Abstract
The COVID-19 pandemic and its social restrictions have affected mental health globally. This systematic review aims to analyze the psychological responses of the general population and its related sociodemographic risk factors, excluding the most vulnerable groups (e.g., healthcare workers, COVID-19 patients and survivors, pregnant women, people with chronic diseases or preexisting psychiatric disorders). A reproducible search from June 2020 to February 2021 was conducted on PubMed and Google Scholar, following the PRISMA guidelines. Papers that (1) considered the most at-risk populations, (2) did not report sociodemographic data, and (3) did not use validated scales were excluded from our analysis. Non-English papers and review articles were also excluded. Of 1116 papers identified, 25 were included for this review (n = 162,465). The main risk factors associated with the emergence of depression, anxiety, sleep disorders, post-traumatic stress disorder, and obsessive compulsive disorder were: female gender, younger and later age, high level of education, Latino origin, free marital status, living quarantine in a house with no outdoor, negative coping strategies, close proximity to positive cases, high concern about contracting COVID-19 and living in a most affected area. High income, physical activity, resilience, family support, and a high level of knowledge about COVID-19, seems to be protective factors against the onset of psychological symptoms. In a general population, COVID-19 restrictions are linked to risk factors for psychological disorders caused by gender and sociodemographic conditions. In this regard governments should pay more attention to the public’s mental health and its risk and protective factors.
Similar content being viewed by others
Background
On March 11, 2020, the World Health Organization declared that the severe acute respiratory syndrome coronavirus (SARS-CoV2) outbreak in Wuhan, could be considered a global pandemic, named COVID-19 (coronavirus disease 2019) [1]. This new pandemic necessitated adapting immediately to a completely new reality, in which, for the good of all, it was essential to sacrifice some personal freedoms by isolating at home and maintaining social distance. The restrictions adopted by the governments of different countries, though they achieved a containment of infection in the first phase (World Health Organization, 2020), also affected people’s psychological well-being, causing emotional distress, anxiety, insomnia, depression, feeling of isolation, loneliness, boredom, and fear of being infected and infecting loved ones [2,3,4,5,6,7]. These negative reactions might have been increased by the growing number of new cases, the first deaths, and the extensive media coverage [8] that often deviates from medical and evidence-based sources, creating misinformation and alarmism [9].
Some population groups, e.g., healthcare workers, COVID-19 patients and survivors, pregnant women, people with chronic diseases or preexisting psychiatric disorder seem to be more vulnerable to the psychological effects of the pandemic [10, 11]. Most healthcare providers, exposed at the front lines in the fight against the virus [1], suffer from several disturbances such as depression (50.4%), anxiety (44.6%), insomnia (34%), and stress (71.5%) [12, 13]. In a study conducted in Wuhan by Zhu et al., the female health care workers or providers working with infected patients in emergency, intensive care or respiratory care, had increased risk of depression, anxiety, and stress [14]. They may have been particularly vulnerable due to close proximity to infected patients, long working hours, concerns about infecting loved ones, limited protective equipment, and involvement in emotional and ethical decisions [15, 16].
A large body of literature is available on the psychological outcomes in the most at-risk population; however, there are fewer studies about the psychological responses in the general population [6, 7, 17, 18]. The aim of this review is to analyze the role of sociodemographic variables in the appearance of psychological disorders in the general population during the pandemic. In particular, we analyzed the possible influence of sociodemographic variables, with special emphasis of gender (but not exclusively), on the onset of psychological disorders, such as depression, anxiety, sleep disorders, post-traumatic stress disorder (PTSD) stress and obsessive compulsive disorder (OCD) in the general population during the COVID-19 pandemic.
Methods
Methods and results were developed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method [19]
Search strategy
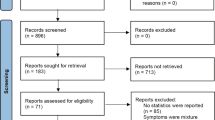
A systematic search using the PRISMA methodology was conducted from December 2020 to February 2021 on the PubMed platform. In the meantime, a manual search was performed on Google Scholar with the aim of identifying additional relevant studies (Fig. 1). The terms used were COVID-19 pandemic, mental health, psychological health, psychiatric disorders, depression, anxiety, sleep disorders, post-traumatic stress disorder, stress, obsessive compulsive disorder, gender-related, and social-demographic factors.
Study selection and inclusion criteria
An initial selection was conducted by Titles and Abstracts. The second selection was made from full-text following the eligibility criteria. The inclusion criteria applied to the selected studies were (1) assessment of the mental health in the general population during the COVID-19 pandemic, (2) evaluation of related risk factors, (3) consideration of gender differences in the sample, and (4) outcomes using standardized and validated scales. Studies were not considered if they were not written in English, and if the sample examined included (1) COVID-19 patients or COVID-19 survivors, (2) subcategories of the population at high risk such as health care workers and pregnant women, and (3) subjects with histories of chronic illness or psychiatric diseases. Moreover, guides, reviews, and articles that did not contain sociodemographic data were not considered.
Data extraction
In the preliminary analysis, the data extracted from the selected studies included (1) journal and author, (2) date of publication, (3) where the study was conducted, (4) study design, (5) period of administration, (6) sample size and characteristics, (7) disorders considered and diagnostic criteria, and (8) instruments/scales used.
Subsequently, a detailed analysis of the sociodemographic risk (or protective) factors related to the appearance of psychological disorders was carried out. More specifically, the risk and protective factors taken into account were (1) gender, (2) age, (3) level of education, (4) employment status, (5) ethnicity, (6) income, (7) region of origin, (8) marital status, (9) housing status, (10) relatives belonging to specific health categories, (11) frequency of physical exercise, (12) location of confinement/quarantine, (13) COVID-stressors (such as close contact with COVID patients, fear, concern about infection, knowledge of infected people, time spent researching COVID news, less knowledge about the virus, living in a high risk zone), and (14) psychological variables (i.e., coping strategy, resilience, tolerance of distress, social support).
