Abstract
Background
Analysis of free DNA molecules shed from tumour cells in plasma of patients referred as circulating tumour DNA (ctDNA) with reference to physiological circulating cell-free DNA (cfDNA) is nowadays exploited as liquid biopsy and is considered a new emerging promising biomarker for diagnosis, selection of proper treatment, and prognosis of cancer. DNA integrity index (DII) is assessed by calculating the ratio between the concentration of long cfDNA strands released from tumour cells (ALU247) and the short strands released from normal cells (ALU115). The aim of the current study was to evaluate DII as a potential diagnostic and prognostic biomarker of NSCLC.
Methods
Our study included 48 NSCLC patients diagnosed as primary NSCLC before starting treatment, 30 COPD patients diagnosed clinically, radiologically, and subjected to chest high-resolution computerized tomography, and 40 healthy controls. cfDNA concentration and DII were measured by quantitative real-time polymerase chain reaction (qPCR).
Results
ALU115, ALU247, and DII were significantly higher in NSCLC compared to COPD patients (p < 0.0001) and controls (p < 0.0001) and in COPD patients compared to control subjects (p < 0.0001). DII positively correlated with the stage of tumour (p = 0.01), tumour metastasis (p = 0.004), and with adenocarcinoma compared to other histopathological types (p = 0.02). To evaluate clinical utility of DII in NSCLC, ROC curve analysis demonstrated an AUC of 0.91 at a cut-off value of 0.44 with total accuracy = 85.6%, sensitivity = 90%, specificity = 83%, PPV = 78.1%, and NPV = 92.1%.
Conclusion
cfDNA and DII represent a promising diagnostic and prognostic tool in NSCLC. This type of noninvasive liquid biopsy revealed its chance in the screening, early diagnosis, and monitoring of NSCLC.
Similar content being viewed by others
Background
Lung cancer, especially non-small cell lung cancer (NSCLC) that accounts for 80–85% of lung cancer cases, represents the foremost lethal malignancy in Egypt; however, it is the fourth most prevalent cancer in men, and it is relatively rare in women [1]. The latest WHO data published in 2020 that lung cancer mortality represented 1.06% of total deaths in Egypt, with an age-adjusted death rate of 8.02 per 100,000 of population, ranking Egypt no. 115 within the world [2].
Cancer screening and early detection tests are of critical importance to enhance treatment effectiveness and subsequently decrease cancer morbidity and mortality rate [3]. Currently, tissue biopsies are considered the gold standard for tumour profiling. However, this method in addition of being invasive, risky, and not easily obtained for a few anatomical locations, it provides an incomplete analysis of the tumour profile due to tumour heterogeneity that requires multiple biopsies. Moreover, biopsies can hardly detect discrepancies between primary and metastatic lesions, beside its inability to detect the continuous genetic changes that may result in new mutations and subsequent resistance to treatment, hence the ineffectiveness of biopsies to observe disease progression [4].
Researches on liquid biopsies using different biological fluids of patients provide genomic [5], epigenetic [6], proteomic, and transcriptomic [7] evidence about tumours and metastasis. The clinical utilization of liquid biopsies has been suggested to improve cancer screening [8], diagnosis [9], prognosis [10, 11], monitoring [12], assessing treatment response [13, 14], and detecting treatment-resistant clones [15].
Circulating cell-free DNA (cfDNA) is believed to be the most hopeful biomarker, being the simplest to perform in clinical routine, and various applications have been developed for diagnostic, therapeutic, and prognostic purposes [16]. A portion of this DNA is shed from tumour cells into the blood stream and referred to as circulating tumour DNA (ctDNA). In healthy individuals, apoptosis of cells generates short fragments of DNA < 200 bp [17, 18], while necrosis of tumour cells results in shedding of longer DNA fragments [17]. The Arthrobacter luteus (ALU) repeats, 300 bp long, are the most prevailing repeated sequences all over the human genome. They account for more than 10% of the human genome [19]. The ratio between long- and short-generated DNA fragments, ALU247 and ALU115, respectively, is referred to as DNA integrity index (DII) [20].
