Abstract
Background
Noninvasive preoperative evaluation of axillary lymph nodes proved to have a significant role not only on the protocol of treatment of breast cancer but also impact the whole life of the patient. Complications of lymph node biopsy or axillary clearance increase the need for noninvasive reliable diagnostic tool. We aimed in the current study to evaluate the role of diffusion-weighted magnetic resonance imaging (DW-MRI) and apparent diffusion coefficient (ADC) in discrimination between benign and malignant axillary lymph nodes. We included 44 suspicious lymph nodes from 29 patients. Qualitative DW-MRI was analyzed into restricted or not; ADC maps and cut-off value were calculated, and they were correlated with histopathological results, which were the gold standard tool of the current study.
Results
The cut-off value of ADC-differentiated between malignant and benign lymph nodes was 0.89 × 10−3 mm2/s. The statistical indices including the sensitivity, specificity, PPV, NPV and accuracy were 89.66%, 86.67%, 93.9, 81.2% and 87.8%, respectively, with P value < 0.001, while DW-MRI results were classified into restricted or not restricted with qualitative statistical indices of 96.6%, 80%, 90.3%, 92.3% and 90.9% for sensitivity, specificity, PPV, NPV and accuracy, respectively, with P value < 0.001.
Conclusion
DW-MRI and ADC both have significant role in discrimination between benign and malignant axillary lymph nodes increasing the accuracy of MRI examination in breast cancer patients.
Similar content being viewed by others
Background
Axillary lymph node metastasis is common in breast cancer patients affecting the treatment modalities as well as surgical procedures [1]. Axillary lymph node dissection and biopsy are considered invasive methods which have long- and short-term complications on patients with breast cancer negatively affecting their life quality [2].
It had been shown that complete axillary lymph node dissection (ALND) for breast cancer patients with limited nodal invasion (1–3 nodes) is not useful; additionally, nodal biopsy which is an invasive technique carries a potential risk of complications [3].
Diffusion-weighted magnetic resonance imaging (DW-MRI) is a noninvasive technique, which works on Brownian motion of water molecules, which are dependent on certain parameters; for example, size of the cell, cell membrane permeability and inside and outside cellular volume fraction [4].
During the acquisition, motion-sensitizing gradients used b-value in the real DW-MRI or sensitization (s/mm2), so no need for contrast because the DW-MRI has its own tissue contrast, ADC is the representative extent of the water molecules of the examined tissue occupies as square mm per second [5]. Identification of the nodes on DW-MRI was remarkably higher than that on T2WI, with marked high SI compared with adjacent muscles and surrounding normal vessels made it easy to identify [6].
Aim of the work
The purpose of this study was to evaluate the role of DW-MRI and ADC in discrimination between benign and malignant axillary lymph nodes in breast cancer patients.
Methods
This study was a prospective study from January 2019 to August 2021 at our institution.
The study included 35 patients with ages ranged from (28–66 y) with mean age (47.43 ± 9.66), presented to the general surgery department with different complaints such as (breast or axillary lump or inflammatory changes), while exclusion criteria were patients with BI-RADS (I OR II), any previous treatment affecting the results of the study or contraindications to do MRI study (e.g., pacemakers or contrast allergy or claustrophobia).
The study was approved by the local ethical committee of our institution. The patients were informed about the nature of the study, and informed consent was taken before the study. Full clinical history was taken (menopause, day of last menstrual cycle, pregnancy, breast feeding), family history of breast cancer. Pre-examination assessment of serum creatinine was done.
From the 35 patients, six patients were excluded ((1 was unfit for surgical interference, 2 DW-MRI was not completed (incomplete inclusion of axilla in the field of view of DWI), 1 with sub centimetric lymph nodes (long axis < 0.6 cm) and 2 for bad-quality images because of motion artifacts)).
In the study, we included 35 axillae from 29 patients with 44 lymph nodes (23with 1 axilla while 6 from both axillae). We included the most suspicious one or two lymph nodes on the same side of the breast lesion. Suspicious criteria were (long axis more than or equal to 0.8 cm, short axis more than or equal to 0.6 cm, lost hilum, focal cortical thickness).
