Abstract
Background
In cases of papillary thyroid carcinoma (PTC), lymph nodes are a typical site of metastasis. Extrathyroidal tissue involvement in differentiated thyroid carcinoma causes the disease to progress and affects the patients’ treatment options. Papillary thyroid carcinoma (PTC) is the common type in differentiated thyroid carcinoma (DTC), the other type is follicular thyroid carcinoma (FTC). Ectopic sites, such as intrathyroidal lymph node invasion in classical papillary thyroid malignancy, are extremely uncommon. It can be difficult to detect an intrathyroidal lymph node (ITLN) during a histopathological test, but it is important to do so since it affects the stage of the disease and subsequent treatment.
Case presentation
We present the case of a 63-year-old woman who presented with multinodular goitre and underwent total thyroidectomy. She was diagnosed with aberrant intrathyroidal lymph node metastases during pathological testing, resulting in an upgrade in treatment. Owing to the exceptionally unusual ectopic position of lymph node metastasis, in this case, there is a risk of diagnostic and therapeutic misinterpretation. This patient was treated with high-dose radioactive iodine in view of lymph node metastases.
Conclusions
Identification of ITLN by imaging characteristics is sometimes difficult, being often an intraoperative discovery and histopathological correlation that lead to upstage the disease and alter the final management.
Similar content being viewed by others
Background
Lymph nodes are a typical site of metastasis in cases of papillary thyroid carcinoma (PTC) [1]. Extrathyroidal tissue involvement in differentiated thyroid carcinoma causes the disease to progress and affects the patients’ treatment options [2]. Ectopic sites, such as intrathyroidal lymph node invasion in classical papillary thyroid malignancy, are extremely uncommon [3]. It can be difficult to detect an intrathyroidal lymph node (ITLN) during a histopathological test, but it is important to do so since it affects the stage of the disease and subsequent treatment as demonstrated in this case.
Case presentation
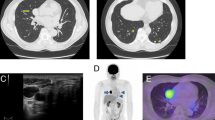
A 63-year-old woman had been suffering from multinodular goitre for 6 months. One month prior to surgery, she began to experience obstructive symptoms. There had been no previous trauma. There was a large multinodular swelling over the anterior neck area on inspection. There were no other major clinical abnormalities found. Ultrasound of the thyroid was performed and showed multiple well-defined anechoic lesions with the largest seen at the left thyroid measures 2.7 × 4.3 × 4.3 cm (AP × W × CC). Hypoechoic lesion at right thyroid measures 1.3 × 1.5 × 2.3 cm (AP × W × CC). Subsequently, she underwent CT scan. Multiple nodules were seen inside the thyroid nodule on a CT scan of the neck and thorax, with the largest nodule measuring 4.4 × 3.4 × 6.4 cm (AP × W × CC) in the left thyroid lobe. This nodule is heterogeneous, with a mixture of solid and cystic components. Another large nodule is seen at the right thyroid lobe extending to the isthmus measuring 1.9 × 1.9 × 3.1 cm (AP × W × CC) (Fig. 1).
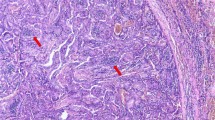
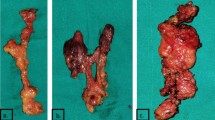
The patient underwent a complete thyroidectomy. The histopathological examination revealed a tumour forming papillary architecture with nuclear clearing, grooving and intranuclear cytoplasmic inclusion within the right thyroid and confirmed a diagnosis of classical papillary thyroid cancer with intrathyroidal lymph node infiltration (N1a). (Fig. 2). The left thyroid exhibited nodular hyperplasia with adenomatous nodule. Postoperatively, the patient shows serum thyroglobulin of 14.91ug/L and had increased to a level within their respective normal limits. She was treated with high-dose radioiodine ablation (120mci) with tyrosine suppression and serum thyroglobulin monitoring (Fig. 3). Post-ablation scan revealed iodine avid functioning thyroid tissue in the neck. She was planned for a diagnostic whole-body scan in 6 month time with continuation of TSH suppression therapy. Her serum thyroglobulin two months after therapy was < 0.04ug/L which is normal.
Histopathological examination. a A total thyroidectomy with nodular appearance. b Section from the right thyroid shows a well-demarcated tumour area with partly encapsulated (arrow) exhibiting tumour in papillary patterns. (H&E, × 40). c The tumour cells with classical features of papillary thyroid carcinoma showing papillae with fibrovascular core, nuclear clearing and grooving. (H&E, × 400). d A well-encapsulated intrathyroidal lymph node with tumour cells infiltration. The tumour cells forming thyroid follicles containing a dense eosinophilic colloid. (H&E, × 100)
Discussion
The presence of abnormal histological elements within the intact thyroid gland has only been recorded in very few cases. In addition to distant metastases to the thyroid, a number of ectopic tissue rests and unusual cysts have been described within the thyroid gland [4, 5]. In this article, we explain the existence of a true intrathyroidal lymph node which is the second case of papillary thyroid cancer with intrathyroidal lymph node metastasis. The first case was reported by Shawky [6] in 2017, a 63-year-old female in New Zealand with suspicious for Hurthle cell neoplasm versus oncocytic variant of papillary thyroid cancer. PTC metastases were indicated by papillae and nests of atypical polyhedral cells with vesicular nuclei, inclusions, and grooves intranodally.