A significantly increased DII was demonstrated in colorectal cancer [18], hepatitis C virus-related hepatocellular carcinoma [21], breast cancer with a positive correlation with TNM staging [22, 23], and in bronchogenic carcinoma [24,25,26,27].
The aim of this study was to evaluate the clinical utility of DII as a potential noninvasive biomarker in NSCLC and its role in diagnosis and prognosis.
Methods
Subjects
This work was done in National Research Centre (NRC) in cooperation with National Cancer Institute (NCI) and Chest Department of Cairo University Hospital (Kasr-ElAiny). This case–control study included 48 unrelated adult patients with primary lung cancer, 30 COPD patients, and 40 unrelated controls. All subjects included in the study were questioned about the lifetime smoking history, residence, occupational history, and family history of cancer. Detailed clinical examination and chest radiographic evaluation, i.e. high-resolution computerized tomography (HRCT), were carried out for diagnosis of COPD patients. Specimens obtained either by open biopsy or via bronchoscopy were assessed for lung cancer by histopathological evaluation. Venous blood sample was drawn from each subject to measure the absolute concentration of ALU247 and ALU115 and to calculate DII. Patients’ inclusion criteria were primary lung cancer confirmed by histopathology, age ≥ 18, and anti-tumour therapy either surgery, chemotherapy, or radiotherapy has not been started yet. Previous history of cancer, metastasis from other organs, pulmonary fibrosis, acute interstitial pneumonia, radio/chemotherapy, or any anticancer therapy received anytime earlier than the study were all considered exclusion criteria for the patients.
The study was permitted by the Ethics Committee of the National Research Centre, registration number 19–234. Informed written consent was obtained from all subjects after being fully aware of the nature of the study.
Samples collection and processing
A total of 5-ml venous blood samples were collected in EDTA vacutainers from newly diagnosed lung cancer patients, COPD patients, and controls and centrifuged at 3000 rpm for 10 min at 4 °C, then plasma layer was removed carefully and spun again for further 5 min at 2500 rpm for better purity, and, finally, plasma was put in storage at − 80 °C until PCR analysis.
Measurement of cfDNA concentration by quantitative real-time PCR
cfDNA was extracted from plasma using the QIAamp DNA Mini kit (Qiagen, Hilden, Germany) according to manufacturer’s instructions. cfDNA concentrations in plasma samples were evaluated by measuring ALU115 and ALU247 repeats. All primers were supplied from Invitrogen (Thermo Fisher, Scientific Inc., USA).
Primers’ sequences were ALU115 forward: 5′-CCTGAGGTCAGGAGTTCGAG-3′ and reverse: 5′-CCCGAGTAGCTGGGATTACA-3′ and ALU247 forward: 5′-GTGGCTCACGCCTGTAATC-3′ and reverse: 5′-CAGGCTGGAGTGCAGTGG-3′.
Quantitative real-time PCR was conducted on StepOne real-time PCR (Applied Biosystems, Foster City, CA, USA) using FastStart Universal SYBR Green Master Mix (Life Technologies-Thermo Fisher, Scientific Inc., USA). PCR amplification was performed with pre-activation of DNA polymerase at 95 °C for 15 min, followed by 40 cycles of denaturation at 94 °C for 15 s, annealing at 64 °C for 30 s, extension at 72 °C for 30 s, and extension at 72 °C for 10 min.
Standard curves for ALU-247 and ALU-115 were obtained using human genomic DNA control PCR-ready concentration (Applied Biosystems) with serial dilutions from 10 ng/μL to 0.01 pg/μL to calculate the absolute concentration of ALU247 and ALU115 in each sample. Integrity index was calculated as ALU247/ALU115.
