Abstract
Background
Clozapine is a second-generation antipsychotic which is known to have superior efficacy as compared to other antipsychotics. It is particularly used in treatment-resistant schizophrenia (10–30%). However, its use is limited due to the serious side effect of inducing seizures which can occur at all doses. The purpose of our study was to analyse patients taking clozapine for any electroencephalographic (EEG) abnormalities. We undertook a cross-sectional study on 107 patients with a different diagnosis taking clozapine who visited the outdoor treatment facility of a tertiary care psychiatric diseases hospital in Kashmir. A 32-channel digital EEG was obtained and evaluated visually for any abnormalities in these patients. The data was tabulated and analysed using SPSS 23.0.
Results
EEG abnormalities were reported in 60.75% of patients receiving clozapine out of which slow waves and epileptiform activities were present in 48.60% and 30.84% of patients, respectively. Background slowing was often in the delta and theta ranges. Our study showed that there was a statistically significant relationship between the dose of clozapine and EEG abnormalities. Clinical seizure occurred in only one patient receiving clozapine 450 mg/day and was a smoker who had recently stopped smoking.
Conclusions
EEG abnormalities occur frequently in clozapine-treated patients specifically those taking higher doses of clozapine. This calls for utilising EEG as a useful clinical investigation in these patients along with clinical monitoring of seizures especially in those taking higher doses of clozapine in order to hint towards early signs of clozapine toxicity. Caution needs to be taken in patients who are smokers and show a pattern of change in their smoking habits. Moreover, EEG abnormalities though frequently associated with clozapine are not reliable predictors of seizures. Therefore, anticonvulsants may not be routinely indicated in patients on clozapine even in the presence of epileptiform discharges.
Similar content being viewed by others
Background
Clozapine is a second-generation antipsychotic which is chemically a dibenzodiazepine derivative [1, 2]. It exerts its antipsychotic effects by blocking dopamine receptors D1 and D4 as well as serotonin receptors 5-HT1A and 5-HT2. When compared to other antipsychotics, it has a unique profile in treatment-resistant schizophrenia due to its multiple receptor occupancy which also renders it less likely to cause extrapyramidal side effects (EPS) including tardive dyskinesia than other antipsychotics [3]. It is regarded as a disease-modifying agent and is widely prescribed despite causing some serious adverse effects such as seizures [4, 5] and agranulocytosis [6]. Research has pointed towards the occurrence of seizures more than agranulocytosis [7] with the incidence of clozapine-induced seizures ranging from 1.3% [8] to 2.8% [9]. There are many retrospective studies which depict a wide range of EEG abnormalities associated with clozapine treatment ranging from 53% [10] and 59% [11] to 74% [12]. Clozapine is known to be the leading cause of EEG slowing and epileptiform discharges among all antipsychotics [13]. Studies done on clozapine-induced seizures reported seizures to occur at all dose ranges [14] including very low doses of clozapine [15] during the titration phase and at high doses during the maintenance phase of clozapine [8]. This may be attributed to the variation in clozapine plasma level at a given dose of clozapine owing to its complex metabolism [16]. There is a dearth of research regarding the pattern of EEG abnormalities in clozapine-treated patients especially in Kashmir. Therefore, this study aimed at exploring the pattern of EEG abnormalities in patients on clozapine and the clinical utility of EEG monitoring in these patients.
Methods
We did a cross-sectional hospital-based study on 107 patients with a different diagnosis who showed treatment resistance and visited the outdoor treatment facility of a tertiary care psychiatric diseases hospital in Kashmir. Patients were selected through a purposive sampling technique who were receiving clozapine for > 1 month. Those who had a history of seizures prior to the introduction of clozapine, a history of significant head trauma, or a history of undergoing electroconvulsive therapy were excluded from the study. EEG was done after obtaining written informed consent from the patients or their caretakers. EEG recordings were taken using a 32-channel digital EEG machine. EEG recordings were taken during arousal, eyes opened and eye closed, hyperventilation and photic stimulation states. The EEG recordings were analysed by a trained EEG specialist, and EEG abnormalities, including slow wave details, types, and epileptiform activity details were characterised separately. The study was approved by the institutional ethics committee.
Statistical analysis
The data was analysed using the SPSS software version 23.0 (SPSS Inc., Chicago, IL, USA). Two groups were made based on the presence and absence of EEG abnormality. Pearson’s chi-square and Student’s independent t tests were used to compare the group variables. A p-value of less than 0.05 was considered statistically significant. All p-values were two-tailed. A logistic analysis was performed to identify any predictors of EEG abnormalities.
