Abstract
Background
Volumetric analysis is a novel radiological technique used in the measurement of target lesions in three dimensions in order to estimate the lesion’s volume. Recently, it has been used for evaluation of the remaining liver volume after partial hepatectomy and also for evaluation of the response of tumours to treatment. It has been proven to be more accurate than the standard one or two-dimensional measurements, and it is especially useful for the evaluation of complex tumours after radiological interventional methods when the use of standard methods is limited. In the current study, our aim was to evaluate the value of the three-dimensional (3D) volumetric method “Response Evaluation Criteria in Solid Tumours (vRECIST)” and to compare it with the non–three-dimensional methods (RECIST) and modified RECIST (mRECIST) in the assessment of the therapeutic response of hepatocellular carcinoma (HCC) after transarterial chemoembolization (TACE).
Results
A retrospective study was conducted on 50 patients with confirmed radiological or pathological diagnosis of hepatocellular carcinoma (HCC) who underwent TACE as the only interventional procedure and follwed up by triphasic CT 1 and 4 months after treatment. The study revealed a significant difference between mRECIST and vRECIST in the assessment of the therapeutic response of HCC after TACE, a weak agreement was found between both methods in the detection of complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD). Also, there was no significant agreement between mRECIST and vRECIST regarding the assessment by classifying the patients into responders or nonresponders.
Conclusion
Volumetric analysis is an effective method for measuring the HCC lesions and evaluating its response to locoregional treatment with a significant difference between vRECIST and mRECIST in the assessment of therapeutic response, which in turn help the interventional radiologist to decide the future treatments and change the therapeutic plans. Based on these results, we recommend vRECIST to be an essential part of the assessment of therapeutic response after locoregional therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Hepatocellular carcinoma (HCC) is the commonest primary liver malignancy, second leading cause of cancer-related mortality and the fifth most common cancer in men and the seventh in women with over half a million cases diagnosed worldwide every year. Chronic viral hepatitis due to hepatitis B virus (HBV) or hepatitis C virus (HCV) accounts for the majority of HCC cases [1, 2].
Transplantation and resection remain the only potentially curative options; however, many patients present with either unresectable tumours or comorbidities eliminating these surgical treatment choices [3, 4].
Among the different staging systems for HCC, many have adopted the Barcelona Clinic Liver Cancer (BCLC) staging classification which recommends a treatment strategy according to the stage of the disease [5]. In most patients with intermediate or advanced stage of the disease, locoregional procedures like transarterial chemoembolization (TACE) could be the best therapeutic option. Proper radiological evaluation of the treatment response after TACE is crucial for further therapeutic decisions and plays a fundamental role in further management plans [6].
The Response Evaluation Criteria in Solid Tumours (RECIST) was introduced to assess the response of tumours to systemic chemotherapy by measurement of the tumour size. However, considering the fact that locoregional therapies induce tumour infarction and tissue necrosis without early changes in the size of the lesion is considered a main limitation to this method of assessment [2].
This deficiency in the RECIST system prompted the development of more suitable approaches for assessment of tumour response to therapy. The European Association for Study of the Liver (EASL) were then introduced and depends on measurement of the size of the viable enhancing tumour only in bidimensional method and hence reflecting the extent of tumour necrosis induced by the treatment procedure. More recently, modified Response Evaluation Criteria in Solid Tumours (mRECIST) criteria were introduced for further improvement of the EASL guidelines. mRECIST differs from EASL in just the measurement of the viable component should be done in the single long axis of the lesion [6].
The current one- and two-dimensional methods are limited by high inter and intra observer variability. The advent of new automated and semiautomated tumour segmentation methods has contributed to the shift away from one- and two-dimensional methods toward 3D quantitative image analysis [6].
The aim of our study was to compare the 2D methods (RECIST, mRECIST) with 3D quantitative method of the index tumour as a more accurate tool for evaluation of the response of HCC after TACE.