Results
Research results
Globally, the identified publications were 1116, of which 139 were discarded as duplicates and 149 were excluded by screening titles and abstracts, leaving 961 full-text articles for eligibility. According to the exclusion criteria, 936 articles were discarded because they included (1) subgroups of the population at risk such as health care workers and pregnant women (n. 358); (2) COVID-19 or recovered patients (n. 107); (3) people with chronic diseases or histories of psychiatric illnesses (n. 237). Papers not in English (n. 9), articles with no sociodemographic information (n. 27), reviews, guides, or essays (n. 195) and articles with not validated assessment tools (n.3) were also excluded. After the selection process, 25 articles satisfied the inclusion criteria.
Study characteristics
The main characteristics of the studies are summarized in Table 1. The number of subjects included in the studies ranged from 103 to 52,730, with a total of 162,465 participants (105,546 females, 56,762 males and 102 “others”). The range of the sample age varied from 6 to 60 years old. All works were cross-sectional studies, and the method used for sampling was “snowball sampling.” With regard to country, the studies were carried out in China (n. 10); the USA (n. 4); Italy (n. 2); Poland (n. 2); Greece (n. 1); Australia (n. 1); Lebanon (n. 1); Bangladesh (n. 1); Canada (n. 1), and Iran (n.1). Finally, one study was conducted worldwide (Australia, China, Ecuador, Iran, Italy, Norway, and the USA). Nine studies specifically discussed the psychological outcome of anxiety and depression, three the sleep disorders and three the correlation between anxiety, depression, and sleep disorders. Seven articles analyzed symptoms related to PTSD (among these articles, three also referred to symptoms related to depression, anxiety, and stress, and one also evaluated psychological distress). Three articles discussed the OCD symptoms.
Sociodemographic risk and protective factors
A variety of sociodemographic factors have been analyzed to identify risk or protective factors related to the appearance of the disorders were taken into account. The data collected are shown below.
Risk and protective factors for anxiety and depression
Depression is a very common disorder in the general population, in both physiological and specific pathological conditions, and results in physical and cognitive changes that affect human functioning [54, 55]. Depression is the most frequently identified disorder during the pandemic, often in comorbidity with other symptoms such as generalized anxiety or sleep disorders [56]. Specifically, depressive symptoms were evaluated in 9 out of the 25 studies. Three studies were conducted in China, [21, 25] (Zhou, Zhang, et al., 2020) two in the USA [23, 28], one in Poland [27], Australia [26], Bangladesh [22], and Lebanon [24]. Data were collected from March to May 2020. The depressive symptoms have also been evaluated in association with other psychological disorders, more specifically with: sleep disorders [29, 30] (Zhou, Wang, et al., 2020) and PTSD [37, 39, 40].
Gender
A strong association between gender and depressive symptoms has been observed by using both the Birleson Depression Self-Rating Scale for Children (DSRS-C) [21, 57] and the Center for Epidemiological Studies-Depression Scale (CES-D) [28, 46]. In particular, female gender is the main risk factor for the development of depressive symptoms [58]. Using the Patient Health Questionnaire-9 (PHQ-9 scale) [51], depressive symptoms were much less reported in males than in females [23, 25, 26, 40] (Zhou, Zhang, et al., 2020). By using other scales such as the Depression, Anxiety, and Stress Scale-21 items (DASS-21) [47], or the Beck’s Depression Inventory scale (BDI) [45], these results were also confirmed [27, 29, 30]. In contrast, Islam et al. observed higher prevalence of depressive symptoms in male students as compared to females [22]. Comorbid with anxiety symptoms was specifically evaluated in eight studies, three of which were conducted in China [21, 25] (Zhou, Zhang, et al., 2020) one in Bangladesh [22], USA [23], Lebanon [24], Australia [26], and Poland [27]. Data were collected from March 2020 to May 2020. Furthermore, in two studies, these symptoms were evaluated in association with sleep disorders. The most frequently used scale to quantify generalized anxiety was the Generalized Anxiety Disorder 7 scale (GAD-7) [48]. The results were highly consistent and showed the association of anxiety symptoms with female gender [23, 25, 26] (Zhou, Zhang, et al., 2020). However, Islam et al., although the same scale was used, reported a large prevalence of anxiety in male students [22]. The other scales used, such as the Screen for Child Anxiety-Related Disorders scale (SCARED) [53, 59] and DASS-21 [27] confirmed the role of female gender on the emergence of symptoms related to anxiety. The State-Trait Anxiety Inventory scale (STAI) [60] was used to assay both the State anxiety (which reflects transient anxiety) and the Trait anxiety (which assesses an individual’s predisposition to react with anxiety to any stressful event). By using this scale, the state anxiety of women showed higher values as compared to men. Finally, Passavanti et al., through the subscale Anxiety of DASS-21, did not observe any gender difference [40].
Age
Adolescents are one of the groups most at-risk. In fact, the pandemic has produced dramatic changes in their lifestyles. Younger age seems to be a risk factor for the development of symptoms of anxiety and depression. Chen et al. showed higher levels of anxiety (23.50%) and depression (21.15%) in the category from 13 to 15 years [21]. In Islam et al., the category from 21 to 24 years was the most affected by depression (66.07%) and anxiety (66.58%) [22]. Rudenstine et al. highlighted that the group between 18 and 39 years old showed higher levels of anxiety (43.0%) and depression (52.5%) [23]. Tang et al. [39] confirmed that the age range with the highest PHQ-9 scores was 18–30 [39].
Education
Educational level is an influencing factor in the development of anxiety and depression symptoms. According to Zhou et al., the prevalence of anxiety and depression was higher in the more educated population [13]. In Rudenstine et al., more severe symptoms of depression were recorded in the “high school diploma” category, and more severe symptoms of anxiety were recorded in the “college” category [23]. Tang et al. confirmed that a high degree of education is considered a risk factor for the emergence of depressive symptoms [39].
Ethnicity
Rudenstine et al. reported higher rates of anxiety and depression in people of Latino origin [23]. In Fitzpatrick et al., the population most affected by depressive symptoms was observed in the people of Hispanic origin [28].
Marital status
The Rudestine study showed higher levels of anxiety (42.6%) and depression (53.4%) in the category of “never married” [23], also confirmed by Fitzpatrick et al. [28].
Living area
Regarding living area, the data are inconsistent. According to Zhou et al. depression and anxiety seem to be more common in the people coming from rural areas (47.5% and 40.4%, respectively) as compared to that from urban area (37.7% and 32.5%, respectively) [25]. In contrast, Islam et al. described a higher prevalence in the sample coming from the urban area (depression 65.05%; anxiety 62.21%) [22].
