Abstract
Background
To evaluate the role of PET/CT on bronchogenic carcinoma staging as well as treatment response evaluation on follow-up compared to CT study alone.
Methods
A prospective study of 60 patients confirmed histopathologically to have non-small cell bronchogenic carcinoma, 30 of them came for staging (group T) while the rest 30 came for follow-up (group F) to assess therapy response. All patients underwent PET/CT with data analysis done using the eighth edition tumor, nodal, metastatic staging (TNM) staging for group T and RECIST/PERCIST criteria for group F. The CT data alone transferred to a blind radiologist for analysis using the same parameters. The results were collected and compared.
Results
Regarding group T, 12 patients showed different TNM staging between PET/CT and CT alone, 5 cases with different T stagings, 4 cases with different N stagings, and 5 cases with different M stagings. Also, 8 cases showed different surgical stagings. Regarding group F, 9 cases showed a difference between RECIST obtained by CT and PERCIST obtained by PET/CT with most of the cases (6 cases) showed change from partial or stable response to progressive response.
Conclusion
PET/CT has a significant role in TNM staging of bronchogenic carcinoma more at T2 staging due to its ability to differentiate the tumoral mass from the nearby pulmonary reaction. Also, PET/CT makes a difference in tumoral follow-up by its ability to detect the functional changes even before structural changes. Finally, PET/CT is a very important tool in management strategy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Bronchogenic carcinoma is one of the most common causes of cancer-related mortalities with the rate of incidence reaching about 1.5 million cases per year worldwide [1].
Bronchogenic carcinoma classified histopathologically into either non-small cell (NSCLC) or small cell type with non-small cell is the commonest representing up to 87% of cases [2].
Currently, the eighth edition of tumor, nodal, metastatic staging (TNM) staging is the most recent and updated edition for bronchogenic carcinoma staging replacing the known seventh edition since January 2017. TNM staging is a universal staging system for tumor (T), lymph nodes (N), and metastases (M) [3].
Bronchogenic carcinoma staging is crucial for treatment strategy, planning, and prognosis prediction with radiological imaging play a cornerstone role in staging [4, 5]. Patients with stage I are suitable for lobectomy or pneumonectomy while stage II patients are treated surgically followed by adjuvant chemotherapy. Patients with stage IIIA receive chemotherapy and radiotherapy followed by surgery if downstaging occurred while for patients with stage IIIB or IV, the surgery has no role in their treatment [6].
CT is the most commonly used radiological modality for tumoral staging due to its availability and rapid scanning with high-resolution images, but it has some limitations in identifying the actual tumoral boundaries separating it from the nearby adjacent non-malignant pulmonary changes such as collapse, atelectasis, or consolidation. Also, the assessment of pleural, pericardial, and mediastinal invasions is difficult to be accurately assessed by CT [7].
Radiological follow-up of bronchogenic carcinoma to assess therapy response using CT established by using Response Evaluation Criteria In Solid Tumor (RECIST criteria) depending on size change and reduction of the tumoral mass. However, structural changes may occur late after positive biological response, giving a false impression of stationary course. Also, central necrosis or hemorrhage secondary to treatment may cause an increase in the tumor mass size, giving a pseudo-progression result in CT [8, 9].
PET/CT is a radiological modality that can assess the tumoral malignant activity depending on fluorodeoxyglucose (FDG) uptake by the malignant tissue. Hence, it can accurately delineate the tumoral mass separating it from the surrounding non-malignant reaction and detect early biological changes in response to therapy even before the structural changes. Also, PET/CT can detect the activity of pulmonary nodules detected during the interpretation of the CT chest differentiating the benign from malignant one as well as the metastatic changes [8]. The follow-up of bronchogenic carcinoma using PET/CT is done using PET/CT Response Criteria In Solid Tumor (PERCIST criteria) depending on standardized uptake value (SUV uptake) changes by the tumoral mass [10].
PET/CT offers both structural and functional information about the tumoral mass and malignant activity overall the body and hence can accurately assess the tumor staging and tumor response to therapy [11].