Methods
A retrospective study was conducted on 50 patients with confirmed diagnosis of hepatocellular carcinoma (HCC) who underwent TACE as the only interventional procedure which was done in the interventional unit, of the radiology department at our insitution; 47 patients were males, and 3 were females. The age ranges between 50 and 74 years with mean age of 61.68 years.
Inclusion criteria
The diagnosis of HCC was confirmed either histologically (by biopsy) or radiologically by the typical radiological features of HCC including two of the major features (arterial enhancment, delayed wash out and enhancing capsule). All patients were Child-Pugh A to B and BCLC class B.
Exclusion criteria
Patients excluded from this study included those with contraindications to the contrast medium, pregnancy, Child-Pugh score > B, patients with contraindications to hepatic embolization procedures (e.g. coagulopathy), patients with history of other malignant disease and patients who underwent other therpautic procedures.
An informed consent was obtained from all participants in this study before the TACE procedure. The study was approved by the local ethical committee. Privacy of all patient's data was strictly guaranteed.
From June 2017 to December 2017, 50 patients underwent intra-arterial therapy for hepatocellular carcinoma with either conventional TACE or TACE with drug-eluting beads. The follow-up CT was performed after 1 and 4 months. Images are transferred to the workstation (Vitrea Workstation, Toshiba) for image processing and volumetric analysis. The response of the index tumour on post TACE contrast-enhanced CT (Siemens16; Bayer Pharma AG, Germany) was assessed by two expericned radiologists in abdominal imaging with 20 and 15 years experince by comparing pre and post TACE CT images.
Treatment response was assessed on arterial phase images by using RECIST, mRECIST and volumetric RECIST methods. The percentage of tumour change (TC) was calculated using the equation:
where Mpre is the baseline tumour measurement before TACE and Mpost is the measurement at the post TACE CT imaging.
Patients were then classified into responders or nonresponders based on the percentage of TC. According to RECIST and mRECIST systems, a decrease by 30% or more was considered “responder”, while less than 30% tumour change was classified as “nonresponder”. There are no specific published guidelines for volumetric tumour response criteria, so we followed previous studies and used the same cutoff values of RECIST and mRECIST for the vRECIST system in order to simplify the response assessment. Using the formula V = 4/3πr3, where V is the volume, r is the radius, and π is the mathematical constant representing the ratio of a circle’s circumference to its diameter, the decrease of 65% in tumour volume is corresponding to a decrease of 30% in unidimensional methods (RECIST and mRECIST) [6].
Image processing
The number and location of the lesions were evaluated. Then using the axial plane, we draw the tumour contour, starting the process by the head or upper part of the lesion and end in the most caudal part. We measured the total volume of the lesion and also the volume of viable parts detected as arterially enhancing areas, and we measure the ratio viable/nonviable parts as a factor of response to the treatment. The software processes all the obtained cuts and represents the tumour in 3D method. The procedure took between 20 and 30 min.
Imaging analysis for quantification of the tumour necrosis and reduction of the tumour’s size
Tumour response by CT was evaluated on all patients 1 and 4 months after treatment, and the response of the tumour to treatment was categorized into four groups: complete response, partial response, stable disease, and progressive disease. Patients with complete and partial responses are corresponding to “responder group” while patients with stable and progressive disease are considered “nonresponders”. The cut-off values were determined by the extrapolation of RECIST—the extrapolation of the diameter of the lesion to the volume of lesion of a regular spherical shape, according the criteria in Table 1.
Statistical analysis
A statistical package software (SPSS) v.24 was used for data analysis. Chi-squared test was used for comparison of the different categorical data. Exact test was used if the expected frequency is < 5. Kappa measure of agreement was calculated to test agreement between methods [7]. Spearman correlation coefficient was used for correlation between the different quantitative variables with P value < 0.05 considered statistically significant.
