Abstract
Background
Idiopathic granulomatous mastitis (IGM) is a rare benign chronic inflammatory condition of the breast and is most commonly seen in women of childbearing age. The etiology is uncertain, and an autoimmune association has been suggested with the diagnosis usually made by exclusion. The clinical and radiological features often mimic that of breast cancer and hence confirmed early diagnosis is required to avoid misdiagnosis and unnecessary delay in the treatment.
Results
The most common clinical presentation of granulomatous mastitis is unilateral palpable breast lump with or without associated pain. The typical ultrasound finding is an ill-defined, irregular heterogeneous, predominantly hypoechoic lesion with multiple tentacles. Histologic features show a well-defined non-necrotizing epitheloid granulomas along with Langhans type giant cells.
Conclusion
Imaging features mimic that of breast cancer, and final diagnosis of granulomatous mastitis always requires specific pathologic findings while excluding other causes.
Similar content being viewed by others
Background
Idiopathic granulomatous mastitis (IGM) is a rare benign chronic inflammatory condition of the breast, first described by Kessler and Wolloch in 1972 [1], and is most commonly seen in women of childbearing age [1]. It is frequently associated with lactation or hyperprolactinemia, and an increased incidence in non-white women has been proposed [2, 3]. The etiology is uncertain, and an autoimmune association has been suggested with the diagnosis usually made by exclusion. The clinical and radiological features often mimic that of breast cancer and hence confirmed early diagnosis is required to avoid misdiagnosis and unnecessary delay in the treatment. In addition, the finding of axillary lymphadenopathy seen in some of the patients with idiopathic granulomatous mastitis is concerning as it is also seen in cases of breast malignancy with nodal metastatic disease. Histologically, idiopathic granulomatous mastitis is characterized by formation of well-defined non-necrotizing granulomas [1, 4]. In this article, we discuss the clinical manifestations, imaging findings on ultrasound, and histopathological findings of this rare inflammatory condition of breast.
Methods
A retrospective study of pathology records from January 2013 to December 2017 from our institution was performed.
A total of 35 patients were included in our study, out of which there were 34 female patients and 1 male patient between the age group of 24 to 57 years whose diagnosis of idiopathic granulomatous mastitis was confirmed on histopathology.
Clinical records, imaging findings, and histopathology specimens of these patients were reviewed.
As most of the patients (n = 26) were young and less than 30 years old, ultrasound examination of the affected breast was performed using a high frequency transducer (7–10 MHz).
A definitive diagnosis was obtained by USG-guided FNA using 20–22 gauge needle or percutaneous core biopsy using 14 G–10 cm needle, and an average of 3 cores were obtained. Eight patients underwent surgical excision followed by pathological analysis of the sample. All the cytology and biopsy slides were reviewed and various parameters were noted: the presence of granulomas, giant cells, type of inflammatory cells, and presence of necrosis. The histochemical stains, Zeihl Neelson stain for acid fast bacilli (AFB), Periodic Acid Schiff (PAS) stain, and Gomorri Methenamine Silver (GMS) stain for fungus were also reviewed in all cases which were already done at the time of sample analysis.
Results
A total of 35 cases were diagnosed with idiopathic granulomatous mastitis.
The age group ranged from 24 to 57 years with the peak incidence in reproductive age group ranging from 26 to 35 years of age.

Clinical features
The most common clinical presentation was a unilateral palpable breast lump (n = 23) out of which 14 patients presented with lump associated with pain and 9 patients presented with lump without any associated pain. Isolated nipple discharge and external draining sinuses were noted in 5 and 3 patients, respectively. Three patients presented with mastalgia without any palpable lump. One patient presented with pain and swelling in both breasts at 1 month interval first on right side and then left. USG-guided biopsy done on the right side revealed features of idiopathic granulomatous mastitis. Ultrasound showed similar appearing lesions in both breasts. Only 2 patients had family history of breast cancer. None of the women had history of specific infection or any systemic disorder.
Clinical features | No. of patients |
|---|---|
Unilateral palpable breast lump | 23 |
With pain | 14 |
Without pain | 9 |
Nipple discharge | 5 |
External draining sinuses | 3 |
Mastalgia without any palpable lump | 3 |
Family history of breast cancer | 2 |
Imaging features
The typical ultrasound finding was an ill-defined, irregular heterogeneous, predominantly hypoechoic lesion with multiple tentacles (Fig. 1) which was seen in 22 patients, out of which 9 patients had associated dilatation of ducts. Multiloculated abscess collections (Fig. 2) were noted in 4 patients. Four patients had well-circumscribed hypoechoic mass mimicking fibroadenoma. Focal heterogeneous breast parenchyma representing mastitis without any obvious mass was seen in 5 patients. External draining sinuses (Fig. 3) were noted in 3 patients. Skin thickening (Figs. 3c and 4b) was noted in few patients. Reactive ipsilateral lymphadenopathy was noted in 22 patients with few nodes showing irregularly thickened cortex (Fig. 2c). Lesions were present in either upper outer quadrant (n = 20) or subareolar/periareolar area (n = 15).
