Abstract
Background
The ongoing global pandemic of coronavirus disease 2019 (COVID-19) may cause, in addition to lung disease, a wide spectrum of non-respiratory complications. Among these are thromboembolic complications. The theories that explain the mechanism of thromboembolic complications of COVID-19 are accumulating rapidly, and in addition to the role of imaging for assessment of COVID-19 pneumonia, CT may be useful for identification of these complications, such as pulmonary embolism, ischaemic stroke, mesenteric ischaemia, and acro-ischaemia.
Results
Thromboembolic manifestations were diagnosed in 10% of our patients (124 patients out of the total 1245 COVID-19 patients); 56 patients (45.2%) presented with pulmonary embolism, 32 patients (25.8%) presented with cerebrovascular manifestations, 17 patients (13.7%) presented with limb affection, and 19 patients (15.3%) presented with gastrointestinal thromboembolic complications.
Most of our patients had significant comorbidities; diabetes was found in 72 patients (58%), dyslipidemia in 72 patients (58%), smoking in 71 patients (57.3%), hypertension in 63 patients (50.8%), and morbid obesity in 40 patients (32.2%).
Thromboembolic events were diagnosed on admission in 41 patients (33.1%), during the first week in 61 patients (49.2%), and after the first week in 22 patients (17.7%).
Conclusions
The incidence of thromboembolic complications in COVID-19 patients is relatively high resulting in a multisystem thrombotic disease. In addition to the crucial role of imaging for assessment of COVID-19 pneumonia, CT is important for assessment of the thromboembolic complications, such as pulmonary embolism, ischaemic stroke, mesenteric ischaemia, and peripheral ischaemia, especially in patients with elevated d-dimer levels and those with sudden clinical deterioration.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The ongoing global pandemic of coronavirus disease 2019 (COVID-19) may cause, in addition to lung disease, a wide range of non-respiratory complications due to involvement of organs by the virus or due to direct or indirect complications of this infection [1, 2]. Among these, thromboembolic complications due to abnormal coagulation were presented as an important issue in patients with COVID-19 infection and may occur in up to 31% of COVID-19 patients in intensive care unit (ICU) [3, 4].
Other organ systems are affected due to the marked affinity of the virus for the angiotensin-converting enzyme 2 (ACE2) receptors [5, 6]. Thus, tissues with high levels of ACE2 receptor are susceptible to direct infection [7]. These are most abundant in lung alveolar epithelial cells, enterocytes of the small intestine, and vascular endothelium [5].
Unlike hemorrhagic viruses (Ebola, Marburg...), Covid-19 is highly prothrombotic causing alterations in the coagulation cascade that leads to a progressive elevation of d-dimer correlated with the severity and extent of microthrombosis [8].
There is increasing evidence that thrombi are a major cause of multisystem organ dysfunction, including respiratory failure [9]. A number of studies showed that coagulation disorders related to COVID-19 are correlated with increased morbidity and mortality [10, 11].
COVID-19-associated thrombotic disease is suggested to be caused by various mechanisms including direct effects of COVID-19 through severe illness and hypoxia or severe inflammatory response or an indirect effect of infection related to investigational therapies used for treating COVID-19, which may have adverse drug interactions with antiplatelet agents and anticoagulants [12].
The theories that explain the mechanism of thromboembolic complications of COVID-19 are accumulating rapidly, and in addition to the role of CT chest for assessment of COVID-19 pneumonia, other imaging modalities may be useful for identification of these complications, such as pulmonary embolism, ischaemic stroke, mesenteric ischaemia, and acro-ischaemia.
Aim of this study
The aim of this study was to estimate the prevalence of thromboembolic manifestations among COVID-19-positive patients and to describe the imaging findings of Covid-19-positive patients who presented with acute arterial or venous thromboembolic events in the pulmonary, cerebral, abdominal, or peripheral circulation.
Methods
Ethics approval and consent to participate
The study protocol was approved by the local Ethics Committee. All study procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The ethics committee’s reference number is 9/2020RAD4.