Results
Both modified RECIST and volumetric RECIST methods of measurements were applied for each HCC lesion before and after TACE, then percentage of tumour change (TC) was calculated (Table 2). Then the lesions were classified according to their therapeutic response either: completer response (CR), partial response (PR), stationary disease (SD) and progressive disease (PD) following the criteria described previously in Table 1, and whether responder or nonresponder where CR and PR are considered responder and SD and PD are considered nonresponder.
According to the mRECIST method, there were 3 cases showing complete response (CR), 11 cases with partial response (PR), 35 cases with stationary disease (SD) and 1 case with progressive disease (PD), with overall 14 cases responders and 36 nonresponders. While assessment of the therapeutic response according to the vRECIST method revealed 3 cases with complete response (CR), 35 cases with partial response (PR), 11 cases with stationary disease (SD) and 1 case with progressive disease (PD), with overall 38 cases responders and 12 nonresponders (Table 3).
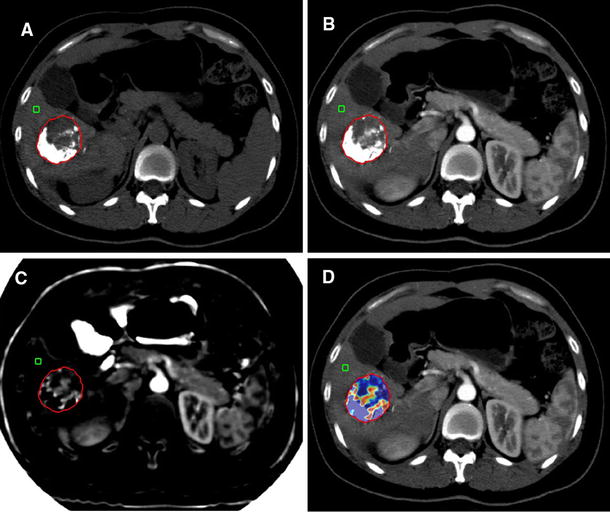
By statistical analysis of the abovementioned findings, there is a weak agreement between both methods mRECIST and vRECIST regarding assessment of the therapeutic response whether CR, PR, SD or PD (Table 4) (Figs. 1, 2, 3 and 4).
A 66-year-old male with hepatitis C cirrhosis complicated by development of right lobe HCC. Child Pugh Score: A. BCLB: B. A Pre-TACE axial arterial phase image showing measurement of the lesion according to RECIST, B pre-TACE axial arterial phase image showing measurement of the lesion according to mRECIST and C pre-TACE axial arterial phase image showing measurement of the lesion according to vRECIST. D vRECIST 3D image showing the lesion’s volume, E post-TACE images showing lesion’s measurement according to RECIST, F measurement according to mRECIST by measuring the diameter of the enhancing component only, G volumetric assessment of the viable component only, H 3D image showing the volume of the viable component, I vRECIST of the whole lesion post TACE, and J 3D image of the whole lesion’s volume. According to mRECIST, the lesion shows stable disease (non-responder) (< 30% decrease in the diameter of viable component), while according to vRECIST, the lesion shows partial response (responder) (> 65% decrease in the diameter of viable enhancing component). This could be explained by the heterogeneity of the lesion which makes it difficult to measure a single diameter of the enhancing component which is better assessed by 3D images
A 56-year-old male with hepatitis C cirrhosis complicated by development of right lobe HCC. Child Pugh Score: A. BCLB: B. A Pre-TACE axial arterial phase image showing measurement of the lesion according to RECIST, B pre-TACE axial arterial phase image showing measurement of the lesion according to mRECIST and C pre-TACE axial arterial phase image showing measurement of the lesion according to vRECIST, D vRECIST 3D image showing the lesion’s volume, E post-TACE images showing lesion’s measurement according to RECIST, F measurement according to mRECIST by measuring the diameter of the enhancing component only detected along the lateral margins of the lesion, G volumetric assessment of the viable component only, H 3D image showing the volume of the viable component, I vRECIST of the whole lesion post TACE, and J 3D image of the whole lesion’s volume. According to mRECIST, the lesion shows partial response (responder) (> 30% decrease in the diameter of viable component), and also according to vRECIST, the lesion shows partial response (responder) (> 65% decrease in the diameter of viable enhancing component)