Our study aimed to assess the role of PET/CT in NSCLC staging and follow-up assessment and to what extent PET/CT can change the tumoral TNM staging and the therapy response degree using PERCIST when compared to CT RECIST. Also, we studied the effects of these changes on the treatment decision and management plane.
Methods
Patients
This was a prospective study conducted on 60 patients who came to the Radiology Department with pathologically proven NSCLC. The patients came to do PET/CT as requested by the chest/radiotherapy team either for staging (group T) or follow-up (group F). 30 patients were included in each group. The study was conducted over the period from April 2017 to January 2019. Informed written consent was taken from all patients according to the ethical committee regulations. All patients were subjected to PET imaging followed by post-contrast CT in the same session.
Inclusion criteria
All patients with pathologically proven NSCLC with no age or sex predilection.
Exclusion criteria
We excluded any pregnant female for the risk of radiation exposure, patients with high kidney function as a contraindication for CT contrast injection, and patients with high blood glucose levels at the time of the study to avoid FDG misinterpretation. Any patients with a history of allergy were also excluded for fear of complications of contrast allergy.
Patient preparation
Serum creatinine was requested before the study and confirmed to be within normal limits for CT contrast injection. Also, the diabetic patients were asked to adequately control their blood glucose level at the period before the date of imaging. Fasting for 6 h before the scan was requested. IV cannula was inserted and better to be inside the antecubital vein at the opposite side to the tumor side. The patients were kept in a controlled warm temperature room to decrease the FDG uptake by the brown fat.
Technique
-
PET/CT machine: Discovery IQ five-ring machine class I IPX0 used with 16 slices of CT, GE (General Electric Company), Milwaukee, Wisconsin, USA, 2016.
-
Contrast dose: 10–20 mCi were injected 60-90 min before the exam and the patients were asked to rest in a quiet place without vigorous activity and trying to avoid even talking as minimal as they can.
-
Technique: All patients were placed on a supine position with elevated arms for imaging acquisition starting from the skull base down to the upper thigh level. We started with PET imaging followed by post-contrast CT using the same scan area.
-
Post-imaging instruction: The patients were asked to drink many amounts of water, avoid contact with children for 24 h, and stop lactation for 24 h.
Image interpretation
All images including PET and CT images were transferred to a specific workstation where PET/CT-fused images could be done. Multi-planar reformatted images (MPR) were also done for both PET and CT images. PET/CT images were interpreted via a specialized radiologist in PET/CT fields with at least 5 years’ experience. The CT images alone were transferred to another workstation to be interpreted by another blind radiologist with at least 5 years of CT imaging experience. The following parameters were used for imaging interpretation:
Regarding group (T), we used the eighth TNM staging system [3].
Regarding group (F), we used PERCIST 1.0 criteria on PET/CT interpretation and RECIST 1.1 criteria on CT interpretation. The tumor size, SUV uptake, and other findings were recorded (Table 1) [12, 13].
Analysis of data
the analysis of data was done using IBM SPSS statistics (V. 24.0, IBM Corp., USA, 2016). Continuous parametric data were presented as mean ± SD and non-parametric data as median (IQR) and categorical data was presented as a number and percentage of patients.
Results
Sixty patients with a histopathological diagnosis of NSCLC were included in our study with the age of the patients ranging from 39 to 72 years old and the mean age was 49 ± 12.5 SD years. 63.3% of the patients were male with 71.7% of all patients showing a positive history of smoking, which is considered one of the most important risk factors for bronchogenic carcinoma.
The TNM staging results in group T patients by CT and PET/CT as well as the surgical staging results are demonstrated in Figs. 1 and 2. Different therapeutic response results obtained in group F patients by CT and PET/CT are demonstrated in Fig. 3.
Regarding TNM staging of group T included 30 patients, 12 patients representing 40% of cases showed different TNM staging results between the PET/CT staging and CT alone staging, and five of them showed different T staging (Figs. 4, 5, and 9) with four of them representing 80% showed downgrade staging (Figs. 4 and 9). Four cases showed different N stagings (Fig. 4) with 100% of them showing upgrade staging. Five cases showed different M stagings (Figs. 5, 6, 7, and 8) with three of them representing 60% showed downgrade staging (Figs. 6 and 8).