Imaging findings | No. of patients |
|---|---|
Ill-defined, irregular, heterogeneous (predominantly hypoechoic) lesions with multiple tentacles | 22 |
Multiloculated abscess collections | 4 |
Well-circumscribed hypoechoic mass | 4 |
Focal heterogeneous breast parenchyma | 5 |
External draining sinuses | 3 |
Reactive axillary lymphadenopathy | 22 |
Ultrasound of a 28-year-old female diagnosed with idiopathic granulomatous mastitis, who presented with pain and swelling in the left breast. a, b Ultrasound showing an ill-defined irregular hypoechoic lesion with tubular tentacle-like extensions (red arrows). c Color flow imaging showing increased internal vascularity. d Histopathology shows Langhans type of giant cells admixed with inflammatory cells, predominantly lymphocytes (H&E × 100)
A 38-year-old female diagnosed with idiopathic granulomatous mastitis, who presented with pain and swelling in the left breast. a Clinical picture showing swelling and redness in the left breast in areolar region. b Ultrasound showing irregular hypoechoic collection and inflammatory changes in surrounding breast parenchyma. c Enlarged lymph node in axilla showing irregularly thickened cortex. d Histopathology showing foreign body and Langhans type of giant cells with epithelioid cells, admixed with granulation tissue—H&E × 100
A 29-year-old female diagnosed with idiopathic granulomatous mastitis, who presented with complaints of pus discharge from sinus tract in the left breast with associated pain. a Clinical picture showing external sinus tract with redness and swelling in the left breast. b A sinus tract (green arrow) between the parenchymal collection and subcutaneous collection to the skin surface. c Ultrasound showing subcutaneous edema and significant skin thickening. d Histopathology showing epithelioid granuloma with Langhans type of giant cells—H&E × 200
A 31-year-old female diagnosed with idiopathic granulomatous mastitis, who presented with complaints of pus discharge from sinus tract in the left subareolar region with associated pain. a Clinical picture showing external sinus tracts with redness in the surrounding breast. b Extended view on high resolution ultrasound showing multiple collections (green arrow), surrounding heterogenous parenchyma (black arrow) & skin thickenning (red arrow head)
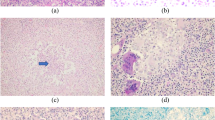
Histopathological features
Microscopic features showed a well-defined non-necrotizing epitheloid granulomas along with Langhans type giant cells (Figs. 1d, 2d, and 3d) in all of the cases while few of them showed additional fibrocystic changes and few had acute component with presence of sheets of neutrophils. The histochemical stains for AFB and fungus were negative in all the cases.
Discussion
Idiopathic granulomatous mastitis is a rare benign chronic inflammatory disease of the breast. The etiology had been uncertain, and it had been postulated that IGM results from a localized autoimmune response to the retained or extravasated fat- or protein-rich secretion in the breast ducts during childbearing age due to a previous hyperprolactinemia [5]. The response to steroids supports this autoimmune nature of the disease [6]. However, histological features of an immune-mediated inflammation, such as vasculitis and predominantly plasma cell and lymphoid aggregates, are not seen in IGM [7]. Idiopathic granulomatous mastitis is not associated with trauma, specific infections, or foreign material [1].
Idiopathic granulomatous mastitis is most commonly seen in premenopausal women, most often in women of childbearing age. The mean age at presentation in our study was 31 years [8]. The most common presentation was unilateral breast lump with or without pain. The distribution of IGM is usually unilateral, with bilateral cases reported less often, in 1–9% of cases [9,10,11]. Prevalence of peripheral, subareolar, and diffuse IGM lesions of 50%, 25%, and 25%, respectively, has been reported [8, 10].
Imaging features of idiopathic granulomatous mastitis have not been described frequently. It manifests in a variety of non-specific appearances. The most common imaging finding of idiopathic granulomatous mastitis in our study was an ill-defined, heterogeneous predominantly hypoechoic lesion with irregular margins and tentacle-like extensions (Fig. 1) (23/35). The tubular extensions demonstrate that idiopathic granulomatous mastitis insinuates around the breast lobules rather than destroys them [2]. These findings were similar to those previously reported by Han et al. [12], Yilmaz et al. [13], and Lee et al [10]. Nine patients had associated dilated ducts. Doppler ultrasound showed the lesion and the surrounding tissue to be hypervascular (Fig. 1c) as stated by Fazzio et al. [9] and Al-Khawari et al. [14].