Statistical analysis
Collected data and clinical results were tabulated and statistically analysed using IBM SPSS version 20.0 software (Statistical Package for Social Science). Quantitative data were expressed as mean ± standard deviation (SD) for normally distributed data and compared using one-way ANOVA test for multiple comparisons and Student’s t-test for two groups comparison. Post hoc test has been conducted following ANOVA test to determine the differences between pairs within the groups. The qualitative data were expressed as number and percentage and then compared using the chi-square test (χ2). Skewed data were expressed as median and interquartile range (IQR) and compared using Mann–Whitney U-test for two groups and Kruskal–Wallis test for multiple groups. Donn’s test has been conducted following Kruskal–Wallis test to determine the differences between pairs within the groups. Point-biserial correlation (rpb) analysis has been used to find potential correlation between the integrity index and tumour characteristics. ROC curve analysis was used to assess the validity of variables as diagnostic tools (95% CI). p-value < 0.05 was considered significant (2-tailed).
Results
A total number of 118 individuals have been studied with mean age 54.8 ± 10.9 and age range (24–85 years). They were classified into 48 patients with lung cancer with mean age 58.6 ± 11.1, 30 patients with COPD with mean age 57.7 ± 9.0, and 40 healthy control with mean age 48.0 ± 9.0 years. All groups were matched in sex (p > 0.05). Significant higher frequencies of smoking and pack year index were observed among cancer and COPD patients than in control group (p < 0.0001). Significant higher values of ALU247 and DII were detected in lung cancer patients compared to COPD patients and control group (p < 0.0001) and in COPD patients than in control group (p < 0.0001) (Figs. 1 and 2) (Table 1). Comparison of integrity index among the three populations (lung cancer, COPD, and controls) is shown in Fig. 3.
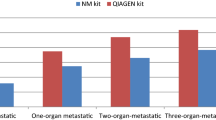
ALU247 was significantly higher in patients with metastasis (stage IV) than in early stages (stages I and II) (p = 0.04) or in advanced stage (stage III) (p = 0.01). In respect to histopathological type, adenocarcinoma patients showed significantly higher values of ALU247 and DNA integrity than other histopathological types (p = 0.04 and 0.02, respectively). No significant difference was found between different grades of lung cancer. Correlation analysis showed significant positive correlations between DNA integrity index and stage of tumour (p = 0.01) and tumour metastasis (p = 0.004) (Tables 2 and 3). DII in healthy smokers of the control group showed significant higher mean 0.28 ± 0.07 in comparison to the healthy nonsmokers in the same group 0.22 ± 0.06 (p = 0.01).
ROC curve analysis showed an AUC for ALU247 = 0.92 with total accuracy = 86.4% at a cut-off value of 26.1 ng/ml with sensitivity = 83%, specificity = 89%, positive predictive value (PPV) = 83.3%, and a negative predictive value (NPV) = 88.5 (p < 0.0001). For DNA integrity, the AUC was 0.91 with total accuracy of 85.6% at a cut-off value 0.44 ng/ml, with sensitivity = 90%, specificity = 83%, PPV = 78.1%, and NPV = 92.1 (p < 0.0001) (Fig. 4).
Discussion
This study aimed to evaluate the clinical utility of DII as a biomarker in NSCLC in comparison with COPD and controls.
Previous studies reported a significantly increased DII in different types of cancer indicating its value as a diagnostic marker. In the current study, we assessed the utility of DII as a diagnostic tool in lung cancer patients in comparison with COPD and control subjects and studied its potential correlation with tumour stage and metastasis. Our results demonstrated significantly higher integrity index in NSCLC patients compared to COPD patients and control subjects. These results are in agreement with previous results [28,29,30,31,32,33]. Moreover, significant higher values were observed in COPD patients compared to the control group. In accordance with the findings of [30] who reported significant differences in ALU115, ALU247 concentrations, and DII between COPD and control groups, which was attributed to inflammation contributing to increased cell death rates [34]. In contrast, Soliman et al. (2018) found insignificant differences in ALU115, ALU247, and DII between COPD and control groups [33].