Housing status
For the housing status variable, the results are also inconsistent. Islam et al. indicate that the subjects that live in the family showed significantly higher values of anxiety (96.40%), and depression (96.93%) than those that lives alone or away from the family [22], while according to Hammarberg et al., living in the family seems to be a protective factor [26].
Physical activity
The most important protective factor for the consequences of the outbreak was the physical exercise [61,62,63,64]. Indeed subjects that did not practice physical activity had higher rates of depression and anxiety compared to those that practiced regular physical activity during the pandemic period [21, 22].
Income
High income seems to be a protective factor regarding the onset of the depressive and/or anxiety symptoms [26]. This observation is also confirmed in Passavanti et al., which showed that higher level of depression was associated with low income [40]. Rudenstine et al. reported that belonging to a low–medium-income group increases the probability that depression and anxiety will arise [23].
COVID-stressors
High level of knowledge regarding COVID-19 prevention and control measures seems to be an important protective factor against the onset of symptoms related to anxiety and depression [25]. Close proximity to confirmed cases in the community [21], high levels of COVID-stressor presence [23], high concern about contracting the virus [26, 37], extreme fear, and infected acquaintances [39] were all considered risk factors closely related to the onset of anxiety and depression.
Risk and protective factors for sleep disorders
Sleep disorders were evaluated in six of the 25 studies included in this review. Two studies were conducted in China [7] (Zhou, Wang, et al., 2020), one in Poland [29], USA [30], Greece [31], and Italy [34]. Data were collected from February to May 2020.
Gender
Tang et al. showed that during the pandemic, sleeping less than 6 h a day is one of the risk factors closely related to the emergence of anxiety and depression [39]. Insomnia Severity Index (ISI) [65] scores were closely related to high scores of anxiety in women [30]. Voitsidis et al. [31], by using the Athen Insomnia Scale (AIS) [44] (the Greek version of the ISI scale) also underlined significantly higher scores in women. Similarly, Zhou et al. (Zhou, Wang, et al., 2020) and Barrea et al. [34] by using the Pittsburgh Sleep Quality Index (PSQI) [52], showed that the prevalence of insomnia symptoms was lower in males than in females. Wang et al. [33] using the same scale, also confirmed this result. Zhou et al. (Zhou, Wang, et al., 2020) using the PHQ-9 and GAD-7 scales to measure depression and anxiety respectively, observed that students who showed depressive or anxiety symptoms, also exhibited symptoms related to insomnia. Bigalke et al., by using the PSQI scale, reported that 66% of the population was classified as “poor sleepers,” but no correlation with the gender was found [30].
Age-related factor
In the Wang et al. study, participants over 50 years old showed higher values at the PSQI scale [33].
Housing area
For the housing area factor, the results are homogeneous. Voitsidis et al. and Zhou et al. collected data showing that living in urban areas was a risk factor for the appearance of symptoms related to insomnia, while living in the rural places was a protective factor [31] (Zhou, Wang, et al., 2020).
Physical activity
Physical exercise is also a protective factor for the onset of sleep disorders. In the study by Wang et al., the category that had maintained a frequency of sports activity of 3 or more times weekly during quarantine showed lower scores at PSQI scale [56], than those who exercised less or not at all [33].
COVID-stressors
High level of knowledge about COVID-19 has been proposed as a protective factor (Zhou, Wang, et al., 2020) for sleep disorders. Similarly, an optimistic outlook with the future vision about COVID-19 was associated with a lower rate of insomnia symptoms. In contrast, excessive worry about the current situation, specifically related to “perceived COVID-19 death” and “treatment difficulty,” was a risk factor for the onset of insomnia symptoms [33].
Risk and protective factors for post-traumatic stress disorder and stress
Post-traumatic stress disorder was seen in 7 out of the 25 studies. Four studies were conducted in China [35, 36, 39, 66], one in the USA [37] and Italy [38]. One research on PTSD and stress symptoms was conducted worldwide, including Australia, China, Ecuador, Iran, Italy, Norway, and the USA [40]. Data were collected in the period between January and May 2020.
Gender
The gender differences for PTSD’s symptoms were not homogeneous. In the research conducted by Zhang et al., the mean scores on the Impact of Event Scale (IES) [49] between males and females were not significantly different [66]. Also, in the post-traumatic stress disorder Check-List-Civilian Version (PCL-C) [67] scores, gender was not associated with PTSD, however gender moderated the direct effect between psychological distress and PTSD in males more than in females [36]. In the studies by Liu et al. [37] and Tang et al. [39], the scores at the PCL-C scale obtained by males and females were not different, but transgender male reported higher level of PTSD symptoms [37]. By contrast, in the studies of Di Crosta et al. and Passavanti et al., the Impact of Event Scale-revised (IES-R) [68] scores of females were higher than those of males [38, 40]. Women also showed higher levels of stress than males in the Perceived Stress Scale 10 (PSS-10) [69] scores and in the stress subscale of DASS-21 [40]. Also, in the COVID-19 Peritraumatic Distress Index (CPDI) scores, females showed significantly greater psychological distress than males [35].
Age
Both young and old age were risk factors for the development of PTSD, indeed 18–30 years old participants and those over 50 had higher probability of manifesting PTSD [35]. The young age as a risk factor was confirmed by both Tang et al. and Liu et al., who observed that the young participants reported more frequently PTSD symptoms [37, 39].
Education
High level of education was related to higher risk of developing distress in the CPDI, and it was also related to high scores in the PCL-C [39]. In contrast, in the research by Di Crosta et al., the less educated subjects exceed the cutoff on the IES-R scale [38].
Housing
The type of housing affected the level of perceived stress during the pandemic. In the study by Passavanti et al., participants who lived in a house with no outdoor space during quarantine had higher mean scores on the PSS-10 than those who lived in a house with a private garden [40].