A 67-year-old male with hepatitis C cirrhosis complicated by development of left lobe HCC. Child Pugh Score: A. BCLB: B. A Pre-TACE axial arterial phase image showing measurement of the lesion according to RECIST, B pre-TACE axial arterial phase image showing measurement of the lesion according to mRECIST and C pre-TACE axial arterial phase image showing measurement of the lesion according to vRECIST, D vRECIST 3D image showing the lesion’s volume, E post-TACE images showing lesion’s measurement according to RECIST, F measurement according to mRECIST by measuring the diameter of the enhancing component only during the arterial phase, G volumetric assessment of the viable component only, H 3D image showing the volume of the viable component, I vRECIST of the whole lesion post-TACE, and J 3D image of the whole lesion’s volume. According to mRECIST, the lesion shows stable disease (nonresponder) (< 30% decrease in the diameter of viable component), while according to vRECIST, the lesion shows partial response (responder) (> 65% decrease in the diameter of viable enhancing component)
A 67-year-old male with hepatitis C cirrhosis complicated by development of right lobe HCC. Child Pugh Score: B, BCLB: B. A Pre-TACE axial arterial phase image showing measurement of the lesion according to RECIST, B pre-TACE axial arterial phase image showing measurement of the lesion according to mRECIST and C pre-TACE axial arterial phase image showing measurement of the lesion according to vRECIST, D vRECIST 3D image showing the lesion’s volume, E post-TACE images showing lesion’s measurement according to RECIST, F measurement according to mRECIST by measuring the diameter of the enhancing component only, G volumetric assessment of the viable component only, H 3D image showing the volume of the viable component, I vRECIST of the whole lesion post-TACE, J 3D image of the whole lesion’s volume. According to mRECIST, the lesion shows stable disease (nonresponder) (< 30% decrease in the diameter of viable component) while according to vRECIST, the lesion shows partial response (responder) (> 65% decrease in the diameter of viable enhancing component)
On the other hand, there's no significant agreement between mRECIST and vRECIST regarding assessment of the therapeutic response whether responders or nonresponders (Table 5).
Accordingly, there's significant difference between mRECIST and vRECIST in the assessment of the therapeutic response whether responders or non-responders (P < 0.001).
Discussion
Transcatheter arterial chemoembolization (TACE) is the optimal treatment option for patients with intermediate stage HCC according to the BCLC staging system. The aim of palliative treatment options is to improve the survival without greatly impairing the quality of life [8]. The goal of imaging biomarkers used in the assessment of the tumour response is to early identify the nonresponder patients in order to allow for potential changes in therapeutic plans [6].
Our study showed a significant statistical difference between mRECIST and vRECIST in the assessment of therapeutic response after intra arterial therapy of HCC whether responders or non-responders. It is also noted that many lesions were diagnosed as stable disease (nonresponders) by mRECIST are classified as partial response (responders) by vRECIST which has a great impact on therapeutic planning and further management of the patients.
Several approaches used for the assessment of tumour response to treatment include RECIST, mRECIST and more recently vRECIST. RECIST and mRECIST are widely used methods but have some limitations when applied to TACE. In their current form, RECIST and mRECIST methods analyze the residual tumour only in the axial plane which gives numerous drawbacks as they are not accurate in lesions with inhomogeneous enhancement, asymmetric regression and multiple tumours [9, 10].
TACE may result in heterogenous tumour necrosis, and as a result, the change in tumour enhancement and tumour size may become heterogeneous and this could be explained by the fact that tumours are fed by multiple arteries that are not typically treated equally. This makes some limitation to the mRECIST method of tumour response assessment [11].