After MRI examination (2 weeks range from 2 to 15 days), all the patients with malignant criteria either had axillary lymph node biopsy or surgical clearance) with close follow-up with imaging for indeterminate or benign looking lesions.
The technique of MRI and DWI
The study was performed with high-field strength 1.5 t MR system (Ingenia; Philips Medical Systems, Best, the Netherlands), using dedicated breast coil.
The premenopausal women were examined on days 6–13 of the menstrual cycle in order to reduce the risk of false positive.
Patient preparation
All patients were examined in the prone position allowing both breasts to naturally hang inside the loop of coil. We ensured that both breasts were fit entirely within the coil.
MRI protocol
The parameters used were as follows:
-
(a)
T2-weighted fast spin echo sequence (TR = 4000 ms, TE = 120 ms) in axial and sagittal planes with slice thickness = 3 mm, matrix = 256 × 160, flip angle = 90° and FOV = 34 × 34 cm.
-
(b)
T1-weighted FSE (TR = 540 ms, TE = 10 ms) in axial plane with slice thickness = 3 mm, matrix = 256 × 160, flip angle = 90° and FOV = 34 × 32 cm.
-
(c)
STIR sequence (TR = 5000 ms, TE = 100 ms) in axial plane with slice thickness = 3 mm, matrix = 256 × 160, flip angle = 90° and FOV = 34X32CM.
-
(d)
DW sequences in axial orientation with TR = 10,036 ms, TE = 80 ms, slice thickness = 3 mm, matrix = 256 × 256 with b-value (0 and 750 s/mm2\().\)
-
(e)
Dynamic contrast series were performed using six series of 3D (T1 High-Resolution Isotropic Volumetric Examination) THRIVE acquisition. One sequence before and five after injection of 0.1–0.2 mmol/kg body weight of gadolinium chelate contrast medium (Dotarem, Guerbet). Rate of injection was 10 ml per 15 s followed by saline flush (nearly at 1.5, 3, 4.5, 6 and 7.5 min) with parameters TR = 8.34, TE = 4.6 ms and slice thickness = 1.5 mm, flip angle = 12 and FOV = 35.
-
(f)
Delayed post-contrast fat-suppressed sequence; all post-contrast acquisitions were performed in the axial plane.
Image analysis
All magnetic resonance images were reviewed by two different radiologists (of 5 and 7 years’ experience); both were blinded to the final histopathological results. The first suspicious morphological criteria of ipsilateral lymph node metastasis were lost hilum. If there was no loss of hilum, then attenuated, eccentric hilum or focal cortical thickness, irregular outlines, decreased L/S ratio were considered as suspicious criteria.
STIR was used as an anatomical reference to rule out misidentification of blood vessels.
Qualitative assessment on the DW-MRI and corresponding ADC map images were evaluated at (0 and 750 b-values), classified into restricted diffusion (high or intermediate SI on DW-MRI and dropped on corresponding ADC map) or not restricted.
Quantitative assessment of the mean ADC values was done by manual drawing of ellipse (ROI) in the selected lymph node avoiding the hilum and margins as much as possible, three measurements were taken and the average of the three was recorded and expressed as the mean ± standard deviation.
Histopathological evaluation
Pathological confirmation of examined LNs was performed using US-guided needle biopsy, SLNB (sentinel lymph node biopsy) or axillary LN dissection and interpreted by two expert pathologists who were blinded to the results of MRI. Correlation between the DWI and ADC findings and pathological reports of these selected LNs was performed.
Statistical analysis
Data obtained by MRI and histopathology were collected and compared. Statistical analyses were performed by using SPSS 15.0.1 for windows; SPSSINC. Lesions were classified into benign and malignant according to sonomammography BI-RADS. Selected patients then proceeded to MRI examination. The mean size, L/S axis mean ADC values were compared among benign and malignant axillary lymph nodes using Chi-square test. Clinical efficiency indicators (sensitivity, specificity, positive and negative predictive values) were calculated for DWI and ADC referring to the gold standard. The cut-off value of ADC was calculated using ROC curve analysis to differentiate benign from malignant axillary lymph nodes. P value < 0.05 will be considered statistically significant.