Ultrasound is also useful in guiding fine needle aspiration (FNA) and core needle biopsy.
Fazzio et al. [9], Yilmaz et al. [13], and Memis et al. [15] identified a focal asymmetric density as the most frequent pattern. Han et al. [12] described multiple small masses or a large focal asymmetric density. A study in 11 women by Lee et al. [4] showed an irregular ill-defined/obscured mass to be the most common finding. One patient in our study showed an equal density irregular lesion (Fig. 5) with obscured margins, while other patient had normal mammography.
MR findings of idiopathic granulomatous mastitis are variable. Heterogeneous ill-defined masses and non-mass enhancement with mixed kinetics were described by Fazzio et al. [9] as the most common pattern in their study. One patient in our study showed similar findings of regional non-mass-like enhancement with prominent duct with wall thickening and surrounding inflammatory changes (Fig. 6). Irrespective of kinetics, the affected parenchyma demonstrates intense enhancement compared to uninvolved tissue. Another patient showed multiple round to oval well defined lesions appearing predominnatly hypointense on T1WI & hyperintense on T2WI. All these lesions showed peripheral enhancement after the administration of intravenous gadolinium. Surrounding parenchyma showed inflammatory changes. Few non-mass-like enhancing foci were also seen with adjacent focal skin thickening (Fig. 7). These findings were similar to those described by Gautier et al. [2] and Oztekin et al. [16]. In advanced disease, larger fluid collections can be seen interspersed within abnormal enhancement, with or without sinus tracts extending to the skin surface [2]. Involved parenchyma displays restricted diffusion in the majority of cases with consistently lower mean ADC values (1.0 × 10−3 mm2/s) than what is observed for normal breast parenchyma (2.3 × 10−3 mm2/s). Although ADC values in IGM are falsely positive for malignancy, time intensity curves are more benign, consistent with inflammation. Additional MR imaging findings include axillary lymphadenopathy, nipple and/or skin thickening, nipple retraction, sinus tracts, and parenchymal distortion [2, 9]. Importantly, MR provides the best estimate of disease extent and contralateral breast involvement.
Pathologically, idiopathic granulomatous mastitis is characterized by well-defined non-necrotizing granulomas with collection of epithelioid cells, Langhans type of multinucleated giant cells, and lymphocytes with no evidence of microorganisms. The presence of non-caseating granuloma is the characteristic finding in a biopsy. At times, there can be a coalescence of the granulomas and microabscess formation. But usually, these granulomas lack caseation necrosis. The presence of neutrophils and microabscess formation warrants a careful search for fungal hyphae and spores, which again needs to be confirmed by histochemical stains. Foreign body type of giant cells should prompt a search for refractile foreign body material.
It should be differentiated from other causes of chronic inflammatory breast diseases such as tuberculosis, Wegener’s granulomatosis, sarcoidosis, fungal infection, duct ectasias, carcinoma, and fat necrosis, where again granulomas may be the presenting feature under the microscope [17].
Pluguez-Turull et al. [18] described the role of a breast radiologist in the surveillance, pre-surgical, and post-treatment evaluation of HPE-confirmed idiopathic granulomatous mastitis is as follows:
- (a)
Establish the multiplicity and location of IGM lesions
- (b)
Document the size of the lesion(s)
- (c)
Identify abscess formation and the related possibility for intervention
- (d)
Evaluate the treatment response by assessing the stability or interval change in the lesion(s)
- (e)
Identify metachronous disease and local recurrence at imaging surveillance
A definite diagnosis of idiopathic granulomatous mastitis always requires a histopathological analysis since the clinical and imaging features of granulomatous mastitis are very non-specific [1, 8]. As FNA is more easily available and more cost-effective, it is often the first option for tissue sampling and gives faster results than core biopsy. FNA is useful in the initial differentiation of an inflammatory breast process from malignancy. However, biopsy is more superior and specific than FNA in distinguishing malignancy from inflammatory condition and for accurate tissue diagnosis.
Conclusion
Idiopathic granulomatous mastitis is a rare inflammatory benign breast disease commonly occurring in women of childbearing age with clinical and imaging features similar to inflammatory breast carcinoma. Final diagnosis of granulomatous mastitis always requires specific pathologic findings while excluding other causes.
Availability of data and materials
Not applicable.