A large retrospective study done by Tacher et al. [6] was done to assess the HCC response after TACE using the uni and bidimensional (RECIST, mRECIST and EASL) versus quantitative three-dimensional methods (qEASL and vRECIST). The study was performed over 290 confirmed HCC cases that underwent TACE, and in line with our findings, they found a significant statistical difference between the responders and nonresponders group when using the three-dimensional-based criteria; on the other hand, no statically significant difference was found between responders and nonresponders groups when using the bidimensional methods. They concluded that 3D methods are the criteria of choice to predict patient survival after TACE as they clearly identify the nonresponders. This agrees with our findings.
A recent study done by Moawad et al. [12] was conducted over 42 HCC cases, and the tumour response assessment was done using the manual volumetric RECIST (M-vRECIST), automated volumetric RECIST (A-vRECIST) and the mRECIST criteria. They compared the diameter changes determined through the different methods. The correlation between tumour diameter measurement changes by mRECIST and M-vRECIST revealed a statistically significant difference between both methods (P < 0.001), and this goes in line with our results. Furthermore, they compared the M-vRECIST and A-vRECIST and found strong linear correlation between the two approaches.
Welsh et al. [13] performed a study over 17 patients with HCC who underwent liver transplantation. The tumour size and volume were assessed by the RECIST and the volumetric methods, then gross pathologic measurements after hepatectomy were analyzed for tumour volumes. They found that RECIST was significantly overestimated the tumour volume by an average of 28%, while volumetric methods of tumour volume measurement was similar to gross pathologic volume.
The assessment of therapeutic response of infiltrative type of HCC is challenging due to its indistinct borders. Previous studies showed high correlation between the volumetric measurement and the pathological tumour volume. Such studies demonstrate the superiority of volumetric assessment in estimation of the real tumour volume, which is more important during assessment of treatment response [13, 14].
Lencioni et al. [15] recommends 3D volumetric analysis to be a priority in future researches. Volumetric analysis of the tumour represents the entire volume of viable portion of the tumour rather than measurement in a single axial slice, and hence, vRECIST reduced the subjectivity of 2D methods; however, such method takes a longer time for assessment which is the major drawback for volumetric analysis of the tumours.
Volumetric measurement is also able to depict tumour size changes earlier than conventional 2D methods which is crucial in patients’ follow-up. It has already been demonstrated that histopathologic tumour response correlates better with tumour volume than with axial measurements. Varzaneh et al. [16] performed a retrospective study on 173 HCC lesions that underwent TACE and liver transplantation done for 53 patients. They found that Volumetric post-TACE CT may accurately predict tumour necrosis in treated HCC lesions and well correlated with pathological findings detected after liver transplantation. They found the Mean predicted tumour necrosis in the liver transplant group was 77.6%, while at pathology was 78.7% with a statistically significant correlation between radiologically predicted tumour necrosis and pathological necrosis (r = 0.871, p < 0.001).
Another study by Chapiro et al. [17] conducted on 17 patients with HCC who underwent TACE before surgery and followed up by 3D volumetric segmentation of target lesions by MR examination before orthotopic liver transplantation or surgical resection, and they found a very good agreement between radiologically predicted liver volume and that detected pathologically after surgery.
In line with our findings, Budjan et al. [18] performed a study over 22 HCC patients who underwent TACE and assessed by both vRECIST and mECIST pre- and post-TACE by MRI, and they found lower variability and overlap errors in measuring the entire tumour volume than by measuring the enhancing components.
The study has some limitations. It was a retrospective analysis with inherited limitations to such study design. This study involved selected patients with certain criteria which did not include some common lesions such as infiltrative HCC with portal vein thrombosis. Therefore, further researches including higher number of cases and variable types of tumours that underwent different therapeutic procedures are recommended. The main limitation of the vERCIST method is that it is a time-consuming technique which needs more time for volumetric measurement and image processing.