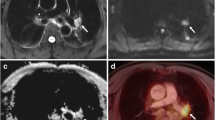
A female patient 72 years old presented with hemoptysis and proven histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the right lower lobe measuring 34.5 × 27.3 mm staged as T2 (a) with sub-centimetric right para-tracheal lymphadenopathy considered to be nonspecific and staged as N0 (c). Her PET/CT revealed right lobe mass lesion measuring 25.6 × 17 mm in average staged as T1 with a downgrade of the CT-T staging separating the actual tumoral tissue from the surrounding pulmonary non-malignant changes with positive activity detected at the right para-tracheal lymphadenopathy staged as N1 instead of N0 diagnosed by CT (b, d). The surgical staging of the patients by PET/CT changed from IA to IIB
A male patient 67 years old presented with dyspnea and attacks of hemoptysis and proven histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the right lower lobe = 3 cm considered as T1 with a small 5 mm pulmonary nodule involving the right middle lobe at the para-cardiac region (a, b) and considered by CT to be non-specific nodule. A bone study by CT was negative. PET/CT study reveals positive FDG uptake detected inside the pulmonary nodule (white circle c) (T4), as well as positive active spots, noted affecting the thoracic bone namely the ribs, sternal body and the transverse process of the dorsal spine (M1c) (black circle) (e, f). The surgical staging of the patients by PET/CT changed from IIB to IVB
A female patient 57 years old presented with attacks of hemoptysis and proven histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the left upper lobe with a small 5 mm pulmonary nodule involving the right middle lobe and considered a metastatic nodule (M1a) (white arrow, a). The nodule showed insignificant FDG uptake as seen in b and c PET/CT images. The surgical staging of the patients by PET/CT changed from IVA to IIA
a–h A male patient 68 years old presented with dyspnea and repeated chest infection with attacks of hemoptysis and proved histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the right lower lobe with multiple malignant mediastinal and hilar lymphadenopathies. Bone examination via CT was negative yet with PET/CT multiple scattered FDG uptake marrow lesions detected involving the spinous process of L1 and right aspect of the sacrum considered metastatic bony lesions (M1c). The surgical staging of the patients by PET/CT changed from IIIB to IVA
a–c A female patient 55 years old presented with dyspnea and attacks of hemoptysis and proven histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the apical segment of the right lower lobe with multiple malignant mediastinal lymphadenopathies as well as contra-lateral 7 mm pulmonary nodules involving the left lower lobe (a). The case staged as T2 N1 M1. PET/CT showed no evidence of significant activity involving the pulmonary nodules and considered nonspecific nodule changing the staging to T2 N1 M0. The surgical staging of the patients by PET/CT changed from IVA to IIB
Among the patients with different T stagings, we found two cases out of five (40%) within T2 staging by CT. While in cases with different N stagings, we found two cases out of four between cases with N1 staging by CT (Fig. 4). In patients with different M stagings, three cases showed a change in M staging due to the PET/CT ability to identify the activity of the contralateral pulmonary nodules (Figs. 6 and 8).
Regarding group T surgical staging, eight cases among the 12 cases with different TNM stagings showed a change in surgical staging (four of them showed upgrade surgical staging (Figs. 4, 5, and 7) while the other four showed downgrade surgical staging (Figs. 6 and 8)). The remaining four cases showed no change in surgical staging, although there was a change in TNM staging (Fig. 9). The change of the surgical staging leads to the change in management strategies which occurred in eight patients of group T representing 26.7% of cases (Fig. 10).
a–c A male patient 69 years old presented with attacks of hemoptysis and proved histopathologically to have NSCLC. CT study reveals a malignant mass lesion involving the left upper lobe = 34.3 × 26.8 mm with subsequent distal pulmonary consolidation with malignant looking ipsilateral mediastinal lymphadenopathies with no definite metastases by CT and the case staged as T2 N1 M0. PET/CT reveals the same results yet with the more adequate delineation between the mass and the related distal consolidation with the actual mass size became 26 × 19 mm on average with subsequent T staging downgrading from T2 to T1. No change occurred for the surgical staging kept with IIB
Regarding group F which included 30 patients, nine cases (30%) showed a change in therapeutic response assessment using RECIST/PERCIST criteria, six of them representing 66.67% showed a change from partial or stable response by RECIST criteria to progressive response using PERCIST criteria (Figs. 11, 12 and 13). Two showed change from stable response by RECIST criteria to partial response by PERCIST (Fig. 11). The last one showed change from the progressive response by RECIST to the stable response by PERCIST criteria. The management strategy changed with seven cases of group F representing 23.3% of cases.