All patients included in this study were informed that their clinical, laboratory, and radiological data will be used in the study. A written consent was taken from all patients.
Study population
Between April and July 2020, we scanned 1245 COVID-19-positive patients, 124 of them (about 10%) had developed thromboembolic manifestations, pulmonary, abdominal, cerebral, or peripheral limbs.
The study included 73 males (58.9%) and 51 females (41.1%) with age ranged from 23 to 65 years old, (mean age 43.52 years ± 12.21 years).
Inclusion criteria included patients with confirmed Covid-19 infection who presented initially with thromboembolic symptoms or admitted to the hospital and then developed thromboembolic manifestations.
Exclusion criteria included patients with thromboembolic manifestations not confirmed to be COVID-19 positive and patients with chronic thromboembolic events.
Imaging techniques
Patients underwent imaging for the suspected region according to the primary manifestations. Patients with suspected stroke underwent MRI brain with DWI according to the routine stroke protocol. Positive patients with acute stroke underwent MR cerebral angiography and venography.
The CT pulmonary and abdominal angiogram was performed after intravenous injection of 80–120 cc of iodinated contrast media at a flow rate of 3–5 ml/s followed by a 30 ml saline at the same rate. Region of interest was determined, and axial scans were taken during the contrast injection until a threshold enhancement and triggering a diagnostic scan. Indirect venography was done for the patients.
Patients with suspected peripheral arterial or venous acute arterial and/or venous thrombosis underwent duplex/Doppler examination of the affected limb followed by CT peripheral angiography for positive cases.
All CT scans were performed on a 128-slice multidetector CT scanner.
Image analysis
The images were assessed for presence of vascular occlusion either arterial or venous.
Pulmonary CT angiography images were evaluated for location and extent of the thrombus, associated pulmonary manifestations of COVID-19, and presence of areas suggestive of lung infarction.
Abdominal CT angiography images were evaluated for evidence of arterial and/or venous thrombus (location and extent); involvement of IVC and portal, mesenteric, and iliac veins; and associated manifestations of bowel ischaemia (pneumatosis intestinale or portal vein gas) or intestinal obstruction. Evidence of solid organs infarction was evaluated.
Cerebral venogram and angiogram images were evaluated for location and extent of venous sinus thrombosis and evidence of acute arterial thrombosis and its location. Associated cerebral infarctions were evaluated for their extent and presence of hemorrhagic infarction. Evidence of diffusion restriction even with no definite vascular occlusion at angiography was considered thromboembolic events.
Duplex studies and peripheral angiography of the upper and lower limbs were evaluated for presence and extent of acute venous thrombosis and presence and extent of acute arterial occlusion.
Data collection
Demographic and clinical data (presenting symptoms, risk factors, d-dimer values, and ICU admission) were collected from medical records. All data were compiled and analyzed.
Results
This study is observational cross-sectional study included 1245 COVID-19-positive patients, 124 of them (10%) developed thromboembolic manifestations (Fig. 1). Fifty-six patients (45.2%) had pulmonary embolism, 32 patients (25.8%) had cerebrovascular manifestations, 17 patients (13.7%) had peripheral vascular affection, and 19 patients (15.3%) had gastrointestinal thromboembolic complications (Fig. 2).
Patients with thromboembolic manifestations were 77 males (62.1%) and 47 females (37.9%) with age ranged from 23 to 65 years old (mean age 43.52 years ± 12.21 years). One or more comorbidities were found; diabetes was found in 72 patients (58%), dyslipidemia in 72 patients (58.1%), smoking in 71 patients (57.3%), hypertension in 63 patients (50.8%), and morbid obesity in 40 patients (32.3%).
The d-dimer level was very high notably in patients with pulmonary embolism (Table 1). Thromboembolic events were diagnosed on admission in 41 patients (33.1%), during the first week of admission in 61 patients (49.2%), and after the first week of admission in 22 patients (17.7%).
