Abstract
Background
Hepatic mesenchymal hamartoma (HMH) is the second most common benign hepatic tumor in the pediatric age group. The etiology of HMH is unclear. Theories include abnormal hepatic mesenchyme, a reactive change or a proliferative lesion. The condition can present prenatally in USG as a mass, high output cardiac failure, pulmonary hypertension, respiratory distress, and abdominal distension or mass in older children. We present this case to discuss an extremely rare presentation of a comparatively rare disease and to emphasise the need for a high index of suspicion even if the patient presents with symptoms common for that age.
Case presentation
A 7-day-old male baby with an uneventful antenatal period, born by vaginal delivery, with a birth weight of 3.1 kg and normal APGAR scores, presented with jaundice, poor feeding, and labored breathing noticed on the same day itself. Examination revealed a grossly distended abdomen with a mass of size 8 × 7 cm occupying the right side down to the right iliac fossa, crossing midline and dullness continuous with liver dullness. On investigation an abnormal liver function test with unconjugated hyperbilirubinemia was seen. USG and CECT abdomen were suggestive of HMH with close proximity to hepatic vessels. Exploratory laparotomy and near total excision with marsupialisation was done. Histopathology report was suggestive of HMH. A 2-year follow-up was normal.
Conclusion
This case of HMH presented as neonatal jaundice with unconjugated hyperbilirubinemia which is a rarity. We had to limit our surgery to near total excision and marsupialisation due to its proximity to vascular structures.
Similar content being viewed by others
Background
Hepatic mesenchymal hamartoma (HMH) is the second most common benign hepatic tumor after hemangioendothelioma and the third most common of all the hepatic tumors in Pediatric population [1]. It has got a male preponderance and 80% of lesions develop within the first 2 years of life [2].
The etiology of HMH is unclear. There are several theories regarding etiogenesis. One theory states that the lesion occurs due to an abnormal development of primitive mesenchyme at the level of the hepatic ductal plate, leading to abnormal bile ducts [3]. An alternate theory considers the lesion as reactive rather than developmental. An abnormal blood supply to an otherwise normal hepatic parenchyma causes ischemic necrosis, leading to reactive cystic changes within that portion of the liver [4]. The third theory postulates HMH to be a proliferative lesion. A local increase in fibroblast growth factor 2(FGF-2) secretion stimulates the growth of the spindle cells to form the mesenchymal hamartoma. The angiogenic potential of FGF-2 leads to an increase in vascularity associated with these lesions [5]. Possible genetic causes have also been proposed. These include translocation/deletion of chromosome 19q13.4, loss of heterozygosity due to multiple monosomies, aneuploidy, and possible alterations of the MALAT1 gene [6].
Routine antenatal ultrasounds have helped in the prenatal diagnosis of HMH. Prenatally detected masses could be cystic or solid and are usually associated with congestive cardiac failure or fetal hydrops. They may present with high-output cardiac failure, pulmonary hypertension and respiratory distress. The mortality rate of prenatally and perinatally detected lesions are 30% and 35% respectively [7]. In older children, HMH presents as progressive abdominal distention or an abdominal mass or both. Occasionally vomiting can occur due to gastrointestinal compression.
We present this case to discuss an extremely rare presentation of a comparatively rare disease and to emphasise the need for a high index of suspicion even if the patient presents with symptoms common for that age.
Case presentation
A 7-day-old male baby born to a 29 years old mother hailing from Kidangoor, a village in Kerala State of India, presented with jaundice and labored breathing since postnatal day 7. The baby was born at full term (37 weeks) by normal vaginal delivery. He had a birth weight of 3.1 kg and normal APGAR Scores. The antenatal period was uneventful. Antenatal ultrasound scans were normal. There were no records of any significant illnesses or drug intake in the mother. The baby was the 3rd child of a non-consanguineous marriage. He has 2 siblings who are normal. Baby was breastfed soon after birth, passed meconium and urine within 4 h. The baby was discharged on postnatal day 4. On postnatal day 7, the baby was noticed to be jaundiced with poor feeding and labored breathing and was brought back to the hospital.
On examination, the baby was hemodynamically stable; heart rate was 150 beats per minute, respiratory rate 52 per minute and oxygen saturation in room air was 95%. Jaundice was present involving palms and soles. Anthropometric measurements were: length 50.5 cm, weight 3.1 kg and head circumference of 34.8 cm. The BIND score was 0.
The abdomen was grossly distended. Palpation revealed a firm mass of 8 × 7 cm in size occupying the entire right side of the abdomen down to the right iliac fossa and crossing the midline. It was dull on percussion and was continuous with the liver dullness.