Results
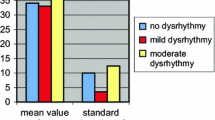
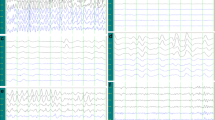
Out of the study sample, 78 were males (72.90%) and 29 were females (27.10%). The mean age was 38.38 ± 7.16 years while the mean duration of illness was 9.63 ± 5.07 years. The mean clozapine dose was 347.43 ± 71.70 mg/day ranging from 200 to 550 mg/day, and the mean duration of clozapine intake was 13.84 ± 6.71 weeks. Out of the study population, 81 (75.7%) had a diagnosis of schizophrenia while the rest were diagnosed with schizoaffective disorder (21, 19.6%) and bipolar disorder (5, 4.67%). Sixty-eight (63.6%) out of 107 patients were smokers while only 39 (36.4%) were non-smokers. All the patients were right-handed. None had a history of childhood epilepsy or other organic causes of seizures like head injury. EEG abnormalities were found in 65 (60.75%) of the study population. EEG abnormalities consisted of predominantly slow wave discharges (48.60%) while epileptiform activity was found in 30.84% of the study sample. The details of the EEG abnormalities are tabulated in Table 1. Only one patient diagnosed with schizophrenia developed clinical seizures of tonic-clonic variety at a clozapine dose of 450 mg/day.
Patients with EEG abnormalities had a higher mean dose of clozapine (385 ± 7.86) than patients without EEG abnormalities (289.29 ± 5.60) which was statistically significant (p-value < 0.01). This study found no significant correlation between the duration of clozapine treatment and EEG abnormalities despite a higher mean duration of clozapine treatment (18.18 ± 0.80 weeks) in the group with EEG abnormalities. The majority of the study sample with EEG abnormalities were non-smokers (66.67%) as compared to the majority of smokers (42.65%) in the group without EEG abnormalities; however, this was not found to be statistically significant.
Seizures which were generalised and had tonic-clonic presentation occurred in only one patient in our study who was diagnosed with schizophrenia and was taking clozapine 450 mg daily. The patient was a smoker who had recently stopped smoking and was not taking any other medication.
No significant difference was found in the two groups of EEG abnormalities and age, gender, duration of illness, and diagnosis (Table 2). Logistic regression analysis found a dose of clozapine to be a significant predictor of EEG abnormalities in patients receiving clozapine (Table 3).
Discussion
In our study, EEG abnormalities were found in more than half (60.75%) of the study subjects with non-specific generalised slowing consisting of theta waves predominantly being the most common. This is in line with many other previous studies [13, 17, 18]
Most of the previous studies found non-specific slowing to be the most common EEG abnormality in clozapine-treated patients [13, 19, 20].
Gunther et al. found EEG abnormality occurring in 61.5% of 283 patients with non-specific slowing being the most frequent abnormality occurring in 47% of the abnormal EEGs [13]. This was similar to our study where non-specific slow wave activity occurred in 48.60% of the study subjects while epileptiform activity occurred in only 30.84%.
A significant positive relationship was found between the mean daily clozapine dose and EEG abnormality in our study. A similar result was found in a number of other previous studies [13, 18]. A review study conducted by Verma et al. in 2011 further reinforces our findings in their regression model [21]. Another study by Neufeld et al. in 1996 in psychotic parkinsonism patients taking clozapine in the range of 6.25–75 mg concluded that EEG abnormalities occurred in low-dose clozapine as well [18]. However, our study sample consisted of patients taking at least 200 mg of clozapine per day. Therefore, such an association could not be ruled out. There is a scarcity of large-scale data regarding the correlation of smoking with EEG abnormalities in patients receiving clozapine. However, a few case studies speak of smoking and occurrence of seizures in patients on clozapine [22, 23]. Our study found a positive correlation between smoking and EEG abnormalities; however, this was not found to be statistically significant. One reason for this may be that the polycyclic aromatic hydrocarbons contained in cigarette smoke are an inducer of CYP1A2 enzymes which accelerates the metabolism of clozapine. This results in the requirement of higher doses of clozapine in smokers compared to non-smokers and hence higher prevalence of EEG abnormalities in them.