Pulmonary embolism presented on admission in 34 patients (60.7%), 13 patients (23.2%) developed symptoms within the first week of admission, and 9 patients (16.1%) had pulmonary embolism after 1 week. The most presenting symptom was shortness of breath (52 patients 92.9%). Fourteen patients were presented with radiological findings that favor the evidence of lung infarction more than the classic features of COVID-19 pneumonia.
Three patients (9.4%) were presented with acute stroke. Twenty-four patients (75%) developed cerebrovascular symptoms within the first week of hospital admission for respiratory manifestations. Five patients (15.6) developed cerebrovascular symptoms after 1 week of admission (2 patients presented with sensory manifestations and found to have small thalamic infarction and 3 patients developed motor deficit). Twenty-five patients (78.1%) with cerebrovascular manifestations had associated pneumonia.
Ischaemic stroke has been associated with arterial thrombosis in 18 patients (40.6%) and venous sinus thrombosis in 9 patients (25%). Seven of them presented with hemorrhagic infarctions. Middle cerebral artery thrombosis was detected in 8 patients, internal carotid artery in 3 patients, anterior cerebral artery in 3 patients, basilar artery in 2 patients, and vertebral artery in 2 patients. Five patients (12.5%) presented with small infarcts identified only on MRI with no definite vascular involvement. Superior sagittal sinus thrombosis was identified in 5 patients, sigmoid sinus thrombosis in 2 patients, one patient presented with isolated straight sinus thrombosis, and one patient presented with internal jugular vein thrombosis.
Seventeen patients had peripheral thromboembolic manifestations; 9 patients (52.9%) had deep venous thrombosis of the lower limb, 2 patients (11.8%) had deep venous thrombosis of the upper limb, 5 patients (29.4%) had lower limb ischaemia, and one patient (5.9%) had upper limb ischaemia. All patients with deep venous thrombosis presented with edema of the affected limb (Table 2). Eleven patients (91.7%) of peripheral thromboembolic manifestations presented within the first week of admission.
Nineteen patients had abdominal thromboembolic manifestation; 17 venous thrombosis (89.5%) and 2 arterial embolism (10.5%). The most presenting symptom was abdominal pain (18 patients 94.7%). Isolated superior mesenteric vein thrombosis was detected in 4 patients (21%), isolated portal vein thrombosis occurred in 3 patients (15.8%), isolated inferior vein thrombosis was detected in 1 patients (5.3%), and combination of more than one vein thrombosis was detected in 9 patients (47.4%). Arterial thrombosis was detected in the superior mesenteric artery in 2 patients (10.5%), and both presented with bowel ischaemia and intestinal obstruction (Table 2).
Discussion
The coagulopathy that goes with COVID-19 has gained increasing interest recently. The International Society of Thrombosis and Haemostasis reported that patients with severe coronavirus disease 2019 (COVID-19) have fulminant activation of coagulation and consumption of coagulation factors [13].
In our study, we found 124 patients (about 10%) with thromboembolic manifestations out of 1245 Covid-19-positive patients, 68.5% of them were admitted to the ICU. The rate of thromboembolism reported in the literature is variable. Some studies have reported thromboembolic rates in the range of 20–30% while others have reported rates as high as 40–70% [14]. The number of patients with thromboembolic manifestations in our study was less than that of Klok et al. [3] who observed thrombotic complications in 31% of ICU patients in a multicenter cohort of 180 patients admitted to the ICU of three Dutch hospitals, and that difference was due to the specific group of patients that they studied as all patients were in the ICU.
The presence of hypercoagulation and thromboembolic complications had been noted to correlate with disease severity and ICU admission [14]. In our study, 85 patients (68.5%) were admitted to the ICU.
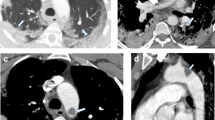
In the current study, pulmonary embolism was the most common complication presented in 56 patients (45.2%) that was similar to Grillet et al. [15] who stated that pulmonary embolism is the most common thromboembolic complication of COVID-19; it has been presented radiologically in up to 30% of patients with COVID-19 on pulmonary CT angiography and in 14% of ICU patients diagnosed with COVID-19 pneumonia Figs. 3, 4 and 5.