The thyroid gland is made up of follicles, which produce colloid and are surrounded by follicular cells, calcitonin-producing parafollicular cells, also known as C-cells, a delicate connective tissue stroma, and vascular elements [7]. Any other histological elements found within the thyroid gland are abnormal. Non-metastatic and metastatic are two types of abnormal intrathyroidal tissue. Ectopic rests of non-thyroid tissue or irregular cysts are both thought to be the product of dysembryogenesis in non-metastatic intrathyroidal tissue. Intrathyroidal metastasis, on the other hand, often means spread from a distant primary malignancy [8].
While the presence of LN tissue within the parotid gland is a common occurrence [9], a similar finding within the thyroid is extremely uncommon, having only been identified once in a 40-year-old Egyptian woman with multinodular goitre [10]. To the best of our knowledge, this is the second case of a metastatic intrathyroidal LN that has been identified. The finding is not lymphocytic infiltration of the thyroid parenchyma; rather, they are a true LN with germinal centres and an intact capsule, lying entirely inside thyroid tissue and displaying features of papillary thyroid carcinoma metastasis. A divergence from the standard developmental phase may be one reason for such findings [11]. During the 8–9th weeks of pregnancy, there may be abnormal extension of the Juglo-axillary lymph sacs or abnormal sprouting of the lymphatic primordials in the cervical area. Since the presence of an intrathyroidal LN may cause the FNAC to contain lymphocytes and be misinterpreted as Hashimoto’s disease or lymphoma, routine sonographic guidance for all FNACs, including well palpable nodules, is important [12]. The presence of a metastatic intrathyroidal LN, with small differentiated thyroid cancer as in our case, should be regarded as N1a if the neck is node negative. However, according to the updated American Thyroid Association 2009 recommendations, this will otherwise up-stage the disease to stage III in patients older than 45 years, potentially affecting the prognosis and management plan [13].
Thyroid metastasis appears to be uncommon, with a prevalence of 5.5% among patients who had their thyroids removed for cancer [14]. Between 2000 and 2010, thyroid metastases from renal cell carcinoma accounted for 48.1 per cent of non-thyroid malignancies (NTMs) metastases to the thyroid gland, with a proclivity to spread into the jugular veins [15]. Renal cell carcinoma, breast cancer, and lung cancer are the most common primary tumour sites; however, there is no complete agreement on which cancers most frequently metastasize to the thyroid, as this depends on many factors such as the epidemiology and clinical behaviour of the primary cancer, as well as the diagnostic methods used [16]. Thyroid metastasis can pose both diagnostic and therapeutic challenges. It is possible that the metastatic focus is very limited and clinically undetectable. In 50 to 60% of patients with no palpable nodules, incidental thyroid nodules are discovered at post-mortem [17]. Furthermore, it has been reported that the delay between the diagnosis of the primary cancer and the thyroid secondary has been as long as 26 years [18]. The presence of metastatic lesions in the thyroid gland is a bad omen in terms of prognosis, with patients dying shortly after the diagnosis of thyroid gland metastasis is made [14]. As a result, any thyroid nodule in a patient with a history of cancer should be treated with caution and extensively examined using FNA, preferably in combination with immunohistochemistry and sonography [12].
Conclusions
Thyroid glands can contain abnormal non-metastatic histological elements, which are uncommon. When assessing a thyroid nodule with atypical radiological and cytological characteristics, this should be taken into account. Within the thyroid gland, a true lymph nodal structure may occur, and papillary thyroid cancer metastasis can influence it. Because of their rarity, the pathophysiology of some of these abnormal tissues is unknown, and further research is required. Since thyroid metastasis can occur decades after the primary cancer has been detected, any thyroid nodule in a patient with a history of cancer should be thoroughly investigated. The presence of a metastatic intrathyroidal LN in differentiated thyroid cancer potentially affecting the prognosis and management plan.
Availability of data and materials
All the data and materials pertaining to this case report were obtained from patient’s electronic and medical records of our institutions. All data used during this case report are included in this published article.