Results
This study included 44 axillary lymph nodes from 29 patients with suspicious breast lesion on the same side (26 axillae with one lymph node and 9 with two lymph nodes). These nodes were evaluated by conventional MRI and DW-MRI to evaluate the role of DW-MRI and ADC in axillary lymph nodes discrimination. The histopathological results were the gold standard of reference, which revealed that 29 out of 44 examined nodes (65.0%) were malignant, while 15 nodes (34.1%) were benign.
Classification of examined axillary lymph nodes on DW-MRI was done according to diffusion restriction of the nodes and was correlated with pathology. The restricted nodes considered to be malignant while not restricted considered to be benign. There were 3 false positive LNs (proved to be benign on histopathology) and one false negative (proved to be malignant on histopathology). Accordingly, calculated sensitivity, specificity, PPV, NPV and accuracy were 96.6%, 80%, 90.3%, 92.3% and 90.9%, respectively, with P value < 0.001 (Table 1, Fig. 1).
The mean ADC value was significantly lower in malignant lymph nodes compared to benign nodes, measuring (0.68 ± 0.15) × 10−3 mm2/s ranging from (0.43–1.03) for malignant nodes while measuring (0.99 ± 0.26) × 10−3 mm2/s ranging from (0.46–1.65) for benign nodes.
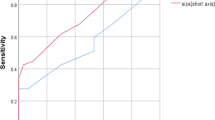
The calculated cut-off value of ADC to discriminate between malignant and benign axillary lymph nodes was (≤ 0.89 × 10−3 mm2/s) according to the ROC curve analysis AUC = 0.878 (84.3%). Accordingly, the sensitivity, specificity, PPV, NPV and accuracy were 89.66%, 86.67%, 92.9%, 81.2% and 87.8%, respectively, with P value < 0.001 (Table 2, Fig. 2).
The mean of long axis for malignant lymph nodes was (1.92 ± 0.79 cm) with a range of (1.03–4.87), while the mean of long axis for benign was (1.95 ± 0.74 cm) with a range of (1.11–3.61 cm), the mean of short axis for malignant nodes (1.26 ± 0.66 cm) with a range of (0.64–3.62) and for benign was (1.07 ± 0.29 cm) with a range of (0.66–1.67). Lastly the L/S ratio was (1.65 ± 0.58 cm) with a range (1–4.08) and (1.85 ± 0.57 cm) with a range (1.3–3.55) for malignant and benign axillary lymph nodes, respectively. No statistical significance was found between malignant and benign nodes for these three measurements with P value (0.901–0.291–0.272) for (long axis–short axis-L/S ratio), respectively.
In this study, hilum was preserved in 3 (10.3%) malignant nodes and 9 (60.0%) benign nodes, lost in 18 (62.1%) malignant and 4 (26.7%) benign nodes, eccentric in 5 (17.2%) malignant and 1 (6.7%) benign, attenuated 3 (10.3%) malignant and 1 (6.7%) benign. Lost hilum was statistically significant in discrimination between malignant and benign lymph nodes with P value (0.006) (Table 3).
Four benign lymph nodes with lost hilum as three nodes from two patients with granulomatous mastitis. The fourth benign lymph node according to histopathological examination with true cut needle biopsy for a patient performed the MRI breast with other imaging proved widespread metastasis from malignant breast mass.
DWI-MRI and ADC both can improve the role of MRI in detection of metastatic lymph nodes in breast cancer patients with no statistically significant difference found between our results and histopathological results especially when adding lost fatty hilum; however, no significant changes in the results could be added when we used the size measurements (Table 4).
Discussion
Recent studies have revealed that breast cancer has become one of the main causes of cancer-related death worldwide [7]. Treatment of breast cancer surgically involves both primary tumor surgical excision and axillary staging. While sentinel lymph node (SLN) biopsy in clinically node-negative patients replaced axillary lymph node dissection (ALND) [8]. Biopsy and ALND both are invasive methods that have long- and short-term complications on breast cancer patients and negatively affecting their life quality [4]. A definite classification of breast cancer patients for axillary surgery is of great significance for both treatment and prognosis [9].
Nowadays, a reduction in breast cancer mortality rate has been noticed especially in young women [10].