There is conflicting evidence regarding the association of clozapine dose and occurrence of seizures. A review paper by Verma et al. did not find any significant correlation between clozapine dose and seizures. Most of the case studies depicted an increasing risk of seizures with increasing doses of clozapine especially a dosage of more than 600 mg a day [5, 7, 24, 25].
However, surprisingly, there are case reports of seizures in low-dose clozapine patients as well [26]. The contrasting results can be explained by the variations in the clozapine serum levels for a given dose within and among individuals due to its complex metabolism [16, 27].
In our study, seizure occurred in one patient diagnosed with schizophrenia receiving a clozapine dose of 450 mg a day for a duration of 25 weeks. The patient developed sudden generalised tonic-clonic seizures (GTCS) which is supported by various existing data on clozapine-induced seizures reporting GTCS as the most common type of seizure induced by clozapine [28]. The patient had both slow waves and epileptiform discharges on EEG. The patient was a smoker who had recently stopped smoking which could explain the sudden increase in the serum levels of clozapine leading to the seizure. However, we could not measure the serum clozapine levels in patients which becomes a limitation of our study. Hence, commenting on this aspect is beyond the scope of this study. Moreover, the patient was not on any other concurrent medication but was added on divalproex sodium after the clinical fit. There is weak evidence in the form of few case reports depicting the increased risk of seizures at clozapine levels greater than 1300 μg/L. [21] In addition to this, the failure to get the pre-treatment EEG becomes another shortcoming of this study. Nevertheless, EEG abnormalities do not predict the occurrence of seizures as was seen in our study [18].
Keeping in mind the suggestions of various authors, it becomes prudent to monitor EEG changes along with serum levels of clozapine in these patients specifically those receiving higher doses of clozapine so as to watch for early signs of toxicity and hence of seizures [17, 20, 27].
Regarding the use of anticonvulsants as prophylaxis in patients on clozapine without clinical seizures, there is insufficient evidence except for some reports that favour the use of such medications after the emergence of clear epileptiform discharges or plasma level of more than 500 μg/L of clozapine [21].
Therefore, we do not suggest the routine use of anticonvulsants even in the presence of epileptiform discharges in the absence of other risk factors such as pre-existing epilepsy and a history of a significant head trauma. A more reasonable approach would be to look for the clinical appearance of seizures especially in higher doses [17].
Our study presents with few limitations like it was a cross-sectional study so we could not infer any causal relationship between clozapine and EEG abnormalities. Also, we could not measure the serum clozapine levels and the associated EEG abnormalities. Furthermore, our study cannot rule out the role of sedative effects of drugs and psychiatric illness as it was one of the limitations of the study. Additional large-scale studies are required to establish with certainty the relationship between clozapine and seizures, sedative effects of drugs, and psychiatric illness.
Conclusions
EEG abnormalities occur frequently in clozapine-treated patients specifically those taking higher doses of clozapine. This calls for utilising EEG as a useful clinical investigation in these patients along with clinical monitoring of seizures especially in those taking higher doses of clozapine in order to hint towards early signs of clozapine toxicity. Caution needs to be taken in patients who are smokers and show a pattern of change in their smoking habits. Moreover, EEG abnormalities though frequently associated with clozapine are not reliable predictors of seizures. Therefore, anticonvulsants may not be routinely indicated in patients on clozapine even in the presence of epileptiform discharges.
Availability of data and materials
The dataset generated and/or analysed during the current study is available from the corresponding author upon reasonable request.