A male patient 40 years old diagnosed to have NSCLC received radiotherapy and chemotherapy. Baseline study (A, B, and C) showed the mass lesion = 82 × 38 mm on average with SUV uptake = 9.9. On follow-up after 3 months (Af, Bf, and Cf) showed almost stationary course regarding the size of the mass by CT = 81 × 37 mm in average interpreted as stable disease by RECIST criteria while on PET/CT the SUV decreased to be 4.4 instead of 9.9 leading to change in the opinion to be partial response by PERCIST criteria
A male patient 45 years old diagnosed to have NSCLC received chemotherapy. Baseline study (A and B) showed the mass lesion = 35.3 × 34.4 mm on average with SUV uptake = 2.9. On follow-up after 3 months (Af and Bf) showed decrease in the size of the mass by CT = 29.6 × 29.5 mm in average interpreted as stable disease by RECIST criteria (the decrease in size not met the criteria of partial response by RECIST criteria) while in PET/CT, the SUV increased to be 6.04 instead of 2.9 leading to change in opinion to be progressive disease response by PERCIST criteria instead of stable disease by RECIST criteria
A female patient 70 years old diagnosed to have NSCLC received chemotherapy and radiotherapy. Baseline study (A and B) showed the mass lesion = 90 × 62 mm in average with SUV uptake = 9.5. On follow-up after 3 months (Af and Bf) showed almost no change in the size of the mass by CT = 92 × 63 mm in average interpreted as stable disease by RECIST criteria while in PET/CT, the SUV increased to be 14.8 instead of 2.9 leading to change in opinion to be progressive disease response by PERCIST criteria instead of stable disease by RECIST criteria
Finally, PET/CT results changed the treatment strategies between 14 patients in all study population representing 23.3% of all our patients including both groups.
Discussion
This study demonstrates the significance of PET/CT uses during the evaluation of cases with non-small cell bronchogenic carcinoma, either during staging or during follow-up to assess the therapeutic response. PET/CT showed a change in the TNM staging in 40% of the studied cases and a change in follow-up response in 30% of the studied cases. Eight cases in group T representing 26.7% and seven cases in group F representing 23.3% showed a change in the management strategy, according to the change in their surgical staging and the change in their treatment response evaluation, respectively.
This is explained by the difference between the two modalities as the CT gives us information about the morphology of the tumor and the morphology of the associated metastatic lesions as well as anatomical details while the PET/CT has the ability to combine both the morphological and the functional activity with the advantage of detection of the functional changes of both the tumoral mass and the associated metastatic lesions.
A lot of researchers studied the impact of PET/CT in bronchogenic carcinoma staging [14,15,16,17,18,19,20,21,22,23]. We used the eight TNM staging system which was already established since early 2017 in controversy to most of the studies used the older seventh edition of TNM staging as in a study done by Chao and Zhang [11].
Twelve cases out of 30 cases in group T representing 40% of cases showed a change in the TNM staging by PET/CT compared to CT alone, and this is almost close to the results found by Bury et al., Hicks et al., Taus et al., and Zheng et al. who concluded that 34%, 43%, 35%, and 35% of their cases showed change in their TNM staging when assessed by PET/CT [15, 18, 22, 23]. In controversy, Pieterman et al. found 62% of cases with a change in their TNM staging which is higher than our result [17] while Takeuchi et al. found the change in TNM staging in 28.7% of their cases [21].