Psychological variables
Negative coping strategies are significantly associated with PTSD [36]. Also, in the study of Passavanti et al., the avoiding coping strategy was associated with high scores in all scales [40]. In the study by Liu et al., 61.5% of participants reported feeling lonely during the pandemic [37]. In this study, loneliness and low distress tolerance appeared to be predictive factors for PTSD, whereas high levels of resilience, family support, and perceived instrumental support were related to low probability of developing PTSD.
COVID stressors
Living in an area of China most affected by COVID-19 was a risk factor for PTSD [35, 39]. However, according to Passavanti et al., Chinese participants exhibited lower levels of stress and PTSD compared to participants of other nationalities [40]. In particular, Italians showed the highest stress levels. A strong concern about infection, extreme fear of COVID-19, knowing infected people and seeking news about COVID-19 several times during the day, were all predictive factors for developing PTSD [37, 38, 39] and stress [40].
Risk and protective factors for obsessive compulsive disorder
Obsessive compulsive disorder symptoms were evaluated in 3 out of the 25 studies. One study was conducted in China [42], one in Canada [41], and one in Iran [43]. Data were collected from March to May 2020.
Gender
The study conducted by Darvishi et al. showed a prevalence of obsessive compulsive disorder’s symptoms in women (72.1%) than men (60.3%) [43]. Using the Maudsley Obsessional-Compulsive Inventory (MOCI) [50] underlined higher scores in women on the different subscales “Checking,” “Washing,” “Strictness,” and “Doubting.”
The studies conducted in China [42] and in Canada [41] showed that male gender had scores indicative of possible OCD. In the study of Abba-Aji et al., 63.2% of male participants are concerned about dirt and being infected with viruses and germs, compared with 60.1% of female participants [41]. Moreover, 57.3% of men wash their hands in a special way to avoid contaminations, compared with 53.4% of women.
Age
Younger and older age are risk factors for the development of OCD symptoms. In the study by Ji et al., the males under 26 years old show more symptoms than female younger than 26 years old [42]. In the study done in Iran by Darvishi et al., the mean age of onset of OCD among participants is 16.67 years [43]. In the research conducted by Abba-Aji et al., participants older than 60 years developed a greater concern about dirt, germs, and viruses and adopted more special hand washing, compared to younger age groups [41].
Education
High levels of education are a risk factor for the development of the OCD. 61% of participants with post-secondary education exhibit OCD symptoms, compared to 57.7% of participants with high school diploma and 52.8% of participants with lower levels of education [41].
Psychological variables
Participants who showed concern about dirt, viruses, and germs since the pandemic perceive increased stress, depressive symptoms [41], and symptoms of anxiety [41, 42].
COVID stressors
Fear intensity was positively related to OCD. Participants with possible OCD showed greater intensity of fear [42].
Discussion
The restrictive measures adopted since the beginning of COVID-19 pandemic have undoubtedly slowed down the transmission of the virus (World Health Organization, 2020). However, the impositions of long periods of isolation, social distancing, and loss of personal freedoms have produced important psychological effects, causing the development of mental disorders and emotional distress [5]. These psychological outcomes have affected the population in different ways. Several groups proved more vulnerable, such as healthcare workers [1, 10], COVID-19 patients and survivors [70,71,72,73], chronically and mentally ill patients [74, 75], and pregnant women [11].
Research’s attention has been primarily directed to these risk groups, so in the literature few data are available on the general population [6, 7, 17, 37]. The objective of this review has been to investigate the impact of sociodemographic factors on the psychological responses to the pandemic in the general population. To achieve this goal, we considered only studies in the general population, excluding all studies involving the highest risk groups. The psychological disorders considered were depression, anxiety, sleep disorder, post-traumatic stress disorder, stress, and obsessive compulsive disorder.
The female gender seems to be the main sociodemographic risk factor for the development of disorders such as anxiety, depression, and insomnia. This result is in agreement with the existing literature, suggesting that women are twice as likely as men to develop symptoms of anxiety, depression [76,77,78] and sleep disorders [79]. Furthermore, depression is highly correlated with suicide attempts (72.4%) [80]. Dubè et al., in a meta-analysis of 54 studies, demonstrated an increase in suicidal ideation (10.81%) and suicide attempts (4.68%) during the COVID-19 pandemic, suggesting that female sex is a vulnerability factor for suicidal ideation [81]. From a social and cultural point of view, the pandemic has only highlighted existing cracks. Social norms and structures dictating that women assume caregiving roles are augmented during pandemics [82]. During this period because of the closure of schools, women have suffered a heavy psychological burden, not being able to rely on the help of grandparents in caring for their children due to social restrictions. Contrary to men, they often have to balance household burdens, responsibility over child rearing, and work pressures [83], still being relegated to the role of caregiver. Moreover, during the pandemic, the “glass ceiling” has hardened so the female unemployment rose to 11% compared to 7% in the males (Center for Law and Social Policy, 2020) and this could lead to further psychological distress.
Results on gender differences in PTSD symptoms are ambiguous. Three studies reported that women manifested more psychological symptoms [35, 38, 40], in line with a large part of the literature that associates women gender with a greater vulnerability to stress [84]. Women showed more reactivity than men in the fear processing that increases arousal response and risk of PTSD [85] However, in a study conducted in China [36], the effect of psychological distress on PTSD was significantly higher in males than in females. Chinese men are culturally seen as power figures, dominant especially in status and rights [59], but this socially acquired role might cause high psychological distress especially in this historical period because of the high economic instability. In the USA, men identified as transgender report high level of PTSD [37]. It is to note that COVID-19 pandemic has caused an increase in xenophobic attitudes toward minorities, such as LGBTQ people, because the novelty of illness and unknown’s fear might be associated with the presence of the “other” [86]. Concerning the gender difference in OCD, in two of the three studies [41, 42], OCD symptoms were highly observable in males compared to females, confirming data from the literature, according to which 70% of OCD patients are male [87, 88]. The predisposing factors of OCD are still unknown, but simply asking people to wash their hands, scrub, and sterilize in a ritualized and frequent manner, in order to protect themselves from the virus, may make people more anxious about their health and could lead to OCD occurring for the first time. This suggests that the combination of genetic factors, environment and psychological variables (e.g., fear, anxiety) could be a trigger factor in the etiology of OCD [42, 89].