Abbreviations
- EEG:
-
Electroencephalogram
- SPSS:
-
Statistical Package for Social Sciences
- EPS:
-
Extrapyramidal side effects
- SD:
-
Standard deviation
- GTCS:
-
Generalised tonic-clonic seizures
References
Coward DM, Imperato A, Urwyler S, White TG (1989) Biochemical and behavioural properties of clozapine. Psychopharmacology 99(Suppl):S6–S12
van Tol HH, Bunzow JR, Guan HC, Sunahara RK, Seeman P, Niznik HB et al (1991) Cloning of the gene for a human dopamine D4 receptor with high affinity for the antipsychotic clozapine. Nature 350:610–614
Tamminga CA, Thaker GK, Moran M, Kakigi T, Gao XM (1994) Clozapine in tardive dyskinesia: observations from human and animal model studies. J Clin Psychiatry 55(Suppl B):102–106
Devinsky O, Pacia SV (1994) Seizures during clozapine therapy. J Clin Psychiatry 55(Suppl B):153–156
Haller E, Binder RL (1990) Clozapine and seizures. Am J Psychiatry 147:1069–1071
Alvir JM, Lieberman JA, Safferman AZ, Schwimmer JL, Schaaf JA (1993) Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med 329:162–167
Karper LP, Salloway SP, Seibyl JP, Krystal JH (1992) Prolonged postictal encephalopathy in two patients with clozapine-induced seizures. J Neuropsychiatr Clin Neurosci 4(4):454–457
Pacia SV, Devinsky O (1994) Clozapine-related seizures: experience with 5,629 patients. Neurology 44:2247–2249
Devinsky O, Honigfeld G, Patin J (1991) Clozapine-related seizures. Neurology 41:369–371
Günther W, Baghai T, Naber D, Spatz R, Hippius H (1993) EEG alterations and seizures during treatment with clozapine. Pharmacopsychiatry. 26(03):69–74
Spatz R, Lorenzi E, Kugler J, Rüther E (1978) The incidence of abnormal EEG patterns with clozapine therapy. Arzneimittelforschung. 28:1499–1500
Welch J, Manschreck T, Redmond D (1994) Clozapine-induced seizures and EEG changes. J Neuropsychiatr Clin Neurosci 6:250–256
Jackson A, Seneviratne U (2019) EEG changes in patients on antipsychotic therapy: a systematic review. Epilepsy Behav 95:1–9
Wilson WH, Claussen AM (1994) Seizures associated with clozapine treatment in a state hospital. J Clin Psychiatry 55(5):184–188
Thomas P, Goudemand M (1992) Seizure with low doses of clozapine. Am J Psychiatry 149:138–139
Haring C, Neudorfer C, Schwitzer J, Hummer M, Saria A, Hinterhuber H et al (1994) EEG alterations in patients treated with clozapine in relation to plasma levels. Psychopharmacology 114:97–100
Goyal N, Praharaj SK, Desarkar P, Nizamie H (2011) Electroencephalographic abnormalities in clozapine-treated patients: a cross-sectional study. Psychiatry Investig 8(4):372
Treves IA, Neufeld MY (1996) EEG abnormalities in clozapine-treated schizophrenic patients. Eur Neuropsychopharmacol 6(2):93–94
Malow BA, Reese KB, Sato S, Bogard PJ, Malhotra AK, Su TP, Pickar D (1994) Spectrum of EEG abnormalities during clozapine treatment. Electroencephalogr Clin Neurophysiol 91(3):205–211
Freudenreich O, Weiner RD, McEvoy JP (1997) Clozapine-induced electroencephalogram changes as a function of clozapine serum levels. Biol Psychiatry 42(2):132–137
Varma S, Bishara D, Besag FM, Taylor D (2011) Clozapine-related EEG changes and seizures: dose and plasma-level relationships. Ther Adv Psychopharmacol 1(2):47–66
Bolu A, Akarsu S, Pan E, Aydemir E, Oznur T (2017) Low-dose clozapine-induced seizure: a case report. Clin Psychopharmacol Neurosci 15(2):190
Chochol MD, Kataria L, O’Rourke MC, Lamotte G (2019) Clozapine-associated myoclonus and stuttering secondary to smoking cessation and drug interaction: a case report. J Clin Psychopharmacol 39(3):275–277
Baker RW, Conley RR (1991) Seizures during clozapine therapy. Am J Psychiatry 148:1265–1266
Simpson GM, Cooper TA (1978) Clozapine plasma levels and convulsions. Am J Psychiatry 135:99–100
Borah AJ, Kalita A, Dutta SK (2019) Clozapine-induced seizure. Indian J Pharm 51(6):410
Greenwood-Smith C, Lubman DI, Castle DJ (2003) Serum clozapine levels: a review of their clinical utility. J Psychopharmacol 17:234–238
Wong J, Delva N (2007) Clozapine-induced seizures: recognition and treatment. Can J Psychiatry 52(7):457–463
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SA, MR, and MM participated in formulating the idea and objectives of the research and developing a research plan and participated in collecting research data. SA and MR participated in presenting the scientific background of the research. SA, MR, and MM participated in scheduling the data, presenting the results, discussing, and matching the results with what was published globally in the field of research. All authors reviewed the manuscript and put it in its final form. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study proposal was approved by the institutional ethical committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roub, M., Dar, M.M. & Dar, S.A. Prevalence and pattern of electroencephalographic changes associated with clozapine treatment: a cross-sectional study. Middle East Curr Psychiatry 30, 37 (2023). https://doi.org/10.1186/s43045-023-00311-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00311-7