In our study, out of the 12 cases in group T with a change in TNM staging, we found 8 cases representing 26.7% with the change in the TNM staging affected the surgical staging with subsequent changes in treatment strategy. The rest 4 cases showed no change in the surgical staging with no effect on the treatment plan. This is close to the result found by Bury et al. and Hicks et al. who found PET/CT impact on the management of 25% and 35% of their cases [15, 18].
The explanation of the TNM staging difference found between PET/CT compared to CT is summarized in Fig. 7 which highlights the effect of PET/CT in the precise and accurate delineation of the tumoral mass separating it from the surrounding nonmalignant pulmonary reaction, especially in T2 stage, and this is consistent with Chao and Zhang and Steinert [11, 24]. Aydin et al. stated that PET/CT measurements of the tumor size were more compatible with the histopathological size compared to CT, and this will affect the T staging which depends on the tumoral size [25]. Also, Hochhegger et al. studied the ability of PET/CT to differentiate the tumor and post-obstructive pulmonary changes which is considered challenging with T staging [26].
Four cases of our study showed changing in their TNM staging due to the difference in diagnosis of the nature of pulmonary nodules. The ability of PET/CT to differentiate the benign from the malignant nodules affects both T and M staging, and this is consistent with Volpi et al. who discussed the accuracy of PET/CT in differentiating the benign nodules from a malignant one [6].
PET/CT is a known modality to detect the malignant activity in the mediastinal lymph nodes more accurately compared to the CT which depends only on the nodal size with the accuracy reaching to about 90% in the diagnosis of malignant mediastinal lymphadenopathy [6, 11, 27].
CT depends only on the size of the lymph node during N staging. However, this carries a lot of fallacies as in post obstructive pneumonitis causing false-positive enlargement of the lymph nodes and also, normal-sized lymph nodes may be found to be metastatic on histopathological verification [28, 29]. Valopi et al. stated that patients with negative mediastinal lymph nodes on PET/CT can proceed to their management, according to the rest of T and M staging while the patients with positive nodal lesions may need further assessment via biopsy using mediastinoscopy for accurate histopathological verification avoiding false-positive results [7].
PET/CT is a known modality to detect the hidden bone marrow infiltrates being more accurate than CT and even bone scan to detect bony metastases, which are a common site for metastases in cases with bronchogenic carcinoma [6, 11, 27, 30]. Ten percent of patients with bronchogenic carcinoma found to have positive distant metastases by PET/CT not detected by CT alone [27].
On follow-up patients after starting their therapy (group F), we found nine cases (30%) with a change in therapeutic response assessment comparing the PERCIST criteria obtained by PET/CT and RECIST criteria obtained by CT alone, and this affects the treatment strategy and plan for seven cases (23.3%).
Multiple research papers are published studying the impact of PET/CT in the evaluation of the treatment response in cases with non-small cell lung cancer [31,32,33].
Although CT is the modality of choice on follow-up cases of lung cancer to evaluate the therapeutic response with RECIST criteria which is widely accepted and used for assessment, yet it still depends on the tumoral size change which shows some sort of variability between observers especially in irregular and speculated lesions. Also, CT cannot detect the activity changes occurred in response to therapy [34].
William et al. found a discrepancy between the CT RECIST and the histopathological results among 41% of the studied cases during follow-up after neoadjuvant chemotherapy [35] which was close to our results. However, in our study, we compared the result of the PET/CT to the CT alone, in controversy to William et al. who compared the PET/CT with the histopathology.
Our results were close to the result of Jimenez-Bonilla et al. and Marcus et al. who found that PET/CT resulted in a change in management between 30.19% and 28.1% of their patients, respectively, who did PET/CT to evaluate the therapeutic response [36, 37]. This was in controversy to Hicks et al. and You et al. who found a change in the management and therapeutic plane between 63.5% and 57% of their patients, respectively, when using PET/CT in the evaluation of therapeutic response [18, 38].
The main limitation of our study was the small sample size due to the high cost of the technique. A multi-centric study will be needed to obtain more accurate results when applied to a larger number of patients.
Conclusion
PET/CT has an important role in changing the staging of bronchogenic carcinoma as well as the judgment about the therapeutic response, which all lead to a significant change in therapeutic and management strategy, and this hopefully will improve the patient’s outcome and prognosis. PET/CT recently became a part of the international guidelines in the diagnosis and the follow-up of cases with bronchogenic carcinoma.