Young age was an important risk factor for the emergence of mental disorder. Young people are much more exposed to media and social media, so to greater media impact, which could increase stress [35]. Losing relationships and other opportunities, young people are the ones who have sacrificed much to protect the elderly, who are most at risk of infection. Over 50 people are more likely to exhibit symptoms of mental disorders during pandemic because they are the most exposed to the risk of infection.
Interestingly, people with higher education levels show more symptoms of mental disorder than people with poor education. This may be because the pressures related to the pandemic are compounded with the elevated pressures associated with higher academic achievement, delays in studies and entry into the workforce [90].
High income is also a protective factor probably because it provides a sense of stability and security during periods of economic instability, such as this current period [23, 91]. Furthermore, during this pandemic, psychological and social resources become very relevant. Resilience, understood as the personal competence to withstand and adapt to adverse events, was associated with greater psychological well-being [37]. People’s ability to cope with stressful events has been important; in fact passive coping styles increase the risk of depression, anxiety, and PTSD symptoms [36, 40]. A passive approach tends to reinforce negative feelings, rejecting the existence of the stressful event in an attempt to avoid it. An active coping style is a protective factor for mental illness [92], because it enhances the individual’s ability to learn lesson in negative situation, to accept the existence of a negative situation, along with the ability to ask for help [93]. Social support, particularly family support, has a protective role for mental health during this period, because it has a stress buffering effect, improving the quality of life [69].
Finally, excessive worry and fear about the pandemic are risk factors for the emergence of psychological symptoms [6, 37, 39, 42]. Searching for COVID-19-related news several times throughout the day can increase vulnerability to exaggerated or even fake news, easily found especially on social media, increasing fear and worry [94]. Interestingly, some authors talk about “Headline Stress Disorder” caused by the bombardment of news related to COVID-19, causing physical symptoms such as insomnia and palpitations, and eventual mental disorders [95].
A possible limitation of the study is that the papers included in this review have a prevalence of female samples, making a gender-difference analysis not possible. Further studies assessing the effects of the pandemic on psychological health in men may be needed to investigate gender differences.
Conclusions
This review is the first work to collect data on the influence of sociodemographic factors on the psychological responses to the pandemic in the general population, excluding at-risk groups (i.e., healthcare workers, pregnant women, chronically ill, mentally ill, COVID-19 patients, and survivors). This paper suggests that psychological disorders caused by restrictions during the pandemic depend on several sociodemographic risk factors. In fact, it seems that a higher incidence of the disorders highlighted in women than in men, younger and in people with and higher level of education. Conversely, it was observed that the sport practice, social and family supports, and higher income are protective factors. Therefore, a greater interest on the part of local and international governments in public mental health would be appropriate, in order to intervene and try to limit risks and improve the quality of life.
Availability of data and materials
Not applicable.
Abbreviations
- AIS:
-
Athen Insomnia Scale
- BDI:
-
Beck’s Depression Inventory scale
- CES-D:
-
Center for Epidemiological Studies Scale
- COVID-19:
-
Coronavirus disease 2019
- COVID-19 PDI:
-
COVID-19 Peritraumatic Distress Index
- DASS-21:
-
Depression, Anxiety, and Stress Scale-21 items
- DSRS-C:
-
Depression Self-Rating Scale for Children
- ESS:
-
Epworth Sleepiness Scale
- GAD-7:
-
Generalized Anxiety Disorder 7 scale
- GHQ-12:
-
12-Item General Health Questionnaire
- IES:
-
Impact of Event Scale
- IES-R:
-
Impact of Event Scale–Revised
- ISI:
-
Insomnia Severity Index
- LGBTQ:
-
Lesbian, gay, bisexual, transgender, and queer
- MOCI:
-
Maudsley Obsessional-Compulsive Inventory
- OCD:
-
Obsessive compulsive disorder
- PCL-C:
-
Post-traumatic stress disorder CheckList-Civilian Version
- PH9-9:
-
Patient Health Questionnaire-9
- PHQ-8:
-
Patient Health Questionnaire-8
- PSQI:
-
Pittsburgh Sleep Quality Index
- PSS10:
-
Perceived Stress Scale 10
- R-UCLA:
-
Revised UCLA loneliness scale
- SCARED:
-
Screen for Child Anxiety-Related Disorders scale
- SCSQ:
-
Simplified Coping Style Questionnaire
- STAI:
-
State-Trait Anxiety Inventory scale
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD:
-
Post-traumatic stress disorder
- SARS-COV2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- UNICEF:
-
United Nations International Children's Emergency Fund
References
Arden MA, Chilcot J (2020) Health psychology and the coronavirus (COVID-19) global pandemic: a call for research. Br J Health Psychol. https://doi.org/10.1111/bjhp.12414.doi:10.1111/bjhp.12414
Lardone A, Sorrentino P, Giancamilli F, Palombi T, Simper T, Mandolesi L, Lucidi F, Chirico A, Galli F (2020) Psychosocial variables and quality of life during the COVID-19 lockdown: a correlational study on a convenience sample of young Italians. PeerJ 18;8:e10611. https://doi.org/10.7717/peerj.10611
Lardone, A., Turriziani, P., Sorrentino, P., Gigliotta, O., Chirico, A., Lucidi, F., & Mandolesi, L. (2021). Behavioral restriction determines left attentional bias: preliminary evidences From COVID-19 Lockdown. Frontiers in Psychology, 12. https://www.frontiersin.org/article/https://doi.org/10.3389/fpsyg.2021.650715
Somma F, Bartolomeo P, Vallone F, Argiuolo A, Cerrato A, Miglino O, Mandolesi L, Zurlo MC, Gigliotta O (2021) Further to the left: stress-induced increase of spatial pseudoneglect during the COVID-19 lockdown. Front Psychol 12:573846. https://doi.org/10.3389/fpsyg.2021.573846
Taylor, S. (2019). The psychology of pandemics: preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing.