Axillary lymph node metastasis is considering one of the main factors, which affects the prognosis of the breast cancer patients, and 5-year survival for them has been changed accordingly to the nodal affection; for example, in negative LNs it measures 82.8%, while 73% in 1–3 positive nodes, 45.7%in 4–12 positive nodes and 28.4% in nodes diseased more than 13 positive one [11]. Pathological analysis for these nodes is still the gold standard for diagnosis [12]; however, about 40–70% of breast cancer patients have histopathological negative axillary lymph nodes, indicating that 40–70% of breast cancer patients undergo unneeded invasive procedure [13].
Diffusion-weighted magnetic resonance imaging (DW-MRI) is a non-contrast procedure, which measures the motion of water particles in vivo and analyzing microscopic tissue structure, membrane integrity, viscosity, cellularity fibers, tubules, macromolecules and organelles [14].
In this study, no significance for the age or the complaint of the patient with P value = 0.956 and 0.631, respectively, these results were in accordance with other studies [3, 15].
In this study, classification of examined axillary lymph nodes on DW-MRI was done according to diffusion restriction of the nodes, the restricted nodes were considered to be malignant (Fig. 3) while not restricted considered to be benign (Fig. 4), calculated sensitivity, specificity and accuracy were 96.6%, 80% and 90.9%, respectively, with P value < 0.001.
A 28-year-old female a, b T1W1 and STIR enlarged left axillary lymph node with eccentric hilum and increased SI in STIR. c, d increased SI in DW-MRI and dropped SI in ADC map with ADC value (0.761 × 10−3 mm.2/s) denoting restricted diffusion matching with metastasis proved by histopathological examination
These results were similar to previous studies [2, 4] with sensitivity, specificity and accuracy of (96%, 85% and 92%), respectively, for both of them, in spite of different numbers of examined lymph nodes (50 and 208 node) and different b-values (50, 400 and 800 s/mm2) and (0 and 1000 s/mm2), respectively. These results were matching with previous studies using 1.5 T breast MRI with sensitivity, specificity and accuracy ranging from (84–100%, 77–83.3% and 80–93%), respectively [16], excluding small lesions, which could not be evaluated on DWI due to the limitation of spatial resolution [17].
ADC is quantitative parameter, which is acquired by DW-MRI, and can exclude the T2 shine-effect providing quantitative assessment of water diffusivity in the target tissues making it easier to differentiate between lesions [2].
In the current study, we used ADC values (0 and 750 s/mm2); three measurements were taken at the highest b-value (750 s/mm2), the average of the three was recorded and expressed as the mean ± standard deviation, a significant difference between malignant and benign lymph nodes was noted.
The mean ADC value was significantly lower in malignant lymph nodes compared to benign nodes ranging from (0.43–1.03) × 10−3 mm2/s with a mean measuring (0.68 ± 0.15) × 10−3 mm2/s for malignant nodes (Fig. 5), while the range of benign nodes was (0.46–1.65) × 10−3 mm2/s with a mean measuring (0.99 ± 026) × 10−3 mm2/s (Fig. 6). Most of the previous studies concluded the same results such as [2, 3, 16, 18,19,20] on the other hand [21, 22] revealed that no significant difference was noted between metastatic and non-metastatic lymph nodes. Although in Bellie et al. study [21], all visualized lymph nodes (630 node from 42 patients) were included in the study, while Schipper et al. [22] used node per node analysis of 135 node from 50 patients.
A 66-year-old female a, b T1WI and STIR enlarged left axillary lymph node enlargement with lobulated outlines and lost hilum measuring (2.33 × 1.41 cm), c, d DW-MRI and color-coded ADC map revealed increased SI in DWI map and blue color, respectively, with ADC value (0.497 × 10−3 mm2/s) matching with malignant histopathological results
A 48-year-old female a T1WI enlarged right axillary lymph node with preserved hilum measuring (1.94 × 1.19 cm), b, c DW-MRI and ADC map revealed increased SI in both DWI and ADC map with ADC value (1.564 × 10−3 mm2/s), d color-coded ADC map displaying red color of examined lymph node matching with benign texture proved to be benign in histopathological examination
On the other hand, Kamitani et al. [23] revealed that ADC value was significantly high in metastatic than non-metastatic axillary lymph nodes mostly because they did not use node-by-node analysis for correlation between DW-MRI and histopathological results.