Availability of data and materials
Available on request with the corresponding author.
Abbreviations
- CT:
-
Computed tomography
- NSCLC:
-
Non-small cell lung cancer
- PERCIST:
-
PET/CT Response Criteria In Solid Tumors
- PET:
-
Positron emission tomography
- RECIST:
-
Response Evaluation Criteria In Solid Tumors
- SUV:
-
Standardized uptake value
- TNM staging:
-
Tumor, nodal, metastatic staging
References
Ningappa R, Ashwini C, Deepak S (2015) Role of MDCT in the evaluation of bronchogenic carcinoma. SSRG International Journal of Medical Science 2(3):21–23
American cancer society (2008) Cancer facts and figures 2008. American cancer society, Atlanta, Ga
Detterbeck FC, Boffa DJ, Kim AW et al (2017) The eighth edition lung cancer stage classification. Chest 151(1):193–203
Ravenel JG, Erasmus J (2013) Azygoesophageal recess. J Thorac Imaging 17:219–226
Ciliberto M, Maggi F, Treglia G et al (2003) Comparison between whole-body MRI and Fluorine-18-Fluorodeoxyglucose PET or PET/CT in oncology: a systematic review. Radiol Oncol 47(3):206–218
Volpi S, Ali J, Tasker A et al (2018) The role of positron emission tomography in the diagnosis, staging and response assessment of non-small cell lung cancer. Ann Transl Med 6(5):95
Purandare N, Rangarajan V (2015) Imaging of lung cancer: implications on staging and management. Indian Journal of Radiology and Imaging 25(2):109–120
Coche E (2016) Evaluation of lung tumor response to therapy: current and emerging techniques. Diagnostic and interventional imaging 97(10):1053–1065
Ichihara E, Kiura K, Takigawa N et al (2008) Pseudoprogression of lung cancer after concomitant chemoradiotherapy. Jpn J Clin Oncol 38(2):140–142
Wahl R, Jacene H, Kasamon Y et al (2009) From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 50:122S–150S
Chao F, Zhang H (2012) PET/CT in the staging of the non-small cell lung cancer. J Biomed Biotechnol 2012:8
Hyun OJ, Lodge M, and Wahl R (2016). Practical PERCIST: a simplified guide to PET response criteria in solid tumor 1.0. Radiology 280(2).
Eisenhauer E, Therasse P, Bogaerts J (2009) New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Lewis P, Griffin S, Marsden P et al (1994) Whole-body 18F-fluorodeoxyglucose positron emission tomography in preoperative evaluation of lung cancer. Lancet 344:1265–1266
Bury T, Dowlati A, Paulus P et al (1997) Whole-body 18FDG positron emission tomography in the staging of non-small cell lung cancer. Eur Respir J 10:2529–2534
Saunders CA, Dussek JE, O’Doherty MJ et al (1999) Evaluation of fluorine-18-fluorodeoxyglucose whole-body positron emission tomography imaging in the staging of lung cancer. Ann Thorac Surg 67:790–797
Pieterman RM, van Putten JW, Meuzelaar JJ et al (2000) Preoperative staging of non-small-cell lung cancer with positron-emission tomography. N Engl J Med 343:254–261
Hicks RJ, Kalff V, MacManus MP et al (2001) (18)F-FDG PET provides high-impact and powerful prognostic stratification in staging newly diagnosed non-small cell lung cancer. J Nucl Med 42:1596–1604
Hoekstra CJ, Stroobants SG, Hoekstra OS et al (2003) The value of [18F]fluoro-2-deoxy-D-glucose positron emission tomography in the selection of patients with stage IIIA-N2 non-small cell lung cancer for combined modality treatment. Lung Cancer 39:151–157
Schmücking M, Baum RP, Griesinger F et al (2003) Molecular whole-body cancer staging using positron emission tomography: consequences for therapeutic management and metabolic radiation treatment planning. Recent Results Cancer Res 162:195–202
Takeuchi S, Khiewvan B, Fox PS et al (2014) Impact of initial PET/CT staging in terms of clinical-stage, management plan, and prognosis in 592 patients with non-small-cell lung cancer. Eur J Nucl Med Mol Imaging 41:906–914