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17(5):1729. https://doi.org/10.3390/ijerph17051729
Wang Y, Di Y, Ye J, Wei W (2021) Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 26(1):13–22. https://doi.org/10.1080/13548506.2020.1746817
Rubin GJ, Wessely S (2020) The psychological effects of quarantining a city. BMJ 368:m313. https://doi.org/10.1136/bmj.m313
Tapia L (2020) COVID-19 and fake news in the Dominican Republic. Am J Trop Med Hyg 102(6):1172–1174. https://doi.org/10.4269/ajtmh.20-0234
Kaufman KR, Petkova E, Bhui KS, Schulze TG (2020) A global needs assessment in times of a global crisis: World psychiatry response to the COVID-19 pandemic. BJPsych Open. 6(3):e48. https://doi.org/10.1192/bjo.2020.25
Saccone G, Florio A, Aiello F, Venturella R, Angelis MCD, Locci M, Bifulco G, Zullo F, Sardo ADS (2020) Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol 223(2):293–295. https://doi.org/10.1016/j.ajog.2020.05.003
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, Min B, Tian Q, Leng H, Du J, Chang H, Yang Y, Li W, Shangguan F, Yan T, Dong H, Han Y, Wang Y, Cosci F, Wang H (2020) Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 89(4):242–250. https://doi.org/10.1159/000507639
Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, Miao J, Zhang C, Yang Y, Sun W, Zhu S, Fan Y, Chen Y, Hu J, Liu J, Wang W (2020) COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine 24:100443. https://doi.org/10.1016/j.eclinm.2020.100443
Pfefferbaum B, North CS (2020) Mental health and the Covid-19 pandemic. N Engl J Med 383(6):510–512. https://doi.org/10.1056/NEJMp2008017
Rana W, Mukhtar S, Mukhtar S (2020) Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr 51:102080. https://doi.org/10.1016/j.ajp.2020.102080
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J (2020) The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 287:112934. https://doi.org/10.1016/j.psychres.2020.112934
Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, Wu L, Sun Z, Zhou Y, Wang Y, Liu W (2020) Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res 287:112921. https://doi.org/10.1016/j.psychres.2020.112921
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Zhou S-J, Wang L-L, Yang R, Yang X-J, Zhang L-G, Guo Z-C, Chen J-C, Wang J-Q, Chen J-X (2020) Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med 74:39–47. https://doi.org/10.1016/j.sleep.2020.06.001
Chen F, Zheng D, Liu J, Gong Y, Guan Z, Lou D (2020) Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav Immun 88:36–38. Epub 2020 May 25. https://doi.org/10.1016/j.bbi.2020.05.061
Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT (2020) Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS One 15(8):e0238162. https://doi.org/10.1371/journal.pone.0238162
Rudenstine S, McNeal K, Schulder T, Ettman CK, Hernandez M, Gvozdieva K, Galea S (2021) Depression and anxiety during the COVID-19 pandemic in an urban, low-income public university sample. J Trauma Stress 34(1):12–22. https://doi.org/10.1002/jts.22600
Fawaz M, Samaha A (2021) E-learning: depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs Forum 56(1):52–57. https://doi.org/10.1111/nuf.12521
Zhang, Z., Zhai, A., Yang, M., Zhang, J., Zhou, H., Yang, C., Duan, S., & Zhou, C. (2020). Prevalence of depression and anxiety symptoms of high school students in Shandong Province during the COVID-19 epidemic. Frontiers in Psychiatry, 11. https://www.frontiersin.org/article/https://doi.org/10.3389/fpsyt.2020.570096
Hammarberg K, Tran T, Kirkman M, Fisher J (2020) Sex and age differences in clinically significant symptoms of depression and anxiety among people in Australia in the first month of COVID-19 restrictions: a national survey. BMJ Open 10(11):e042696. https://doi.org/10.1136/bmjopen-2020-042696
A Debowska B Horeczy D Boduszek D Dolinski 2020 A repeated cross-sectional survey assessing university students’ stress, depression, anxiety, and suicidality in the early stages of the COVID-19 pandemic in Poland Psychol Med 1–4 https://doi.org/10.1017/S003329172000392X
Fitzpatrick KM, Harris C, Drawve G (2020) Living in the midst of fear: depressive symptomatology among US adults during the COVID-19 pandemic. Depress Anxiety 37(10):957–964. https://doi.org/10.1002/da.23080
Bartoszek A, Walkowiak D, Bartoszek A, Kardas G (2020) Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement—a study from Poland. Int J Environ Res Public Health 17(20):7417. https://doi.org/10.3390/ijerph17207417
Bigalke JA, Greenlund IM, Carter JR (2020) Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol Sex Differ 11(1):56. https://doi.org/10.1186/s13293-020-00333-4
Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, Syngelakis M, Holeva V, Diakogiannis I (2020) Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res 289:113076. https://doi.org/10.1016/j.psychres.2020.113076
Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, Liu M, Chen X, Chen J-X (2020) Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 29(6):749–758. https://doi.org/10.1007/s00787-020-01541-4
Wang J, Gong Y, Chen Z, Wu J, Feng J, Yan S, Lv C, Lu Z, Mu K, Yin X (2020) Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors. Sleep Med 74:199–203. https://doi.org/10.1016/j.sleep.2020.08.002
Barrea L, Pugliese G, Framondi L, Di Matteo R, Laudisio D, Savastano S, Colao A, Muscogiuri G (2020) Does Sars-Cov-2 threaten our dreams? effect of quarantine on sleep quality and body mass index. J Transl Med 18(1):318. https://doi.org/10.1186/s12967-020-02465-y
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213
Liang L, Gao T, Ren H, Cao R, Qin Z, Hu Y, Li C, Mei S (2020) Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol 25(9):1164–1175. https://doi.org/10.1177/1359105320937057
Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC (2020) Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res 290:113172. https://doi.org/10.1016/j.psychres.2020.113172