According to TNM staging system, a significantly high ALU115, ALU247, and DII were detected among late-stage cancer patients (III & IV) and in cases with metastatic lesions in comparison with non-metastatic cases. Adenocarcinoma showed significantly higher values of all parameters compared to other histopathological types (squamous and large cell carcinoma). Findings are in line with similar studies which reported higher plasma concentration of cfDNA in late stages of tumour than in early stages [35, 36] and more elevation in metastatic than in non-metastatic cases [32, 33]. In contrast, other researches could not find any association between cfDNA concentration and tumour stage [37], metastasis [38], or histological type (adenocarcinoma or squamous cell carcinoma) [31].
Wang et al. (2003) declared DII clinical utility by proving significantly higher value in ovarian and gynaecological cancers [39]. Furthermore, studies in solid tumuors such as colorectal [18, 40, 41], breast [17, 42], head and neck [43], and prostate cancers [44] reported positive results for diagnostic and prognostic value of ALU repeats. That might be elucidated by vascular invasion occurring in malignant tumours that enhances DNA release into the circulation, hence enabling the dissemination of tumour cells [35].
Francaviglia et al. (2019) investigated lung cancer cfDNA analysis and reported the successful use of plasma ctDNA for identification of therapeutic targets, monitoring of therapy, and resistance to treatment [27], while Dziadziuszko et al. (2022) suggested the usefulness of plasma cfDNA concentration as a prognostic marker in advanced ALK + NSCLC [45].
To evaluate diagnostic validity of integrity index, ROC curve analysis demonstrated a cut-off value of 0.44 with total accuracy of 85.6%, sensitivity and specificity 90% and 83%, respectively, and PPV 78.1% and NPV 92.1. The median of DNA integrity in COPD cases in this study was 0.4 ng/ml (IQR = 0.3–0.5 ng/ml).
In a similar study on 60 NSCLC patients 40 COPD and 40 controls, Soliman et al. (2018) demonstrated a cut-off value of 0.48 ng/ml for DNA integrity but with lower sensitivity and specificity, 75% and 42.5%, respectively [33]. They also found that ALU247 had higher diagnostic accuracy 92.1%, with sensitivity and specificity of 96.7% and 88.7%, respectively, and PPV of 86.6% and NPV of 97.3%. Similarly, in a study on 50 NSCLC patients, 101 patients with chronic respiratory inflammation, and 40 healthy controls, Szpechcinski et al. (2015) found that the use of the quantitative cfDNA assay as a diagnostic biomarker to differentiate NSCLC from non-malignant inflammatory diseases and healthy individuals showed a highest accuracy achieved at a cut-off value of 42.80 ng/ml, with sensitivity of 90% and specificity of 80.5% and PPV of 85% and NPV of 87% [31].
Kamel et al. (2016) reported a significantly higher level of DII in plasma of breast cancer than patients with in benign breast lesions and healthy controls. They stated a sensitivity and specificity values of DII 85% and 100%, respectively, defining the clinical utility of ctDNA. Moreover, they described a correlation between DII and TNM staging suggesting that DII might be a promising diagnostic and prognostic biomarker of breast cancer [23].
In a previous study to check the accuracy, sensitivity, and specificity of using cfDNA as a screening tool in cancer patients against both benign and control groups, cfDNA represented a highly sensitive and specific marker, 100% and 75%, respectively, in comparison to traditional tumour markers [38].
In a recent study on 84 NSCLC patients, Ren et al. (2023) reported a significantly higher concentration of plasma cfDNA (ALU60, ALU115) in NSCLC patients (stage III/IV) than in healthy controls [46].
In contrast, other studies concluded that DII is not a useful clinical tool to detect malignancies because of its poor specificity and sensitivity [47, 48]. Discrepancies noticed among different studies might be related to the variation in selection of subjects, pre-analytical and analytical procedures, and to the characteristics and numbers of patient populations.