Taus Á, Aguiló R, Curull V et al (2014) Impact of 18F-FDG PET/CT in the treatment of patients with non-small cell lung cancer. Arch Bronconeumol 50:99–104
Zheng Y, Sun X, Wang J et al (2014) FDG-PET/CT imaging for tumor staging and definition of tumor volumes in radiation treatment planning in non-small cell lung cancer. Oncol Lett 7:1015–1020
Steinert HC (2011) PET and PET-CT of lung cancer. Methods Mol Biol 727:33–51
Aydin F, Dertsiz L, Budak E et al (2013) Measurements of tumor size using CT and PET compared to histopathological size in non-small cell lung cancer. Diagn Interv Radiol 19(4):271–278
Hochhegger B, Alves G, Irion K et al (2015) PET/CT imaging in lung cancer: indications and findings. J Bras Pneumol 41(3):264–274
McLoud TC (2003) The role of PET scanning in the evaluation of lung carcinoma. Cancer Imaging 3:83–84
Kerr K, Lamb D, Wathen C et al (1992) Pathological assessment of mediastinal lymph nodes in lung cancer: implications for non-invasive mediastinal staging. Thorax 47(5):337–341
Gupta N, Tamim W, Graeber G et al (2001) Mediastinal lymph node sampling following positron emission tomography with fluorodeoxyglucose imaging in lung cancer staging. Chest 120(2):521–527
Liu J, Dong M, Sun X et al (2016) Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: a meta-analysis. PLoS One 11:e0146195
De Ruysscher D, Nestle U, Jeraj R et al (2012) PET scans in radiotherapy planning of lung cancer. Lung Cancer 75:141–145
Weber WA, Petersen V, Schmidt B et al (2003) Positron emission tomography in non-small-cell lung cancer: prediction of response to chemotherapy by quantitative assessment of glucose use. J Clin Oncol 21:2651–2657
Patz EF, Connolly J, Herndon J (2000) Prognostic value of thoracic FDG PET imaging after treatment for non-small cell lung cancer. AJR Am J Roentgenol 174:769–774
Sheikhbahaei S, Mena E, Yanamadala A et al (2017) The value of FDG PET/CT in treatment response assessment, follow-up, and surveillance of lung cancer. AJR 208(2):420–433
William W, Pataer A, Kalhor N et al (2013) Computed tomography RECIST assessment of histopathological response and prediction of survival in patients with resectable non small cell lung cancer after neoadjuvant chemotherapy. J Thorac Oncol 8:222–228
Jimenez-Bonilla J, Quirce K, Martinez-Rodriguez I et al (2013) Diagnosis of recurrence and assessment of post recurrence survival in patients with extracranial non small cell lung cancer evaluated by 18F-FDG PET/CT. Lung Cancer 81:71–76
Marcus C, Paidpally V, Antoniou A et al (2015) 18F-FDG PET/CT and lung cancer: the value of fourth and subsequent posttherapy follow upscan for patient management. J Nucl Med 56:204–208
You J, Cline K, Gu C et al (2015) 18F-flurodeoxy-glucose positron-emission tomography-computed tomography to diagnose recurrent cancer. Br J Cancer 112:1737–1743
Acknowledgements
Not applicable
Funding
No fund
Author information
Authors and Affiliations
Contributions
AO and HK as authors both share together the writing, editing, data collection, and statistical analysis of the research in almost the same way. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It was taken from our institutional ethical committee (Radiology Department, Ain Shams University) with informed written consent taken from each patient. The reference number is not applicable as it was a departmental approval to use the patients’ data and material with no need to change the patient investigation with the PET/CT already requested during their management.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Osman, A.M., Korashi, H.I. PET/CT implication on bronchogenic carcinoma TNM staging and follow-up using RECIST/PERCIST criteria: a comparative study with CT. Egypt J Radiol Nucl Med 51, 16 (2020). https://doi.org/10.1186/s43055-020-0133-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-0133-5