67 proliferation index is attributed to rapid proliferation and high cellularity of these tumors and this restricts the diffusion of water molecules in the extracellular and extravascular spaces [42].
There are few limitations in this research work. First, inter observer agreement about the patient’s data was not performed. Second, not all DTI parameters were examined and we assessed only the FA value.
Conclusions
ADC, time to peak and maximum enhancement values have high sensitivity, specificity and accuracy in differentiating breast cancer with high Ki-67 status from those with low Ki-67 status.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DCE-MRI:
-
Dynamic contrast-enhanced magnetic resonance imaging
- DWI:
-
Diffusion-weighted imaging
- DTI:
-
Diffusion tensor imaging
- HER2:
-
Human epidermal growth factor receptor 2
- LA:
-
Luminal A
- LB:
-
Luminal B
- FA:
-
Fractional anisotropy
- MD:
-
Mean diffusivity
- SD:
-
Standard deviation
- BI-RADS:
-
Breast imaging reporting and data system
- NAC:
-
Neoadjuvant chemotherapy
- FSE:
-
Fast spin echo
- TE:
-
Echo time
- TR:
-
Repetition time
- FOV:
-
Field of view
- ROI:
-
Region of interest
- EWS:
-
Extended workspace
- ADC:
-
Apparent diffusion coefficient
- ROC:
-
Receiver operating curve
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- VEGF:
-
Vascular endothelial growth factor
References
Kamińska M, Ciszewski T, Łopacka-Szatan K, Miotła P, Starosławska E (2015) Breast cancer risk factors. Przeglad Menopauzalny Menopause Review 3(3):196–202
Armstrong K, Eisen A, Weber B (2000) Assessing the risk of breast cancer. N Engl J Med 342(8):564–571
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Ades F, Zardavas D, Bozovic-Spasojevic I, Pugliano L, Fumagalli D, de Azambuja E et al (2014) Luminal B breast cancer: molecular characterization, clinical management, and future perspectives. J Clin Oncol 32(25):2794–2803
Gao JJ, Swain SM (2018) Luminal a breast cancer and molecular assays: a review. Oncologist 23(5):556–565
Ignatiadis M, Sotiriou C (2013) Luminal breast cancer: from biology to treatment. Nat Rev Clin Oncol 10(9):494–506
Liu FF, Shi W, Done SJ, Miller N, Pintilie M, Voduc D et al (2015) Identification of a low-risk luminal A breast cancer cohort that may not benefit from breast radiotherapy. J Clin Oncol 33(18):2035–2040
Kazama T, Takahara T, Hashimoto J (2022) Breast cancer subtypes and quantitative magnetic resonance imaging: a systemic review. Life 12:490
Huang J, Lin Q, Cui C, Fei J, Su X, Li L et al (2020) Correlation between imaging features and molecular subtypes of breast cancer in young women (≤ 30 years old). Jpn J Radiol 38(11):1062–1074
Jenkins S, Kachur ME, Rechache K, Wells JM, Lipkowitz S (2021) Rare breast cancer subtypes. Curr Oncol Rep 23:54
Romeo V, Accardo G, Perillo T, Basso L, Garbino N, Nicolai E et al (2021) Assessment and prediction of response to neoadjuvant chemotherapy in breast cancer: a comparison of imaging modalities and future perspectives. Cancers 13(14):3521
- Matzke LA, Watson PH (2020) Biobanking for cancer biomarker research: issues and solutions. Biomark Insights 15
Ferguson NL, Bell J, Heidel R, Lee S, Vanmeter S, Duncan L et al (2013) Prognostic value of breast cance subtypes, Ki-67 proliferation index, age, and pathologic tumor characteristics on breast cancer survival in Caucasian women. Breast J 19(1):22–30
Rashmi S, Kamala S, Murthy SS, Kotha S, Rao YS et al (2018) Predicting the molecular subtype of breast cancer based on mammography and ultrasound findings. Indian J Radiol Imaging 28(03):354–361
Kim KI, Lee KH, Kim TR, Chun YS, Lee TH, Park HK (2014) Ki-67 as a predictor of response to neoadjuvant chemotherapy in breast cancer patients. J Breast Cancer 17(1):40–46
Nishimura R, Osako T, Okumura Y, Hayashi M, Toyozumi Y, Arima N (2010) Ki-67 as a prognostic marker according to breast cancer subtype and a predictor of recurrence time in primary breast cancer. Exp Ther Med 1(5):747–754
Inwald EC, Klinkhammer-Schalke M, Hofstädter F, Zeman F, Koller M, Gerstenhauer M et al (2013) Ki-67 is a prognostic parameter in breast cancer patients: results of a large population-based cohort of a cancer registry. Breast Cancer Res Treat 139(2):539–552
Potemski P, Pluciennik E, Bednarek AK, Kusinska R, Kubiak R, Jesionek-Kupnicka D et al (2006) Ki-67 expression in operable breast cancer: a comparative study of immunostaining and a real-time RT-PCR assay. Pathol Res Pract 202(7):491–495
Mann RM, Cho N, Moy L (2019) Breast MRI: state of the art. Radiology 292(3):520–536
Baxter GC, Graves MJ, Gilbert FJ, Patterson AJ (2019) A meta-analysis of the diagnostic performance of diffusion mri for breast lesion characterization. Radiology 291:632–641
Onaygil C, Kaya H, Ugurlu MU, Aribal E (2017) Diagnostic performance of diffusion tensor imaging parameters in breast cancer and correlation with the prognostic factors. J Magn Reson Imaging 45:660–672
Wu J, Tha KK, Xing L, Li R (2018) Radiomics and radiogenomics for precision radiotherapy. J Radiat Res 59(1):25–31
Li Y, Huang Y, Su X, Gu Z, Lai Q, Huang J et al (2022) Breast MRI segmentation and Ki-67 high- and low-expression prediction algorithm based on deep learning. Comput Math Methods Med