In this study, the calculated cut-off value of ADC to discriminate between malignant and benign axillary lymph nodes was (≤ 0.89 × 10−3 mm2/s) according to the ROC curve analysis AUC = 0.878 (84.3%). The nearest cut-off values to the cut-off value of this study were (0.90, 0.904, 0.95, 0.98, 1.09) × 10−3 mm2/s in the studies of [2,3,4, 17, 19], respectively, while the cut-off value of [7, 24] was (1.22 × 10−3 mm2/s) which was slightly increased than that of the current study. Accordingly, the sensitivity, specificity, PPV, NPV and accuracy were 89.66%, 86.67%, 92.9, 81.2% and 87.8%, respectively, with P value < 0.001. According to Rautiainen et al. [16], a wide range of cut-off value of ADC in previous studies was (0.889–1.351 × 10−3 mm2/s) mostly due to different b-values, MRI acquisition parameters [25].
In this study, there was an overlap between the ADC values of benign and malignant nodes; these results were explained by Wang and his team [26] as they found that some of the malignant LNs were not completely replaced by tumor cells, resulting in that some areas were free of metastasis in the same lymph node; on the other hand, in benign nodes diffusion of water molecules may be limited by inflammatory infiltration of the cell, reactive hyperplasia or proliferation of fibrous connective tissue resulting in decrease in ADC value (Fig. 7). A possible explanation for false-positive (inflamed enlarged nodes) motion leads to decrease ADC value [12].
A 54-year-old female a, b T1W1 and STIR revealed enlarged left axillary lymph node with focal cortical thickness measures (0.74 cm) c, d DW-MRI and ADC map revealed increased SI in DWI and dropped in ADC map with ADC value (0.607 × 10−3 mm.2/s) denoting restricted diffusion while pathology proved to be benign reactive lymph node (false positive)
Mortellaro et al. [27] study was the first to conclude that there was a significant correlation between the loss of fatty hilum and malignancy in axillary lymph nodes, and this agreed with our results; more recent studies proved the same such as [2,3,4, 24]. On the other hand, we had four benign lymph nodes with lost hilum and that could by explained as three nodes from two patients with granulomatous mastitis, and this was matching with Jeffery et al. [28] study, which concluded that granulomatous lymphadenitis are nonspecific and similar to metastatic nodes, as they are enlarged, rounded with lost hilum in mammographic and sonographic imaging. Another study from the University of Florida Shands Cancer Centre mentioned that although loss of fatty hilum in axillary lymph nodes correlated with spread of cancer but not all nodes with lost hilum necessarily were malignant [29]. The fourth benign lymph node according to histopathological examination with true cut needle biopsy for a patient performed the MRI breast with other imaging proved widespread metastasis from malignant breast mass, taking in consideration that the sensitivity of core needle biopsy is 82% and 88.2% [30, 31] and the axilla is the first site for metastasis for breast cancer we thought that it was malignant node due to the previous causes but as histopathology was our gold standard tool we mentioned it as benign in the results.
In the current study, we found no significant correlation between short axis in differentiation between malignant and benign lymph nodes (P value 0.291) in accordance with [2, 4, 24]. On the other hand [19, 32] found that lymph nodes with short axis more than 10 mm were a significant parameter in discrimination between benign and malignant lymph nodes.
In contrast to the current study, Chung et al. [19] concluded that the mean long axis of malignant axillary lymph nodes was significantly higher than benign nodes with (P value < 0.001), while in the current study there is no significant difference.
In this study, L/S ratio with (P value 0.272) was not significant and that was in accordance with previous study [2] while other study [3] concluded that the L/S ratio was significantly different between benign and malignant nodes.
In this study, we concluded that a combination of DW-MRI, ADC and lost fatty hilum all together increases the diagnostic accuracy of the MRI examination; these results were matched with other previous studies [2, 23], decreasing the need for contrast injection on the other, when size criteria were added, the diagnostic accuracy was not increased and that better results were added and that was in accordance with [2, 33].