Conclusion
Volumetric analysis is an effective method for measuring the HCC lesions and evaluating its response to locoregional treatment with a significant difference between vRECIST and mRECIST in the assessment of therapeutic response, which in turn help the interventional radiologist to decide the future treatments and change the therapeutic plans. Based on these results, we recommend vRECIST to be an essential part of the assessment of therapeutic response after locoregional therapy.
Availability of data and materials
All the datasets used and analyzed in this study are available with the corresponding author on reasonable request.
Abbreviations
- BCLC:
-
Barcelona Clinic Liver Cancer
- CR:
-
Complete response
- EASL:
-
European Association for the Study of the Liver
- HCC:
-
Hepatocellular carcinoma
- mRECIST:
-
Modified Response Evaluation Criteria in Solid Tumours
- M-vRECIST:
-
Manual volumetric RECIST
- PD:
-
Progressive disease
- PR:
-
Partial response
- RECIST:
-
Response Evaluation Criteria in Solid Tumours
- SD:
-
Stable disease
- TACE:
-
Transcatheter arterial chemoembolization
- vRECIST:
-
Volumetric Response Evaluation Criteria in Solid Tumours
References
Metwally LI, Mahmoud BE, Yehia M (2019) The value of dynamic subtraction MRI technique in the assessment of treatment response of hepatocellular carcinoma to transcatheter arterial chemoembolization. Egypt J Radiol Nucl Med 50(1):1–13
Mahmoud BE, Gadalla AAEH, Elkholy SF (2021) The role of dynamic and diffusion MR imaging in therapeutic response assessment after microwave ablation of hepatocellular carcinoma using LI-RADS v2018 treatment response algorithm. Egypt J Radiol Nucl Med 52(1):1–10
Kooby DA, Egnatashvil V, Srinivasan S et al (2010) Comparison of yttrium-90 radioembolization and transcatheter arterial chemoembolization for the treatment of unresectable hepatocellular carcinoma. J Vasc Interv Radiol 21(2):224–230. https://doi.org/10.1016/j.jvir.2009.10.013
Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, Atassi B, Baker T, Gates V, Miller FH, Sato KT, Wang E, Gupta R, Benson AB, Newman SB, Omary RA, Abecassis M, Kulik L (2010) Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology 138(1):52–64. https://doi.org/10.1053/j.gastro.2009.09.006
Seinstra BA, Defreyne L, Lambert B, Lam MGEHH, Verkooijen HM, van Erpecum KJ, van Hoek B, van Erkel AR, Coenraad MJ, al Younis I, van Vlierberghe H, van den Bosch MAAJ (2012) Transarterial radioembolization versus chemoembolization for the treatment of hepatocellular carcinoma (TRACE): study protocol for a randomized controlled trial. Trials 13(1):144. https://doi.org/10.1186/1745-6215-13-144
Tacher V, Lin M, Duran R, Yarmohammadi H, Lee H, Chapiro J, Chao M, Wang Z, Frangakis C, Sohn JH, Maltenfort MG, Pawlik T, Geschwind JF (2015) Comparison of existing response criteria in patients with hepatocellular carcinoma treated with transarterial chemoembolization using a 3D quantitative approach. Radiology 278(1):275–284. https://doi.org/10.1148/radiol.2015142951
Chan YH (2003) Biostatistics 104: correlational analysis. Singap Med J 44(12):614–619
Subramaniam S, Kelley RK, Venook AP (2013) A review of hepatocellular carcinoma (HCC) staging systems. Chin Clin Oncol 2(4)
Lin M, Pellerin O, Bhagat N, Rao PP, Loffroy R, Ardon R, Mory B, Reyes DK, Geschwind JF (2012) Quantitative and volumetric EASL and RECIST: feasibility of a semi-automated software method to assess tumor response after transcatheter arterial chemoembolization (TACE). J Vasc Interv Radiol 23(12):1629–1637. https://doi.org/10.1016/j.jvir.2012.08.028