In a meta-analysis conducted by Xiong et al. [16], they found that prothrombin time and d-dimer levels were significantly higher in patients with severe COVID-19 than in those with the mild disease. Lorant et al. [17] stated that COVID-19 patients with pulmonary embolism have higher d-dimer levels than those without pulmonary emboli and are more likely to be admitted to the ICU. They also reported that d-dimer > 2660 ng/mL has 100% sensitivity and 67% specificity for pulmonary embolism diagnosis prediction in COVID-19 patients, and that was the same in our study which found that highest d-dimer average value was found in patients with pulmonary embolism (average 2765.45 ± 169.11).
As a complication of pulmonary embolism, the lung infarction is rare due to the dual arterial supply of the lung, but it has been described in COVID-19 patients. On CT, lung infarction appears as ground-glass opacities in the early phases in unobstructed lung zones that represents pulmonary haemorrhage and peripheral wedge-shaped pulmonary consolidation [18, 19].
Therefore, the radiological findings of lung infarction from pulmonary embolism should be differentiated from GGO as well as consolidations of the COVID-19 pneumonia that may also show reverse a halo sign in about 4% of patients as this will positively impact the patient management. In non-enhanced CT, the presence of peripheral lung opacities with a reverse halo sign, dilatation of pulmonary trunk, and/or increased cardiac volume (particularly, enlargement of the right cardiac chamber) indicate risk of PE and may aid in the decision to perform CT pulmonary angiography to confirm or exclude pulmonary embolism [20]. Clinical parameters including highly elevated d-dimer levels, haemoptysis, and/or sudden worsening of respiratory function or chest pain should also be considered [21].
We have identified 14 patients with radiological findings that favor the evidence of lung infarction more than the classic GGO and consolidations of COVID-19. These patients had higher d-dimer levels with dilatation of the affected segment of the pulmonary artery. The peripheral wedge-shaped consolidation was associated with thrombus of the related subsegmental artery (Figs. 6 and 7).
In the current study, we reported 32 patients with acute cerebrovascular manifestations, 27 (65.6%) of them had evidence of vascular occlusion (arterial in 18 patients Fig. 8 and venous sinus thrombosis in 9 patients Fig. 9) and 7 (21.88%) had haemorrhagic stroke. These results are close to those of Li et al. [22] who reported cerebrovascular manifestations for (6%) of 221 COVID-19 patients in a retrospective case series from Wuhan: 5% patients developed ischaemic strokes, < 1% intracerebral haemorrhage, and < 1% cerebral venous sinus thrombosis. However, the number of patients in our results was much less than the patients of Benussi et al. [23] who reported that (77%) of 55 COVID-19 patients admitted to one neurology unit with cerebrovascular disease, 35 of them had ischaemic stroke, three patients had haemorrhagic stroke, and five had transient ischaemic attacks. This difference is likely due to specific patient’s group that they studied as it was specialized neurology unit.
In our study, five patients (12.5%) presented with small infarcts identified only on MRI with no definite vascular involvement. Figures 10 and 11 Kandemirli et al. [24] reported that 44% of ICU COVID-19 patients with neurological symptoms showed abnormal findings on brain MRI studies.
In a study done by Wichmannet et al. [25] on autopsy series, they found unsuspected deep vein thrombosis in the majority of COVID-19 patients, and that pulmonary embolism was the cause of death; also, Goldman et al. [26] stated that there is high incidence of arterial thrombosis in COVID-19 patients presenting with ischaemic leg symptoms (100% of cases in their cohort). They found that lower extremity arterial thrombosis associated with COVID-19 is characterized by greater thrombus burden and increased rate of amputation and death. In our study, 17 patients had peripheral thromboembolic manifestations, 9 patients (52.9%) had deep venous thrombosis of the lower limb, 2 patients (11.8%) had deep venous thrombosis of the upper limb, 5 patients (29.4%) had lower limb ischaemia Fig. 12, and one patient (5.9%) had upper limb ischaemia.