Di Crosta, A., Palumbo, R., Marchetti, D., Ceccato, I., La Malva, P., Maiella, R., Cipi, M., Roma, P., Mammarella, N., Verrocchio, M. C., & Di Domenico, A. (2020). Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID-19 emergency. Frontiers in Psychology, 11. https://www.frontiersin.org/article/https://doi.org/10.3389/fpsyg.2020.567367
Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, Chen S, Xu J (2020) Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord 274:1–7. https://doi.org/10.1016/j.jad.2020.05.009
Passavanti M, Argentieri A, Barbieri DM, Lou B, Wijayaratna K, Foroutan Mirhosseini AS, Wang F, Naseri S, Qamhia I, Tangerås M, Pelliciari M, Ho C-H (2021) The psychological impact of COVID-19 and restrictive measures in the world. J Affect Disord 283:36–51. https://doi.org/10.1016/j.jad.2021.01.020
Abba-Aji A, Li D, Hrabok M, Shalaby R, Gusnowski A, Vuong W, Surood S, Nkire N, Li X-M, Greenshaw AJ, Agyapong VIO (2020) COVID-19 pandemic and mental health: prevalence and correlates of new-onset obsessive-compulsive symptoms in a canadian province. Int J Environ Res Public Health 17(19):6986. https://doi.org/10.3390/ijerph17196986
Ji G, Wei W, Yue K-C, Li H, Shi L-J, Ma J-D, He C-Y, Zhou S-S, Zhao Z, Lou T, Cheng J, Yang S-C, Hu X-Z (2020) Effects of the COVID-19 pandemic on obsessive-compulsive symptoms among university students: prospective cohort survey study. J Med Internet Res 22(9):e21915. https://doi.org/10.2196/21915
Darvishi E, Golestan S, Demehri F, Jamalnia S (2020) A cross-sectional study on cognitive errors and obsessive-compulsive disorders among young people during the outbreak of coronavirus disease 2019. Act Nerv Super 62(4):137–142. https://doi.org/10.1007/s41470-020-00077-x
Soldatos CR, Dikeos DG, Paparrigopoulos TJ (2000) Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res 48(6):555–560. https://doi.org/10.1016/S0022-3999(00)00095-7
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004
Radloff LS (1977) The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401. https://doi.org/10.1177/014662167700100306
Henry JD, Crawford JR (2005) The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 44(Pt 2):227–239. https://doi.org/10.1348/014466505X29657
Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41(3):209–218. https://doi.org/10.1097/00006842-197905000-00004
Hodgson RJ, Rachman S (1977) Obsessional-compulsive complaints. Behav Res Ther 15(5):389–395. https://doi.org/10.1016/0005-7967(77)90042-0
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M (1999) Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38(10):1230–1236. https://doi.org/10.1097/00004583-199910000-00011
Minino R, Troisi Lopez E, Sorrentino P, Rucco R, Lardone A, Pesoli M, Tafuri D, Mandolesi L, Sorrentino G, Liparoti M (2021) The effects of different frequencies of rhythmic acoustic stimulation on gait stability in healthy elderly individuals: a pilot study. Sci Rep 11(1):19530. https://doi.org/10.1038/s41598-021-98953-2
Sorrentino P, Rucco R, Baselice F, De Micco R, Tessitore A, Hillebrand A, Mandolesi L, Breakspear M, Gollo LL, Sorrentino G (2021) Flexible brain dynamics underpins complex behaviours as observed in Parkinson’s disease. Sci Rep 11(1):4051. https://doi.org/10.1038/s41598-021-83425-4
Pesoli M, Rucco R, Liparoti M, Lardone A, D’Aurizio G, Minino R, Troisi Lopez E, Paccone A, Granata C, Curcio G, Sorrentino G, Mandolesi L, Sorrentino P (2022) A night of sleep deprivation alters brain connectivity and affects specific executive functions. Neurol Sci 43(2):1025–1034. https://doi.org/10.1007/s10072-021-05437-2
Birleson P, Hudson I, Buchanan DG, Wolff S (1987) Clinical evaluation of a self-rating scale for depressive disorder in childhood (depression Self-Rating Scale). J Child Psychol Psychiatry 28(1):43–60. https://doi.org/10.1111/j.1469-7610.1987.tb00651.x
Liparoti M, Troisi Lopez E, Sarno L, Rucco R, Minino R, Pesoli M, Perruolo G, Formisano P, Lucidi F, Sorrentino G, Sorrentino P (2021) Functional brain network topology across the menstrual cycle is estradiol dependent and correlates with individual well-being. J Neurosci Res 99(9):2271–2286. https://doi.org/10.1002/jnr.24898
Chen Z, Fiske ST, Lee TL (2009) Ambivalent sexism and power-related gender-role ideology in marriage. Sex Roles 60(11):765–778. https://doi.org/10.1007/s11199-009-9585-9
Spielberger, C. (1971). The State-Trait Anxiety Inventory | Revista Interamericana de Psicología/Interamerican Journal of Psychology. https://journal.sipsych.org/index.php/IJP/article/view/620
Liparoti, M. (2021a). Effects of motor and cognitive loads on postural stability in healthy children. Journal of Human Sport and Exercise. https://doi.org/10.14198/jhse.2021.16.Proc3.08
Liparoti, M. (2021b). Effects of acute and chronic, multimodal and unimodal, physical exercise on brain of elderly people:a systematic review. Giornale Italiano di Educazione alla Salute, Sport e Didattica Inclusiva, 5(2), Article 2. https://doi.org/10.32043/gsd.v5i2.365
Montuori S, D’Aurizio G, Foti F, Liparoti M, Lardone A, Pesoli M, Sorrentino G, Mandolesi L, Curcio G, Sorrentino P (2019) Executive functioning profiles in elite volleyball athletes: preliminary results by a sport-specific task switching protocol. Hum Mov Sci 63:73–81. https://doi.org/10.1016/j.humov.2018.11.011
Sorrentino, P., Lardone, A., Pesoli, M., Liparoti, M., Montuori, S., Curcio, G., Sorrentino, G., Mandolesi, L., & Foti, F. (2019). The development of spatial memory analyzed by means of ecological walking task. Frontiers in Psychology, 10. https://www.frontiersin.org/article/https://doi.org/10.3389/fpsyg.2019.00728
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2(4):297–307. https://doi.org/10.1016/S1389-9457(00)00065-4
Zhang Y, Ma ZF (2020) Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health 17(7):2381. https://doi.org/10.3390/ijerph17072381
Weathers, F., Litz, B., Herman, D., Huska, J. A., & Keane, T. (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper Presented at the Annual Convention of the International Society for Traumatic Stress Studies.