Kuhl C (2007) The current status of breast MR imaging. Part I. Choice of technique, image interpretation, diagnostic accuracy, and transfer to clinical practice. Radiology 244:356–378
Kuhl CK (2015) The changing world of breast cancer: a radiologist’s perspective. Investig Radiol 50:615–628
Trimboli RM, Codari M, KhouriChalouhi K, Ioan I, Lo Bue G, Ottini A et al (2018) Correlation between voxel-wise enhancement parameters on DCE-MRI and pathological prognostic factors in invasive breast cancers. Radiol Med 123:91–97
Fernández-Guinea O, Andicoechea A, González LO, González-Reyes S, Merino AM, Hernández LC et al (2010) Relationship between morphological features and kinetic patterns of enhancement of the dynamic breast magnetic resonance imaging and clinico-pathological and biological factors in invasive breast cancer. BMC Cancer 10:8
Shin SU, Cho N, Kim SY, Lee SH, Chang JM, Moon WK (2020) Time-to-enhancement at ultrafast breast DCE-MRI: potential imaging biomarker of tumour aggressiveness. Eur Radiol 30:4058–4068
Onishi N, Sadinski M, Hughes MC, Ko ES, Gibbs P, Gallagher KM et al (2020) Ultrafast dynamic contrast-enhanced breast MRI may generate prognostic imaging markers of breast cancer. Breast Cancer Res 22:58
Caiazzo C, Di Micco R, Esposito E, Sollazzo V, Cervotti M, Varelli C et al (2018) The role of MRI in predicting Ki-67 in breast cancer: preliminary results from a prospective study. Tumori 104:438–443
Song SE, Cho KR, Seo BK, Woo OH, Park KH, Son YH et al (2019) Intravoxel incoherent motion diffusion-weighted MRI of invasive breast cancer: correlation with prognostic factors and kinetic features acquired with computer-aided diagnosis. J Magn Reson Imaging 49:118–130
Girardi V, Carbognin G, Camera L, Tonegutti M, Bonetti F, Manfrin E et al (2010) Fischer’s score criteria correlating with histopathological prognostic factors in invasive breast cancer. Radiol Med 115:421–433
Lee SH, Cho N, Kim SJ, Cha JH, Cho KS, Ko ES et al (2008) Correlation between high resolution dynamic MR features and prognostic factors in breast cancer. Korean J Radiol 9:10–18
Li L, Wang K, Sun X, Wang K, Sun Y, Zhang G et al (2015) Parameters of dynamic contrast-enhanced MRI as imaging markers for angiogenesis and proliferation in human breast cancer. Med Sci Monit 21:376–382
Molinari C, Clauser P, Girometti R, Linda A, Cimino E, Puglisi F et al (2015) MR mammography using diffusion-weighted imaging in evaluating breast cancer: a correlation with proliferation index. Radiol Med 120:911–918
Kim EJ, Kim SH, Park GE, Kang BJ, Song BJ, Kim YJ et al (2015) Histogram analysis of apparent diffusion coefficient at 3.0t: correlation with prognostic factors and subtypes of invasive ductal carcinoma. J Magn Reson Imaging 42:1666–1678
Catalano OA, Horn GL, Signore A, Iannace C, Lepore M, Vangel M et al (2017) PET/MR in invasive ductal breast cancer: correlation between imaging markers and histological phenotype. Br J Cancer 116:893–902
Kitajima K, Yamano T, Fukushima K, Miyoshi Y, Hirota S, Kawanaka Y et al (2016) Correlation of the SUVmax of FDG-PET and ADC values of diffusion-weighted MR imaging with pathologic prognostic factors in breast carcinoma. Eur J Radiol 85:943–949
Tuan Linh L, Minh Duc N, Minh Duc N, Tra My TT, Viet Bang L, Cong Tien N et al (2021) Correlations between apparent diffusion coefficient values and histopathologic factors in breast cancer. Clin Ter 172:218–224
Shin JK, Kim JY (2017) Dynamic contrast-enhanced and diffusion-weighted MRI of estrogen receptor-positive invasive breast cancers: associations between quantitative MR parameters and Ki-67 proliferation status. J Magn Reson Imaging 45(1):94–102
Shen L, Zhou G, Tong T, Tang F, Lin Y, Zhou J et al (2018) ADC at 3.0 T as a noninvasive biomarker for preoperative prediction of Ki67 expression in invasive ductal carcinoma of breast. Clin Imaging 52:16–22
Onishi N, Kanao S, Kataoka M, Iima M, Sakaguchi R, Kawai M et al (2015) Apparent diffusion coefficient as a potential surrogate marker for Ki-67 index in mucinous breast carcinoma. J Magn Reson Imaging 41:610–615
Acknowledgements
Not applicable.
Funding
No funding resources.
Author information
Authors and Affiliations
Contributions
DM revised the collected data and the manuscript. DE & AM analyzed the MR images of all patients. DE & AM wrote the manuscript. DE performed the statistical analysis. AH revised the pathological data of all patients. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by our institution’s ethics committee (Mansoura Faculty of Medicine Institutional Research Board) (ethics committee reference number is MS.20.10.1) and all patients gave their written informed consent before inclusion in the study.
Consent for publication
Written informed consent for the publication of this data was taken from the patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
EL-Metwally, D., Monier, D., Hassan, A. et al. Preoperative prediction of Ki-67 status in invasive breast carcinoma using dynamic contrast-enhanced MRI, diffusion-weighted imaging and diffusion tensor imaging. Egypt J Radiol Nucl Med 54, 62 (2023). https://doi.org/10.1186/s43055-023-01007-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01007-y