Edeline J, Boucher E, Rolland Y, Vauléon E, Pracht M, Perrin C, le Roux C, Raoul JL (2012) Comparison of tumor response by Response Evaluation Criteria in Solid Tumors (RECIST) and modified RECIST in patients treated with sorafenib for hepatocellular carcinoma. Cancer 118(1):147–156. https://doi.org/10.1002/cncr.26255
Lim HK, Han JK (2002) Hepatocellular carcinoma: evaluation of therapeutic response to interventional procedures. Abdom Imaging 27(2):168–179. https://doi.org/10.1007/s00261-001-0093-9
Moawad AW, Fuentes D, Khalaf AM, Blair KJ, Szklaruk J, Qayyum A, Hazle JD, Elsayes KM (2020) Feasibility of automated volumetric assessment of large hepatocellular carcinomas' responses to transarterial chemoembolization. Front Oncol 10:572. https://doi.org/10.3389/fonc.2020.00572
Welsh JL, Bodeker K, Fallon E, Bhatia SK, Buatti JM, Cullen JJ (2012) Comparison of response evaluation criteria in solid tumors with volumetric measurements for estimation of tumor burden in pancreatic adenocarcinoma and hepatocellular carcinoma. Am J Surg 204(5):580–585. https://doi.org/10.1016/j.amjsurg.2012.07.007
Reynolds AR, Furlan A, Fetzer DT, Sasatomi E, Borhani AA, Heller MT, Tublin ME (2015) Infiltrative hepatocellular carcinoma: what radiologists need to know. Radiographics 35(2):371–386. https://doi.org/10.1148/rg.352140114
Lencioni R, Crocetti L (2012) Local-regional treatment of hepatocellular carcinoma. Radiology 262(1):43–58. https://doi.org/10.1148/radiol.11110144
Varzaneh N, Pandey F, Ghasabeh A et al (2018) Prediction of post-TACE necrosis of hepatocellular carcinoma using volumetric enhancement on MRI and volumetric oil deposition on CT, with pathological correlation. Eur Radiol 28(7):3032–3040. https://doi.org/10.1007/s00330-017-5198-9
Chapiro J, Wood LD, Lin M, Duran R, Cornish T, Lesage D, Charu V, Schernthaner R, Wang Z, Tacher V, Savic LJ, Kamel IR, Geschwind JF (2014) Radiologic-pathologic analysis of contrast-enhanced and diffusion-weighted MR imaging in patients with HCC after TACE: diagnostic accuracy of 3D quantitative image analysis. Radiology 273(3):746–758. https://doi.org/10.1148/radiol.14140033
Budjan J, Sauter EA, Morelli JN, aI. (2016) Semi-automatic volumetric measurement of treatment response in hepatocellular carcinoma after trans-arterial chemoembolization. Anticancer Res 36(8):4353–4358
Funding
Not applicable (no funding)
Author information
Authors and Affiliations
Contributions
MFO put the study design idea of the study and performed the volumetric CT assessment. ASA participated in the study design, data collection and statistical analysis. HAS put the idea of the study and participated in the manuscript editing and supervision of the volumetric CT assessment. TME did data collection and clinical assessment of the patients. SFE was Editor of the manuscript and participated in the statistical analysis and volumetric CT assessment. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was signed by all patients before the TACE procedure and before the contrast-enhanced CT study. The study was approved by the medical committee of the Faculty of Medicine, Cairo University. Reference number is not available.
Consent for publication
The study is retrospective with data collection from the PACS of our institution. The consent for publication is not available.
Competing interests
The authors declare that they have no financial or non-financial competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osman, M.F., Farag, A.S.A., Samy, H.A. et al. Role of multislice computed tomography 3D volumetric analysis in the assessment of the therapeutic response of hepatocellular carcinoma after transarterial chemoembolization. Egypt J Radiol Nucl Med 52, 177 (2021). https://doi.org/10.1186/s43055-021-00542-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00542-w