Weiss, D. S. (2007). The Impact of Event Scale: Revised. In J. P. Wilson & C. S. Tang (A c. Di), Cross-cultural assessment of psychological trauma and PTSD (pagg. 219–238). Springer US. https://doi.org/10.1007/978-0-387-70990-1_10
Cohen S, Wills TA (1985) Stress, social support, and the buffering hypothesis. Psychol Bull 98(2):310–357. https://doi.org/10.1037/0033-2909.98.2.310
Bo H-X, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, Wu X, Xiang Y-T (2021) Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med 51(6):1052–1053. https://doi.org/10.1017/S0033291720000999
LaHue SC, James TC, Newman JC, Esmaili AM, Ormseth CH, Ely EW (2020) Collaborative delirium prevention in the age of COVID-19. J Am Geriatr Soc 68(5):947–949. https://doi.org/10.1111/jgs.16480
Russell B, Moss C, Rigg A, Hopkins C, Papa S, Van Hemelrijck M (2020) Anosmia and ageusia are emerging as symptoms in patients with COVID-19: what does the current evidence say. Ecancermedicalscience 14:ed98. https://doi.org/10.3332/ecancer.2020.ed98
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 87:18–22. https://doi.org/10.1016/j.bbi.2020.03.031
Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, Cuomo-Dannenburg G, Thompson H, Walker PGT, Fu H, Dighe A, Griffin JT, Baguelin M, Bhatia S, Boonyasiri A, Cori A, Cucunubá Z, FitzJohn R, Gaythorpe K, Ferguson NM (2020) Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 20(6):669–677. https://doi.org/10.1016/S1473-3099(20)30243-7
Yao H, Chen J-H, Xu Y-F (2020) Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry 7(4):e21–e21. https://doi.org/10.1016/S2215-0366(20)30090-0
Altemus M, Sarvaiya N, Neill Epperson C (2014) Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol 35(3):320–330. https://doi.org/10.1016/j.yfrne.2014.05.004
Kuehner C (2017) Why is depression more common among women than among men? The Lancet Psychiatry 4(2):146–158. https://doi.org/10.1016/S2215-0366(16)30263-2
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC (2018) Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 8(1):2861. https://doi.org/10.1038/s41598-018-21243-x
Mallampalli MP, Carter CL (2014) Exploring sex and gender differences in sleep health: a society for women’s health research report. J Women’s Health 23(7):553–562. https://doi.org/10.1089/jwh.2014.4816
Almaghrebi AH (2021) Risk factors for attempting suicide during the COVID-19 lockdown: Identification of the high-risk groups. J Taibah Univ Med Sci 16(4):605–611. https://doi.org/10.1016/j.jtumed.2021.04.010
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH (2021) Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res 301:113998. https://doi.org/10.1016/j.psychres.2021.113998
Smith J (2019) Overcoming the ‘tyranny of the urgent’: Integrating gender into disease outbreak preparedness and response. Gend Dev 27(2):355–369. https://doi.org/10.1080/13552074.2019.1615288
González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, Muñoz M (2020) Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 87:172–176. https://doi.org/10.1016/j.bbi.2020.05.040
Tolin DF, Foa EB (2008) Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull 132(6):959-92. https://doi.org/10.1037/1942-9681.S.1.37
Felmingham K, Williams LM, Kemp AH, Liddell B, Falconer E, Peduto A, Bryant R (2010) Neural responses to masked fear faces: sex differences and trauma exposure in posttraumatic stress disorder. J Abnorm Psychol 119(1):241–247. https://doi.org/10.1037/a0017551. https://www.unicef.org/media/65931/file/Social%20stigma%20associated%20with%20the%20coronavirus%20disease%202019%20(COVID-19).pdf.
UNICEF. Social stigma associated with COVID-19: a guide to preventing and addressing social stigma. Updated March 2020. https://www.unicef.org/documents/social-stigma-associated-coronavirus-disease-covid-19.
Ruscio AM, Stein DJ, Chiu WT, Kessler RC (2010) The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 15(1):53–63. https://doi.org/10.1038/mp.2008.94
Weissman MM, Bland RC, Canino GJ, Greenwald S, et al. (1994). The cross national epidemiology of obsessive compulsive disorder: The Cross National Collaborative Group. The Journal of Clinical Psychiatry, 55(3, Suppl), 5–10.
Adam, D. (2020). The hellish side of handwashing: how coronavirus is affecting people with OCD. The Guardian, 14.
Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, Kessler RC, Liu H, Mortier P, Nock MK, Pinder-Amaker S, Sampson NA, Aguilar-Gaxiola S, Al-Hamzawi A, Andrade LH, Benjet C, Caldas-de-Almeida JM, Demyttenaere K, Bruffaerts R (2016) Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med 46(14):2955–2970. https://doi.org/10.1017/S0033291716001665
Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M (2020) Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med Sci Monit. 26:e924609. https://doi.org/10.12659/MSM.924609.
Lazarus RS, Folkman S (1984). Stress, appraisal, and coping. Springer Publishing Company.
Liu D, Fu L, Jing Z, Chen C (2016) Post-traumatic stress disorder and it’s predictors among tibetan adolescents 3years after the high-altitude earthquake in China. Arch Psychiatr Nurs 30(5):593–599. https://doi.org/10.1016/j.apnu.2016.01.005
Erku DA, Belachew SA, Abrha S, Sinnollareddy M, Thomas J, Steadman KJ, Tesfaye WH (2021) When fear and misinformation go viral: pharmacists’ role in deterring medication misinformation during the «infodemic» surrounding COVID-19. Res Social Adm Pharm 17(1):1954–1963. https://doi.org/10.1016/j.sapharm.2020.04.032
Dong M, Zheng J (2020) Letter to the editor: Headline stress disorder caused by Netnews during the outbreak of COVID-19. Health Expect 23(2):259–260. https://doi.org/10.1111/hex.13055
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Each of the authors was involved in the study and preparation, as follows: F.B.: conceptualization, writing (original draft preparation); A.L: conceptualization, writing (original draft preparation). M.L: writing (review); R.M: methodology, writing (review); P.S: project administrator, writing (review), final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biondi, F., Liparoti, M., Lacetera, A. et al. Risk factors for mental health in general population during SARS-COV2 pandemic: a systematic review. Middle East Curr Psychiatry 29, 85 (2022). https://doi.org/10.1186/s43045-022-00251-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-022-00251-8