Strength points of the study
We included patients with BI-RADS III, IV and V with evidence of lymphadenopathy to avoid bias. We were blinded to the results of histopathological examination. We used node-by-node analysis not patient by patient, we tried to correlate every examined node with pathological results according to morphological criteria in both. We used b-value (750 s/mm) to obtain good spatial resolution and adequate DW-MRI sensitivity.
Limitations
This study had some limitations, the first was relatively small-sized sample because of motion artifact and suboptimal visualization of the axilla due to obesity or uncomfortable position. The second was exclusion of sub-centimetric axillary lymph nodes, which could not assessed perfectly by usually used 1.5-T MRI.
Recommendations
Large-size sample will increase the accuracy of the examination.
Using 3-T breast MRI could improve the detection of sub-centimetric nodes and increasing the sensitivity of the examination.
Using chest coil with supine position and abducted arms can overcome obesity or uncomfortable position [3]
Conclusions
The combination of DW- MRI and ADC increase the sensitivity and accuracy in discrimination between benign and malignant axillary lymph nodes, especially when adding lost fatty hilum to the diagnostic criteria.
Availability of data and materials
The data and material used in this study are available.
Abbreviations
- DW-MRI:
-
Diffusion-weighted magnetic resonance imaging
- ADC:
-
Apparent diffusion co-efficient
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ROC curve:
-
Receiver operating characteristics curve
- LNs:
-
Lymph nodes
- DCE-MRI:
-
Dynamic contrast-enhanced MRI
- SPAIR:
-
Spectral selective attenuation inversion recovery
- STIR:
-
Short-time inversion recovery
- TSE:
-
Turbo spin echo sequence
- SE-EPI:
-
Spin echo-echo planer imaging
- L/S ratio:
-
Long-to-short-axis ratio
- AUC:
-
Area under the curve
- CE-FS- T1W1:
-
Contrast-enhanced fat-suppressed T1-weighted image
- ALND:
-
Axillary lymph node dissection
- SI:
-
Signal intensity
References
Jessing C, Langhans I, Jensen MB, Talman ML, Tvedskov TV, Kroman N (2018) Axillary lymph node dissection in breast cancer patients after sentinel node biopsy. ACTA Oncol 57:166–169. https://doi.org/10.1080/0284186x.2017.1401227
Zaiton F, Shehata SM, Warda MHA, Alekrashy MA (2016) Diagnostic value of MRI for predicting axillary lymph nodes metastasis in newly diagnosed breast cancer patients: diffusion-weighted MRI. Egypt J Radiol Nucl Med 47(2):659–667. https://doi.org/10.1016/j.ejrnm.2016.03.008
Elmesidy DS, Badawy EAMO, Kamal RM, Khalaf ESE, AbdelRahman RW (2021) The additive role of diffusion-weighted magnetic resonance imaging to axillary nodal status evaluation in cases of newly diagnosed breast cancer. Egypt J Radiol Nucl Med. https://doi.org/10.1186/s43055-021-00480-7
Hasanzadeh F, Faeghi F, Valizadeh A, Bayani L (2017) Diagnostic value of Diffusion Weighted Magnetic Resonance Imaging in evaluation of metstatic axillary lymph nodes in a sample of Iranian women with breast cancer. APJCP 18:1265–1270. https://doi.org/10.22034/APJCP.2017.18.5.1265
Durer Subasi I (2019) DW-MRI of the breast: a pictorial view. Insights Imaging 10:61. https://doi.org/10.1186/s13244-019-0745-3
Ismail AA, Hasan DI, Alshakor A (2014) Diagnostic accuracy of apparent diffusion coefficient value in differentiation metastatic from benign axillary lymph nodes in cancer breast. Egypt J Radiol Nucl Med 45(3):1011–1016. https://doi.org/10.1016/j.ejrnm.2014.06.003
Siegel RI, Miller KD, Jemal A (2018) Cancer statistics. CA Cancer J Clin 68:7–30. https://doi.org/10.3322/caac.21442