Bhayana et al. [27], in their study, described radiological abnormalities detected on abdominal CT in about 42% of COVID-19 patients as large or small bowel thickening, pneumatosis intestinale, portal vein gas, or bowel perforation, and also bowel ischaemia or necrosis was demonstrated in some of these patients who underwent surgery. In addition, acute infarction in abdominal solid organs was demonstrated in 4.8% of patients.
In the current study, we reported 19 cases with gastrointestinal thromboembolic complications, 17 venous thrombosis (89.5%) and 2 arterial embolism (10.5%). The most presenting symptom was abdominal pain in 18 patients (94.7%). Isolated superior mesenteric vein thrombosis was detected in 4 patients (21%), isolated portal vein thrombosis occurred in 3 patients (15.8%), isolated inferior vein thrombosis was detected in 1 patients (5.3%), and combination of more than one vein thrombosis was detected in 9 patients (47.4%) Fig. 13. Arterial thrombosis was detected in the superior mesenteric artery in 2 patients (10.5%) and both of them presented with bowel ischaemia and intestinal obstruction.
Conclusion
The incidence of thromboembolic complications in COVID-19 patients is relatively high, and the appropriate mechanism of these complications is the pro-coagulant pattern and the endothelial thrombo-inflammatory syndrome, which may result in multisystemic thrombotic disease.
In our study, the d-dimer level was more than 2600 ng/mL in 83 patients including all 56 patients with pulmonary emboli. So, in patients with high d-dimer levels on hospital admission or sudden clinical worsening, CT pulmonary angiography should be done to exclude pulmonary embolism
Also risk factors (diabetes, obesity, heavy smoking), clinical parameters, including haemoptysis, sudden worsening of respiratory function, acute abdomen and peripheral limb edema, or chest pain should raise the suspicions of thromboembolic complications.
So, in addition to the crucial golden role of CT chest for assessment of COVID-19 pneumonia, other imaging modalities (Duplex study, CT angiography, and MRI brain) are also important for the assessment of the thromboembolic complications, such as pulmonary emboli, cerebrovascular strokes, mesenteric vascular ischaemia, and peripheral ischaemia, especially in patients with high d-dimer levels and those with sudden clinical deterioration.
Availability of data and materials
All data and materials are available.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- ACE2:
-
Angiotensin-converting enzyme 2
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- MRI:
-
Magnetic resonance imaging
- DWI:
-
Diffusion weighted imaging
References
Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020, https://doi.org/https://doi.org/10.1111/jth.14817.
Wang T, Chen R, Liu C, et al. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol 2020, https://doi.org/https://doi.org/10.1016/S2352-3026(20)30109-5. S2352- 3026(20)30109-5.
Klok FA, Kruip MJHA, Van M et al (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res S0049-3848(20):30120–30121
Cui S, Chen S, Li X, et al. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 2020, https://doi.org/https://doi.org/10.1111/jth.14830.
Hamming I, Timens W, Bulthuis M et al (2004) Tissue distribution ofACE2 protein, the functional receptor for SARS coronavirus: a first step in understanding SARS pathogenesis. J Pathol 203:631–637 Cross Ref Medline
Li WH, Moore MJ, Vasilieva NY et al (2003) Angiotensin-convertingenzyme 2 is a functional receptor for the SARS coronavirus. Nature 426:450–454 Cross Ref Medline
Zou X, Chen K, Zou J, Han P, et al. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020;http://dx.doi.org/https://doi.org/10.1007/s11684-020-0754-0.
Chen J, Wang X, Zhang S, et al. Findings of acute pulmonaryembolism in COVID-19 patients. 2020. Available at SSRN: https://ssrn.com/abstract=3548771 or https://doi.org/102139/ssrn3548771 Google Scholar.