Blood investigations showed abnormal liver function tests with indirect hyperbilirubinemia. Other blood investigations were normal (Table 1).
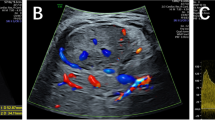
X-ray abdomen revealed a soft tissue shadow occupying the entire right side of the abdomen with bowel loops pushed to the right side (Fig. 1A). USG abdomen revealed a large multiseptated cystic lesion involving the right side of the liver (Fig. 1B).
CECT abdomen showed a large cystic lesion 7.6 × 6 × 4.6 cm with hyperdense areas noted in segments 6 and 7 of liver, extending down to the right iliac fossa (Fig. 2). The lesion was seen displacing the right hepatic vein and compressing the IVC. The right branch of common hepatic artery was seen coursing close to the posterior aspect of the lesion. The possibility of the lesion being mesenchymal hamartoma was considered.
The baby was started on intravenous antibiotics and supportive measures. Jaundice was managed with phototherapy based on the AAP hour specific nomogram. We attempted to aspirate the cyst under USG guidance and decompress the abdomen but we were unsuccessful. Hence, we proceeded with an emergency laparotomy through a right upper transverse incision. It revealed a large multiloculated cystic lesion with hemorrhagic areas filling the entire right side of the abdomen (Fig. 3). The cyst was seen to be arising from the posterosuperior aspect of the liver, pushing the entire liver to the midline and opposite side. There were dense adhesions between the tumor capsule, bowel and abdominal wall. Entire tumor was filled with altered blood. Capsule was very friable. After separating the adhesions, near total excision of the tumor (sparing the area of the vascular pedicle) and marsupialisation were done.
Postoperatively the child was electively ventilated with other supportive measures and extubated the next day.
Histopathology was indicative of a cystic lesion which showed mesenchymal tissue with myxoid stroma and hepatocytes. No normal bile ducts or portal triads could be seen in the liver tissue. Marked hemorrhage was seen in the cyst cavity and cyst wall. All findings were in favor of mesenchymal hamartoma of liver (Fig. 4).
On follow-up, the baby was a healthy 2-year-old boy with a normal LFT and a sonologically normal liver.
Discussion
The occurrence of HMH is a rare event even though it is the second most benign hepatic tumor of childhood [4]. Hamartoma is an overgrowth of tissues, indigenous to the site. Histologically HMH consists of a mixture of cysts, bile ducts, hepatocytes, and mesenchyme [4].
Neonatal hepatic mesenchymal hamartoma (HMH) usually presents as an asymptomatic mass which is detected incidentally on ultrasound. It can also present with symptoms like abdominal distention, pain and respiratory distress. Other features include cardiac failure, anorexia, vomiting, poor weight gain, vascular steal and thrombocytopenia, intralesional bleeding, pulmonary hypertension, tumor rupture, ascites, pedal edema, obstructive jaundice, and smooth, and large non-tender hepatomegaly [8].
The differential diagnosis of HMH could be any abdominal cystic lesion in a newborn like mesenteric cyst, duplication cyst, hepatoblastoma, teratoma, lymphangioma, choledochal cyst, and renal cyst [8]. These could all be differentiated from HMH using imaging studies.
The initial investigation is plain X‐ray abdomen. It may show calcification or soft tissues mass with displacement of bowel [8]. Ultrasound, computed tomography, and magnetic resonance imaging of HMH may show a multiloculated cystic tumor with varying amounts of solid components. With ultrasound scan, the presence of thin mobile septae and round hyper-echoic parietal nodules within the cyst is highly suggestive of HMH.
Cases of HMH presenting with jaundice are rare but described earlier in the literature. These were predominantly cases of obstructive jaundice as a result of biliary tract compression by the mass. In 1982 Henrik Ehren et al. published a series of 48 cases of benign liver tumors in infancy. The author described a newborn girl who was admitted to the hospital with hepatomegaly and jaundice. The reason for jaundice was found to be a hamartoma partially obstructing the extrahepatic bile ducts [9]. Heller. K et al. in 1992, described another case concerning a 2-year-old female child, who was found to have a hamartoma of the liver located centrally in the hilar region. She presented with severe biliary obstruction which developed rapidly and was surgically treated [10].
Our patient presented as a case of neonatal jaundice (indirect hyperbilirubinemia). This can be explained by the hemorrhage into the tumor causing heme catabolism leading to excess bilirubin production.
Cases of HMH with indirect hyperbilirubinemia are much rarer when compared to direct hyperbilirubinemia. A case of a 3-week-old male newborn with HMH and mild indirect hyperbilirubinemia was described by Moaied A. Hassan in 2020. But the presenting complaint was not jaundice but abdominal distension and respiratory distress [11].