Dutta SW, Volaric A, Morgan JT, Chinn Z, Athins KA, Janowski E-M (2019) Pathological evaluation and prognostic implications of nodal micrometastasis in breast cancer. Semin Radiat Oncol 29(2):102–110. https://doi.org/10.1016/j.semradonc.2018.11.001
Nieciecki M, Dobruch-Sobczak K, Wareuk P, Guminska A, Bialek E, Cacko M, Krolicki L (2016) The role of ultrasound and lymphoscintigraphy in the assessment of axillary lymph nodes in patients with breast cancer. J Ultrasonography 16(64):5–15. https://doi.org/10.15557/JoU.2016.0001
Autier P, Boniol M, La Vecchia C, Vatten L, Gavin A, Hery C (2010) Disparities in breast cancer mortality trends between 30 European countries: retrospective trend analysis of WHO mortality database. BMJ 341:c3620. https://doi.org/10.1136/bmj.c3620
Li C, Meng S, Yang X, Wang J, Hu J (2014) The value of T2* in differentiation metastatic from benign axillary lymph nodes in patient with breast cancer—a preliminary in vivo study. PLoS ONE 9(1):e84038. https://doi.org/10.1371/journal.pone.0084038
He N, Xie C, Wei W, Pan C, Wang W, Lv N, Wu P (2012) A new preoperative MRI-based scoring system for diagnosing malignant axillary lymph nodes in women evaluated for breast cancer. Eur J Radiol 81(10):2602–2612. https://doi.org/10.1016/j.ejrad.2012.03.019
Zhou P, Wei Y, Chen G, Guo L, Yan D, Wang Y (2018) Axillary lymph node metastasis detection by magnetic resonance imaging in patients with breast cancer: a meta-analysis. Thorac Cancer 9(8):989–996. https://doi.org/10.1111/1759-7714.12774
Durur SI, Durur K, Karaman A, Seker M, Dernirci E, Alper F (2016) Is the necrosis/wall ADC ratio useful for the differentiation of benign and malignant breast lesions? Br J Radiol 90(1073):0803. https://doi.org/10.1259/bjr.20160803
Ashturkar AV, Pathak GS, Deshmukh SD, Pandave HT (2011) Factors predicting the axillary lymph node metastasis in breast cancer: is axillary lymph node clearance indicated in every breast cancer patients? Indian J Surg 73(5):331–335. https://doi.org/10.1007/s12262-011-0315-5
Rauitiainen S, Kononen M, Sironen R, Masarwah A, Sudah M, Hakumaki J, Vanninen R, Sutela A (2015) Preoperative axillary staging with 3.0-T breast MRI: clinical value of diffusion imaging and apparent diffusion coefficient. PLoS ONE 10(3):e0133111. https://doi.org/10.1371/journal.pone.0122516
Guvenc I, Whitman GJ, Liu P, Yalniz C, Ma J, Dogan BE (2019) Diffusion-weighted MR imaging increases diagnostic accuracy of breast MR imaging for predicting axillary metastasis in breast cancer patients. Breast J25:47–55. https://doi.org/10.1111/tbj.13151
Basara I, Orguc S, Coskun T (2013) The role of diffusion weighted imaging in the assessment of axillary lymph nodes. J Breast Health 9:76–81. https://doi.org/10.5152/tjbh.2013.08
Chung J, Youk JH, Kim JA, Gweon HM, Kim EK, Ryu YH, Son EJ (2014) Role of diffusion-weighted predicting axillary lymph node metastasis in breast cancer. Acta Radiol 55:909–916. https://doi.org/10.1177/0284185113509094
Yamaguchi K, Schacht D, Nakazono T, Irie H, Abe H (2015) Diffusion weighted images of metastatic as compared with non metastatic axillary lymph nodes in patients with newly diagnosed breast cancer. J Magn Reason Imaging 42:771–778. https://doi.org/10.1002/jmri.24829
Belli P, Bufi E, Buccheri C, Rinaldi P, Giulian M, Romani M, Fabrizi G, D’Angelo A, Brunelli C, Mule A, Franceschini G, Colosimo C (2017) Role of DWI assessing nodal involvement and response to neoadjuvant chemotherapy in advanced breast cancer. Eur Rev Med Pharmacol Sci 21(4):695–705
Schipper RJ, Paiman ML, Beets-Tan RG, Nelemans PJ, De Vries B, Heuts EM, Van De Vuver KK, Keymeulen KB, Brans B, Smidt ML, Lobbes MB (2015) Diagnostic performance of dedicated axillary T2- and diffusion weighted MR Imaging for nodal staging in breast cancer. Radiology 275:345–355. https://doi.org/10.1148/radiol.14141167