Despite the valuable implications of our results, this study has several limitations. First, the small sample size in addition to discrepancy of demographic characteristics (age/gender) and smoking behaviour between patients and control may introduce bias. Therefore, larger cohort studies with balanced demographics between NSCLC patients and controls are required in the future researches. Second, the study’s cross-sectional design limits its capacity to assess the prognostic value of cfDNA and DII over time. Third, our study lacks direct comparison with other established NSCLC biomarkers, hindering proper insights of cfDNA and DII’s significance. Fourth, we did not explore the potential influence of other factors such as comorbidities, medications, and environmental factors on cfDNA and DII levels. Finally, challenges in translating these findings into clinical practice necessitate further validation in diverse populations and clinical settings.
Conclusion
As liquid biopsies represent a potential, attractive, noninvasive alternative of routine surgical biopsies for diagnosis and prognosis of cancer, this study aimed to evaluate the clinical utility of DII as a biomarker in NSCLC in comparison with COPD and controls.
By detecting cfDNA concentrations in plasma samples and evaluating DII by means of ALU repeats, we suggest that DII could be a candidate biomarker in the early detection and screening for NSCLC. We also identified a prognostic role of this new emerging biomarker, being correlated with TNM and metastasis, highlighting its potential role in monitoring disease progression. We also identified a cut-off value for DNA integrity index in COPD patients for periodic follow-up and closer monitoring to help screening and early detection of lung cancer among COPD patients.
Availability of data and materials
All data supporting our findings can be found in the "Results" section in the main manuscript.
Abbreviations
- ALU:
-
Arthrobacter luteus
- cfDNA:
-
Circulating cell-free DNA
- COPD:
-
Chronic obstructive lung disease
- ctDNA:
-
Circulating tumour DNA
- DII:
-
DNA integrity index
- EDTA:
-
Ethylenediaminetetraacetic acid
- HRCT:
-
High-resolution computerized tomography
- IQR:
-
Interquartile range
- LCC:
-
Large cell carcinoma
- NCI:
-
National Cancer Institute
- NPV:
-
Negative predictive value
- NRC:
-
National Research Centre
- NSCLC:
-
Non-small cell lung cancer
- PPV:
-
Positive predictive value
- qPCR:
-
Quantitative real-time polymerase chain reaction
- SCC:
-
Squamous cell carcinoma
- SD:
-
Standard deviation
- TNM:
-
Tumour, nodes, and metastasis
- WHO:
-
World Health Organization
References
Ibrahim AS, Khaled HM, Mikhail NN, Baraka H, Kamel H. Cancer incidence in Egypt: results of the National Population-Based Cancer Registry Program. J Cancer Epidemiol. 2014;2014:437971.
WORLD HEALTH RANKINGS; Lung cancer in Egypt – World Life Expectancy,2022; https://www.worldlifeexpectancy.com› Egypt-lung-cancers
Mattox AK, Bettegowda C, Zhou S, Papadopoulos N, Kinzler KW, Vogelstein B. Applications of liquid biopsies for cancer. Sci Transl Med. 2019;11:eaay1984.
Xie F, Li P, Gong J, Tan H, Ma J. Urinary cell-free DNA as a prognostic marker for KRAS-positive advanced-stage NSCLC. Clin Transl Oncol. 2018;20:591–8.
Von Felden J, Garcia-Lezana T, Schulze K, Losic B, Villanueva A. Liquid biopsy in the clinical management of hepatocellular carcinoma. Gut. 2020;69:2025–34.
Roy D, Tiirikainen M. Diagnostic power of DNA methylation classifiers for early detection of cancer. Trends Cancer. 2020;6:78–81.
Zhou B, Xu K, Zheng X, Chen T, Wang J, Song Y, Shao Y, Zheng S. Application of exosomes as liquid biopsy in clinical diagnosis. Signal Transduct Target Ther. 2020;5:1–14.
Mattox AK, Bettegowda C, Zhou S, Papadopoulos N, Kinzler KW, Vogelstein B. Applications of liquid biopsies for cancer. Sci Transl Med. 2019;11:eaay1984.
Gao W, Huang T, Yuan H, Yang J, Jin Q, Jia C, Mao G, Zhao J. Highly sensitive detection and mutational analysis of lung cancer circulating tumor cells using integrated combined immunomagnetic beads with a droplet digital PCR chip. Talanta. 2018;185:229–36.