Abbreviations
- AFB:
-
Acid fast bacilli
- FNA:
-
Fine needle aspiration
- HPE:
-
Histopathology
- IGM:
-
Idiopathic granulomatous mastitis
- USG:
-
Ultrasound
References
Kessler E, Wolloch Y (1972) Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 58(6):642–646 [Medline]
Gautier N, Lalonde L, Tran-Thanh D et al (2013) Chronic granulomatous mastitis: imaging, pathology and management. Eur J Radiol 82(4):e165–e175
Al-Khaffaf B, Knox F, Bundred NJ (2008) Idiopathic granulomatous mastitis: a 25-year experience. J Am Coll Surg 206(2):269–273
Going JJ, Anderson TJ, Wilkinson S, Chetty U (1987) Granulomatous lobular mastitis. J Clin Pathol 40:535–540
Cserni G, Szajki K (1999) Granulomatous lobular mastitis following drug-induced galactorrhea and blunt trauma. Breast J 5(6):398–403 [PubMed]
DeHertogh DA, Rossof AH, Harris AA, Economou SG (1980) Prednisone management of granulomatous mastitis. N Engl J Med 303:799–800
Fletcher A, Magrath IM, Riddell RH, Talbot IC (1982) Granulomatous mastitis: a report of seven cases. J Clin Pathol 35:941–945
Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G (2009) Granulomatous lobular mastitis: imaging, diagnosis, and treatment. Am J Roentgenol 193(2):574–581
Fazzio RT, Shah SS, Sandhu NP, Glazebrook KN (2016) Idiopathic granulomatous mastitis: imaging update and review. Insights Imaging 7(4):531–539. https://doi.org/10.1007/s13244-016-0499-0
Lee JH, Oh KK, Kim EK, Kwack KS, Jung WH, Lee HK (2006) Radiologic and clinical features of idiopathic granulomatous lobular mastitis mimicking advanced breast cancer. Yonsei Med J 47:78–84
Aghajanzadeh M, Hassanzadeh R, Alizadeh Sefat S et al (2015) Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast 24(4):456–460
Han BK, Choe YH, Park JM et al (1999) Granulomatous mastitis: mammographic and sonographic appearances. AJR 173:317–320
Yilmaz E, Lebe B, Usal C, Balci P (2001) Mammographic and sonographic findings in the diagnosis of idiopathic granulomatous mastitis. Eur Radiol 11:2236–2240
Al-Khawari HA, Al-Manfouhi HA, Madda JP, Kovacs A, Sheikh M, Roberts O (2011) Radiologic features of granulomatous mastitis. Breast J 17(6):645–650
Memis A, Bilgen I, Ustun EE, Ozdemir N, Erhan Y, Kapkac M (2002) Granulomatous mastitis; imaging findings with histopathologic correlation. Clin Radiol 57:1001–1006
Oztekin PS, Durhan G, Nercis Kosar P, Erel S, Hucumenoglu S (2016) Imaging findings in patients with granulomatous mastitis. Iran J Radiol 13(3):e33900. https://doi.org/10.5812/iranjradiol.33900
Imoto S, Kitaya T, Kodama T, Hasabe T, Mukai K (1997) Idiopathic granulomatous mastitis: case report and review of the literature. Jpn J Clin Oncol 27:274–277
Pluguez-Turull CW, Nanyes JE, Quintero CJ, Alizai H, Mais DD, Kist KA, Dornbluth NC (2018) Idiopathic granulomatous mastitis; manifestations at multimodality imaging and pitfalls. RadioGraphics 38(2):330–356
Acknowledgements
The author would like to thank his great and beloved teachers, mother, father, husband, and the hospital management for their moral support and patience.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PM collected the patient data, obtained consent from the patients, and followed up the cases; written the full manuscript of the article; and has approved the submitted version of the study. BD was the radiologist who performed the ultrasound scans to all the patients and did the ultrasound-guided FNAC/biopsy as required, guided the interpretation of data and substantively revised it, and has approved the submitted version of the study. LDJ was the pathologist who reviewed and reported all the pathology slides, guided the interpretation of data and substantively revised it, and has approved the submitted version of the study. RR is a Professor Of Surgery, Sri Ramachandra Institute of Higher Education & Research (SRIHER). She clinically examined & refereed the patients for imaging also treated the patients accordingly. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval has been obtained for the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Manogna, P., Dev, B., Joseph, L.D. et al. Idiopathic granulomatous mastitis—our experience. Egypt J Radiol Nucl Med 51, 15 (2020). https://doi.org/10.1186/s43055-019-0126-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-019-0126-4