Treatment options include enucleation of small lesions or marsupialisation into the peritoneal cavity in case of large lesions. However, the gold standard of treatment is complete surgical excision with a margin of normal tissue of the liver. This is to avoid local recurrence and long-term malignant transformation [11]. In our case, we did a near total excision with marsupialisation. Complete excision was not feasible as it was in close relation with hepatic vasculature.
Conclusion
Even though hepatic mesenchymal hamartoma is a rare benign hepatic tumor of infancy, it can present as a surgical emergency. Our case presented as unconjugated neonatal jaundice, which is a rarity. Even though complete excision is desirable we had to limit our surgery to near total excision and marsupialisation due to its proximity to vascular structures.
Availability of data and materials
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HMH:
-
Hepatic mesenchymal hamartoma
- USG:
-
Ultrasonogram
- CECT:
-
Contrast enhanced computed tomography
- IVC:
-
Inferior vena cava
- LFT:
-
Liver function test
- BIND:
-
Bilirubin induced neurologic dysfunction
- AAP:
-
American Academy of Pediatrics
References
Stocker JT (2001) Hepatic tumors in children. Clin Liver Dis 5(1):259–81, viii−ix. https://doi.org/10.1016/s1089-3261(05)70163-x. PMID: 11218918
Saeed O, Saxena R (2017) Primary mesenchymal liver tumors of childhood. Semin Diagn Pathol 34:201–207
Stocker JT, Ishak KG (1983) Mesenchymal hamartoma of the liver: report of 30 cases and review of the literature. Pediatr Pathol 1:245–267
Helal A, Nolan M, Bower R et al (1995) Pathological case of the month. Mesenchymal hamartoma of the liver. Arch Pediatr Adolesc Med. 149:315–316
von Schweinitz D, Dammeier BG, Gluer S (1999) Mesenchymal hamartoma of the liver–New insight into histogenesis. J Pediatr Surg 34:1269–1271
Shehata BM, Gupta NA, Katzenstein HM et al (2011) Undifferentiated embryonal sarcoma of the liver is associated with mesenchymal hamartoma and multiple chromosomal abnormalities: a review of eleven cases. Pediatr Dev Pathol 14:111–116
Cornette J, Festen S, van den Hoonaard TL et al (2009) Mesenchymal hamartoma of the liver: a benign tumor with deceptive prognosis in the perinatal period. Case report and review of the literature. Fetal Diagn Ther 25:196–202
Stringer MD, Alizai NK (2005) Mesenchymal hamartoma of the liver: a systematic review. J Pediatr Surg 40:1681–1690
Ehren H, Mahour GH, Isaacs H (1983) Benign liver tumors in infancy and childhood: report of 48 cases. Am J Surg 145(3):325–329
Heller K, Markus BH, Waag KL (1992) Central hamartoma of the liver in a child. Eur J Pediatr Surg 2(2):108–109. https://doi.org/10.1055/s-2008-1063415. PMID: 1610748
Hassan MA (2020) Giant solid mesenchymal hamartoma of the liver in a neonate: case report. Ann Pediatr Surg 16:29. https://doi.org/10.1186/s43159-020-000
Acknowledgements
We acknowledge our former Head of the department and Professor, Dr. S Sethunath, our present Head of the department and Professor, Dr. K Sivakumar, and Dr. Vishnuraj T, Assistant professor for their valuable input in the study. We acknowledge Dr. Priya P V, Associate Professor, Department of Pathology for her valuable help in interpreting the histopathology. We acknowledge Dr. Sajitha Krishnadas, Professor and Head of the Department, Department of Radiodiagnosis for her valuable help in interpreting the USG and CECT findings. We acknowledge Dr. Rejimol, Associate professor, Department of Anesthesia for her skilled management during intraoperative period.
Funding
No funding was obtained.
Author information
Authors and Affiliations
Contributions
SJM and AP did the active workup and surgical management of the case. BMC and RKM helped in the initial diagnosis and did the active pre-operative and post-operative management of the patient. All the authors participated in writing and reviewing the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from The Scientific review committee, Department of Pediatric Surgery, ICH, Government Medical College, Kottayam. Written informed consent was obtained from the parents of the child.
Consent for publication
Written informed consent was obtained from the parents of the child.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mathews, S.J., Perveen K, A., Chandy, B.M. et al. Hepatic mesenchymal hamartoma masquerading as neonatal unconjugated hyperbilirubinemia: a case report. Egypt Pediatric Association Gaz 71, 50 (2023). https://doi.org/10.1186/s43054-023-00199-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00199-2