Guibert N, Delaunay M, Lusque A, Boubekeur N, Rouquette I, Clermont E, Mourlanette J, Gouin S, Dormoy I, Favre G. PD-L1 expression in circulating tumor cells of advanced non-small cell lung cancer patients treated with nivolumab. Lung Cancer. 2018;120:108–12.
Akamatsu H, Koh Y, Okamoto I, Fujimoto D, Bessho A, Azuma K, Morita S, Yamamoto N, Nakagawa K. Clinical significance of monitoring EGFR mutation in plasma using multiplexed digital PCR in EGFR mutated patients treated with afatinib (West Japan Oncology Group 8114LTR study). Lung Cancer. 2019;131:128–33.
Okajima W, Komatsu S, Ichikawa D, Miyamae M, Kawaguchi T, Hirajima S, Ohashi T, Imamura T, Kiuchi J, Arita T. Circulating microRNA profiles in plasma: identification of miR-224 as a novel diagnostic biomarker in hepatocellular carcinoma independent of hepatic function. Oncotarget. 2016;7:53820–36.
Zedan AH, Hansen TF, Assenholt J, Madsen JS, Osther PJS. Circulating miRNAs in localized/locally advanced prostate cancer patients after radical prostatectomy and radiotherapy. Prostate. 2018;79:425–32.
Avogbe PH, Manel A, Vian E, Durand G, Forey N, Voegele C, Zvereva M, Hosen I, Meziani S, De Tilly B. Urinary TERT promoter mutations as non-invasive biomarkers for the comprehensive detection of urothelial cancer. EBioMedicine. 2019;44:431–8.
Song T, Mao F, Shi L, Xu X, Wu Z, Zhou J, Xiao M. Urinary measurement of circulating tumor DNA for treatment monitoring and prognosis of metastatic colorectal cancer patients. Clin Chem Lab Med. 2018;57:268–75.
Garinet S, Laurent-Puig P, Blons H, Oudart J. Review current and futuremolecular testing in NSCLC, what can we expect from new sequencing technologies? J Clin Med. 2018;7:144.
Umetani N, Giuliano AE, Hiramatsu SH, Amersi F, Nakagawa T, Martino S, Hoon DS. Prediction of breast tumor progression by integrity of free circulating DNA in serum. J Clin Oncol. 2006;24(26):4270–6.
Umetani N, Kim J, Hiramatsu S, Reber HA, Hines OJ, Bilchik AJ, Hoon DS. Increased integrity of free circulating DNA in sera of patients with colorectal or periampullary cancer: direct quantitative PCR for ALU repeats. Clin Chem. 2006;52(6):1062–9.
Oliveira IBD. Hirata RDC;Circulating cell-free DNA as a biomarker in the diagnosis and prognosis of colorectal cancer. Br J Pharmaceutical Sciences. 2018;54:e17368.
Wang X, Shi XQ, Zeng PW, Mo FM, Chen ZH. Circulating cell free DNA as the diagnostic marker for colorectal cancer: a systematic review and meta-analysis. Oncotarget. 2018;9:24514–24.
El-Shazly SF, Eid MA, El-Sourogy HA, Attia GF, Ezzat SA. Evaluation of serum DNA integrity as a screening and prognostic tool in patients with hepatitis C virus-related hepatocellular carcinoma. Int J Biol Markers. 2010;25(2):79–86.
Hashad D, Sorour A, Ghazal A, Talaat I. Free circulating tumor DNA as a diagnostic marker for breast cancer. J Clin Lab Anal. 2012;26(6):467–72.
Kamel AM, Teama S, Fawzy A, El Deftar M. Plasma DNA integrity index as a potential molecular diagnostic marker for breast cancer. Tumour Biol. 2016;37:7565–72.
Ilie M, Hofman V, Long E, Bordone O, Selva E, Washetine K, Marquette CH, Hofman P. Current challenges for detection of circulating tumor cells and cell-free circulating nucleic acids, and their characterization in non-small cell lung carcinoma patients What is the best blood substrate for personalized medicine? Ann Transl Med. 2014;2(11):107.