Abbreviations
- PTC:
-
Papillary thyroid carcinoma
- ITLN:
-
Intrathyroidal lymph node
- DTC:
-
Differentiated thyroid carcinoma
- FTC:
-
Follicular thyroid carcinoma
References
Maksimovic S, Jakovljevic B, Gojkovic Z (2018) Lymph node metastases papillary thyroid carcinoma and their importance in recurrence of disease. Med Arch (Sarajevo, Bosnia Herzegovina) 72(2):108–111
Schmidbauer B, Menhart K, Hellwig D, Grosse J (2017) Differentiated thyroid cancer—treatment: state of the art. Int J Mol Sci 18(6):1–17
Agosto-Vargas Y, Gutiérrez M, Martínez JH, Mangual-Garcia M, Palermo C, Vélez-Maymi S et al (2017) Papillary thyroid carcinoma: ectopic malignancy versus metastatic disease. Case Rep Endocrinol 2017:1–3
Chung EJ, Baek SK, Youn SW, Kim CH, Lee JH, Jung KY (2010) A case of bilateral intrathyroidal branchial cleft cyst in a newborn. J Pediatr Surg 45(1):e1-4. https://doi.org/10.1016/j.jpedsurg.2009.09.038
Arsheed Hussain H, Hassaan J, Hima Bindu R, Fozia JW (2020) Intrathyroidal thyroglossal duct cyst presenting as chronic thyroiditis: case report and narrative review of the literature. Int J Clin Endocrinol Metab 6:017–021
Shawky MS, Meyer-Rochow W (2017) Aberrant intrathyroid tissue: a report of intrathyroid lymph node metastasis and a review of literature. Indian J Surg 79(2):148–152
Khan YS, Farhana A. Histology, Thyroid Gland. In: Histology, Thyroid Gland. StatPearls Publishing; 2021 [cited 2021 Aug 10]. https://www.ncbi.nlm.nih.gov/books/NBK551659/
Okstad S, Mair IWS, Sundsfjord JA, Eide TJ, Nordrum I (1986) Ectopic thyroid tissue in the head and neck. J Otolaryngol 15(1):52–55
Bialek EF, Fakubowski W, Zajkowski P, Szopinski KT, Osmolski A (2006) US of the major sali- vary glands: anatomy and spatial relation-ships. Pathol Cond Pitfalls 1:745–764
Cameselle-Teijeiro J, Varela-Durán J. Intrathyroid salivary gland-type tissue in multinodular goiter. Vol. 425, Virchows Archiv. 1994. p. 331–4.
Zadvinskis DP, Benson MT, Kerr HH, Mancuso AA, Cacciarelli AA, Madrazo BL et al (1992) Congenital malformations of the cervicothoracic lymphatic system: embryology and pathogenesis. Radiographics 12(6):1175–1189
Yoon JH, Kim E-K, Kwak JY, Moon HJ, Kim GR (2013) Sonographic features and ultrasonography-guided fine-needle aspiration of metastases to the thyroid gland. Ultrasonography 33(1):40–48
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133
Nachiappan AC, Metwalli ZA, Hailey BS, Patel RA, Ostrowski ML, Wynne DM (2014) The thyroid: review of imaging features and biopsy techniques with radiologic-pathologic correlation. Radiographics 34(2):276–293
D’Angelo F, Magistri P, Antolino L, Socciarelli F, Olivieri T, Canegallo F et al (2016) Metastases from renal cell cancer to the thyroid gland: a systematic review of 175 cases between 1964 and 2016. Lung 19(2):32.8
Zhou L, Chen L, Xu D, Shao Q, Guo Z, Ge M (2017) Breast cancer metastasis to thyroid: a retrospective analysis. Afr Health Sci 17(4):1035–1043
Jin J, McHenry CR (2012) Thyroid incidentaloma. Best Pract Res Clin Endocrinol Metab 26(1):83–96
Nguyen QT, Lee EJ, Huang MG, Park YI, Khullar A, Plodkowski RA (2015) Diagnosis and treatment of patients with thyroid cancer. Am Heal Drug Benefits 8(1):30–38
Acknowledgements
The authors would like to thank the patient and his family members for providing informed consent to allow the use of his anonymized clinical data and images for the purpose of knowledge sharing and publication.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
WMNWZ, WFWAR, NSS and NMN were involved in the interpretation of imaging findings and initial management of the patient. MMY was involved in the subsequent surgical management as well as the consent taking from patient and family members. NMN was responsible for proofreading the manuscript writing. All authors contributed significantly to the manuscript writing and all authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Verbal informed consent was obtained from the patient to participate in this case report.
Consent for publication
A written consent has been obtained and is available upon request by the Editors. The images presented do not compromise the patient’s anonymity.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wan Zainon, W.M.N., Wan Abdul Rahman, W.F., Yahya, M.M. et al. Aberrant intrathyroidal lymph node metastasis in classical papillary thyroid carcinoma. Egypt J Radiol Nucl Med 52, 229 (2021). https://doi.org/10.1186/s43055-021-00614-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00614-x