Kamitani T, Hatakenaka M, Yabuuch H, Matsuo Y, Fujita N, Jinnouchi M, Nagao M, Shirahane K, Tokunaga E, Honda H (2013) Detection of axillary node metastasis using diffusion-weighted MRI in breast cancer. Clin Imaging 37(1):56–61. https://doi.org/10.1016/j.clinimag.2012.02.014
Hussein MT, Ahmed BM, Qenawy OK, Ali AH, Omar EMA (2021) The role of diffusion-weighted imaging MRI in differentiation between benign and malignant axillary lymphadenopathy in clinical TNM stages I and II breast cancer. JCMRP 6(3):257–263. https://doi.org/10.4103/JCMRP.JCMRP_74_20
Zhang F, Zhu L, Huang X, Chen X (2013) Differentiation of reactive and tumor metastatic lymph nodes with diffusion-weighted and SPIO-enhanced MRI. MOI Imaging Biol 15(1):40–47. https://doi.org/10.1007/s11307-012-0562-2
Wang J, Liao Q, Zhang Y, Yu C, Bai R, Sun H (2012) Differential diagnosis of axillary inflammatory and metastatic lymph nodes in rabbit models by using diffusion-weighted imaging compared with conventional magnetic resonance imaging. Korean J Radiol 13(4):458–466. https://doi.org/10.3348/kjr.2012.13.4.458
Mortellaro VE, Marshall J, Singer L, Hochwald SN (2009) Magnetic resonance imaging for axillary staging in patients with breast cancer. J Magn Reason Imaging 30(2):309–312. https://doi.org/10.1002/jmri.21802
Illman JE, Terra SB, Clapp AJ, Hunt KN, Fazzio RT, Shan SS, Glazebrook KN (2018) Granulomatous diseases of the breast and axilla: radiological findings with pathological correlation. Insight Imaging 9:59–71. https://doi.org/10.1007/s13244-017-0587-9
Grobmyer S (2009) Breast MRI study suggests it may not be lymph node size that signals metastasis. Oncol Times 31(17):14. https://doi.org/10.1097/01.COT.0000360984.14035.0a
Rao R, Lilley L, Andrews V, Radford L, Ulissey M (2009) Axillary staging by percutaneous biopsy: sensitivity of fine-needle aspiration versus core needle biopsy. Ann Surg Oncol 16(5):1170–1175. https://doi.org/10.1245/s10434-009-0421-9
Rautiainen S, Masarwah A, Sudan M, Sutela A, Pelkonen O, Joukainen S, Sironen R, Kärjä V, Vanninen R (2013) Axillary lymph node biopsy in newly diagnosed invasive breast cancer: comparative accuracy of fine-needle aspiration biopsy versus core-needle biopsy. Radiology. https://doi.org/10.1148/radiol.13122637
Razek AA, Lattif MA, Denewer A, Farouk O, Nada N (2016) Assessment of axillary lymph nodes in patients with breast cancer with diffusion-weighted MR imaging in combination with routine and dynamic contrast MR imaging. Breast Cancer 23(3):525–532. https://doi.org/10.1007/s12282-015-0598-7
Kvistad KA, Rydland J, Smethurst HB, Lundgren S, FjØsne HE, Haraldseth O (2000) Axillary lymph node metastasis in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol 10(9):1464–1471. https://doi.org/10.1007/s003300000370
Acknowledgements
Not applicable.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
AZ collected the patients’ data and wrote the manuscript. RM revised the data and analyzed it. AH participated in the design of the study. AS interpreted the data collected and performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Ain Shams University ethical and scientific committee “The committee’s reference number is not available”. A written informed consent is obtained from all patients before the procedure.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Competing interests
There are no competing interests in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zahran, A.M.H., Maarouf, R.A., Hussein, A. et al. The role of diffusion-weighted MR imaging in discrimination between benign and malignant axillary lymph nodes in breast cancer patients. Egypt J Radiol Nucl Med 53, 126 (2022). https://doi.org/10.1186/s43055-022-00801-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00801-4