Zhang Y, Zheng H, Zhan Y, Long M, Liu S, Lu J, Zang H, Fan S. Detection and application of circulating tumor cell and circulating tumor DNA in the non-small cell lung cancer. Am J Cancer Res. 2018;8(12):2377–86.
Chudasama DY, Aladag Z, Felicien MI, Hall M, Beeson J, Asadi N, Anikin VB. Prognostic value of the DNA integrity index in patients with malignant lung tumors. Oncotarget. 2018;9(30):21281–8.
Francaviglia I, Magliacane G, Lazzari C, Grassini G, Brunetto E, Cin ED, Girlando S, Medicina D, Smart CE, Bulotta A. Identification and monitoring of somatic mutations in circulating cell-free tumor DNA in lung cancer patients. Lung Cancer. 2019;134:225–32.
Szpechcinski A, Dancewicz M, Kopinski P, Kowalewski J, Chorostowska-Wynimko J. Real-time PCR quantification of plasma DNA in non-small cell lung cancer patients and healthy controls. Eur J Med Res. 2009;14(4):237–40.
van der Drift MA, Hol BE, Klaassen CH, Prinsen CF, van Aarssen YA, Donders R, van der Stappen JW, Dekhuijzen PN, van der Heijden HF, Thunnissen FB. Circulating DNA is a non-invasive prognostic factor for survival in non-small cell lung cancer. Lung Cancer. 2010;68(2):283–7.
Hao TB, Shi W, Shen XJ, Qi J, Wu XH, Wu Y, Tang YY, Ju SQ. Circulating cell-free DNA in serum as a biomarker for diagnosis and prognostic prediction of colorectal cancer. Br J Cancer. 2014;14 111(8):1482–9.
Szpechcinski A, Chorostowska-Wynimko J, Struniawski R, Kupis W, Rudzinski P, Langfort R, Puscinska E, Bielen P, Sliwinski P, Orlowski T. Cell-free DNA levels in plasma of patients with non-small-cell lung cancer and inflammatory lung disease. Br J Cancer. 2015;113(3):476–83.
Chudasama DY, Aladag Z, Felicien MI, Hall M, Beeson J, Asadi N, Gidron Y, Karteris E, Anikin VB. Prognostic value of the DNA integrity index in patients with malignant lung tumors. Oncotarget. 2018;9(30):21281–8.
Soliman SE, Alhanafy AM, Habib MSE, Hagag M, Ibrahem RAL. Serum circulating cell free DNA as potential diagnostic and prognostic biomarker in non-small cell lung cancer. Biochem Biophys Rep. 2018;15:45–51.
Holdenrieder S, Burges A, Reich O, Spelsberg FW, Stieber P. DNA integrity in plasma and serum of patients with malignant and benign diseases. Ann N Y Acad Sci. 2008;1137:162–70.
Sozzi G, Conte D, Leon M, Ciricione R, Roz L, Ratcliffe C, Roz E, Cirenei N, Bellomi M, Pelosi G, Pierotti MA, Pastorino U. Quantification of free circulating DNA as a diagnostic marker in lung cancer. J Clin Oncol. 2003;21(21):3902–8.
Gautschi O, Bigosch C, Huegli B, Jermann M, Marx A, Chassé E, Ratschiller D, Weder W, Joerger M, Betticher DC, Stahel RA, Ziegler A. Circulating deoxyribonucleic Acid as prognostic marker in non-small-cell lung cancer patients undergoing chemotherapy. J Clin Oncol. 2004;22(20):4157–64.
Yi Z, Liu B, Guan X, Ma F. Plasma cell-free DNA and survival in non-small-cell lung cancer: a meta-analysis. Mol Clin Oncol. 2017;7:167–72.
Zaher ER, Anwar MM, Kohail HM. Cell-free DNA concentration and integrity as a screening tool for cancer. Indian J Cancer. 2013;50(3):175–83.