Algahtani H, Subahi A, Shirah B (2016) Neurological complications of Middle East respiratory syndrome coronavirus: a report of two cases and review of the literature. Case Rep Neurol Med 2016:3502683
Chen N, Zhou M, Dong X et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507–513
Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med 2020; Epub ahead of print. https://doi.org/https://doi.org/10.1515/cclm-2020-0188
Bikdeli B, Madhavan MV, Jimenez D et al (2020) COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol S0735-1097(20):35008–35007
Kaur P, Qaqa F, Ramahi A , et al. Acute upper limb ischemia in a patient with COVID-19. Hematol Oncol Stem Cell Ther 2020. https://doi.org/https://doi.org/10.1016/j.hemonc.2020.05.001, Submitted for publication.
Malas M, Naazie I, Elsayed N et al (2020) Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. E Clin Med 29-30:1–9
Grillet F, Behr J, Calame P et al (2020) Acute pulmonary embolism associated with COVID-19 pneumonia detected by pulmonary CT angiography. Radiology:201544. https://doi.org/10.1148/radiol.2020201544
Xiong M, Liang X, Wei Y. Changes in blood coagulation in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Br J Haematol 2020. https://doi.org/https://doi.org/10.1111/bjh.16725, Submitted for publication.
Lorant LI, Delabranche X, Severac F et al (2020) Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship to D-dimer levels. Radiology:201561. https://doi.org/10.1148/radiol.2020201561
Lax SF, Skok K, Zechner P, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med (14 May 2020), https://doi.org/10.7326/M20-2566
Cha SI, Shin KM, Lee J et al (2012) Clinical relevance of pulmonary infarction in patients with pulmonary embolism. Thromb Res 130(3):e1–e5. https://doi.org/10.1016/j.thromres.2012.03.012
Torres P, Mancano A, Zanetti G et al (2020 Apr) Multimodal indirect imaging signs of pulmonary embolism. Br J Radiol 93(1108):20190635. https://doi.org/10.1259/bjr.20190635
Moreira B, Santana P, Zanetti G, Marchiori E (2020) COVID-19 and acute pulmonary embolism: what should be considered to indicate a computed tomography pulmonary angiography scan? Rev Soc Bras Med Trop 53:e20200267. https://doi.org/10.1590/0037-8682-0267-2020
Li Y, Wang M, Zhou Y, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. 2020. https://media.tghn.org/medialibrary/2020/06/Li_2020_Preprint_
Benussi A, Pilotto A, Premi E, et al. Clinical characteristics and outcomes of inpatients with neurologic disease and COVID-19 in Brescia, Lombardy, Italy. Neurology 2020; published online May 22. https://doi.org/10.1212/WNL.0000000000009848.
Kandemirli SG, Dogan L, Sarikaya ZT et al (2020) Brain MRI findings in patients in the intensive care unit with COVID-19 infection. Radiology 297:E232–E235.
Wichmann D, Sperhake JP, Lütgehetmann M et al (2020) Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study (published online ahead of print, 2020). Ann Intern Med. https://doi.org/10.7326/M20-2003
Goldman I, Kenny Y & Scheinfeld M. Radiology Published Online: Jul 16 2020 https://doi.org/https://doi.org/10.1148/radiol.2020202348
Bhayana R, Som A, Li M et al (2020) Abdominal imaging findings in COVID-19. Preliminary observations. Radiology:201908. https://doi.org/10.1148/radiol.2020201908
Acknowledgements
We would like to thank all people who helped us in this work including the CT and MRI technicians.
Funding
Self-funding.
Author information
Authors and Affiliations
Contributions
SO made substantial contribution to the main research idea; design of the work; acquisition, analysis, and interpretation of the data; writing of the manuscript, and revision of the work. RH contributed in the analysis of the data, interpretation of the results, summarization of the discussion, and final revision of the manuscript. AM made substantial contribution to the main research idea; design of the work; acquisition, analysis, and interpretation of the data; and drafting and revision of the work. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local Ethics Committee. All study procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The ethics committee’s reference number is 9/2020RAD4.
Consent for publication
A written consent was taken from all patients prior to the study for publication.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Omar, S.F., Habib, R.M. & Motawea, A.M. Radiological findings of COVID-19-related thromboembolic complications. Egypt J Radiol Nucl Med 52, 99 (2021). https://doi.org/10.1186/s43055-021-00446-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00446-9