Wang BG, Huang HY, Chen YC, Bristow RE, Kassauei K, Cheng CC, Roden R, Sokoll LJ, Chan DW, Shih IM. Increased plasma DNA integrity in cancer patients. Cancer Res. 2003;63:3966–8.
Salem R, Ahmed R, Shaheen K, Hassan H. DNA integrity index as a potential molecular biomarker in colorectal cancer. Egypt J Med Hum Genet. 2020;21:38.
Zhu F, Ma J, Ru D, Wu N, Zhang Y, Li H, Liu X, Li J, Zhang H, Xu Y, Zhao J, Tang H, Wang Y, Fu W. Plasma DNA integrity as a prognostic biomarker for colorectal cancer chemotherapy. J Oncol. 2021;26(2021):5569783.
Lehner J, Stötzer OJ, Fersching DM, Nagel D, Holdenrieder S. Plasma DNA integrity indicates response to neoadjuvant chemotherapy in patients with locally confined breast cancer. Int J Clin Pharmacol Ther. 2013;51:59–62.
Jiang WW, Zahurak M, Goldenberg D, Milman Y, Park HL, Westra WH, Koch W, Sidransky D, Califano J. Increased plasma DNA integrity index in head and neck cancer patients. Int J Cancer. 2006;119:2673–6.
Hanley R, Rieger-Christ KM, Canes D, Emara NR, Shuber AP, Boynton KA, Libertino JA, Summerhayes IC. DNA integrity assay: a plasma-based screening tool for the detection of prostate cancer. Clin Cancer Res. 2006;12:4569–74.
Dziadziuszko R, Peters S, Mok T, Camidge DR, Gadgeel SM, Ou SI, Konopa K, Noé J, Nowicka M, Bordogna W, Morcos PN, Smoljanovic V, Shaw AT. Circulating cell-free DNA as a prognostic biomarker in patients with advanced ALK+ non-small cell lung cancer in the global phase III ALEX trial. Clin Cancer Res. 2022;28(9):1800–8.
Ren S, Zeng G, Yi Y, Liu L, Tu H, Chai T, Hu L. Combinations of plasma cfDNA concentration, integrity, and tumor markers are promising biomarkers for the early diagnosis of non-small cell lung cancer. Heliyon. 2023;9(10):e20851. https://doi.org/10.1016/j.heliyon.2023.e20851. PMID:37860559;PMCID:PMC10582504.
Boddy JL, Gal S, Malone PR, Shaida N, Wainscoat JS, Harris AL. The role of cell-free DNA size distribution in the management of prostate cancer. Oncol Res. 2006;16:35–41.
Utomo WK, Janmaat VT, Verhaar AP, Cros J, Lévy P, Ruszniewski P, den Berg MS, Jenster G, Bruno MJ, Braat H, Fuhler GM, Peppelenbosch MP. DNA integrity as biomarker in pancreatic cyst fluid. Am J Cancer Res. 2016;6:1837–41.
Acknowledgements
Center of Excellence, National Research Center, Cairo, Egypt.
Funding
This work was funded by the National Research Centre (NRC), Cairo, Egypt.
Author information
Authors and Affiliations
Contributions
NE and DE prepared the study conception and design. Funding was obtained by NE. Material preparation and data collection made by DE, MH, ASh, SH, AG, GL, and MS. Medical analysis was performed by MS. Laboratory investigations and analysis were carried out by DE, MH, and AR. Statistical analysis was done by AM. The first draft of the manuscript was written by NE and revised by DE and MH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was permitted by the Ethics Committee of the National Research Centre, registration number 19–234. A written informed consent was obtained from all subjects after being fully aware of the nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ezzeldin, N., El-Lebedy, D., Hassan, M. et al. Evaluating circulating cell-free DNA and DNA integrity index as biomarkers in non-small cell lung cancer. J Egypt Natl Canc Inst 36, 21 (2024). https://doi.org/10.1186/s43046-024-00219-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43046-024-00219-1