Abstract
Background
Nursing has a reputation for being one of the most stressful occupations. As a result of their work, many nurses suffer from anxiety and depression. Nurses are also at risk of poor sleep owing to their work nature. This study aimed to examine the relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses. A descriptive cross-sectional study design was utilized in this study. Setting/sample: This study was conducted at El Azazi Hospital for Mental Health, Al-Sharkia Governorate on 139 mental health nurses. Four tools were used in this study: Socio-demographic data sheet, Work–Family Conflict Scale, Arabic Pittsburgh Sleep Quality Index, and Arabic Center for Epidemiologic Studies Depression Scale.
Results
Results revealed that, a significant percentage of mental health nurses suffered from poor sleep quality and depressive symptoms, there were highly statistically significantly positive correlations between work–family conflict (WFC) and both of Pittsburgh Sleep Quality Index (PSQI) and depressive symptoms among nurses.
Conclusions
Working with psychiatric patients affected their nurses, which disturbed their sleep quality and led to depressive symptoms. As well, increasing work–family conflict in mental health nurses leads to poor sleep quality and depressive symptoms. Family interference with work, sleep quality, and work interference with family were statistically significant predictors of depressive symptoms.
Similar content being viewed by others
Background
Nursing is often acknowledged as a difficult and demanding career. The stress levels of 92% of hospital nurses ranged from moderate to extremely high [1]. According to recent studies, high-stress situations can cause physical and psychological difficulties in nurses, such as work–family conflicts (WFCs), poor sleep, and poor health [2]. Due to busy work hours and a variety of physical and psychosocial job pressures, nurses are at a significant risk of work–family conflict and its harmful consequences [3].
In addition to the recognized work stress measures, the importance of WFC on organizational behavior and occupational health has been documented. The WFC has been defined as “a type of inter-role conflict in which the role pressures from the work and family domains are mutually contradictory in some respects.” Participation in one role makes it difficult to participate in the other [4]. Work–family conflict is defined as a bidirectional role conflict that includes both work interference with family (WIF) and family interference with work (FIW). It is a major source of stress for workers, and it has a substantial impact on work, family, behavior, and health (3). The WIF occurs when a person’s job role has a negative impact on his/her home/family role, while FIW occurs when problems and troubles from home/family follow them to work and obstruct their work role [5].
For each direction of work–family conflict, there are three types: time-based conflict, strain-based conflict, and behavior-based conflict. Time-based conflict arises when time spent on activities within one role cannot be committed to activities within another one. Strain-based conflict occurs when one function’s strain affects another’s performance. Behavior patterns in one role may be incompatible with behavior expectations in another, resulting in behavior-based conflict [6].
Nurses have been demonstrated to have more issues with work interfering with their personal lives than with personnel lives interfering with their work [7]. In this regard, one study found that 50% of nurses experience chronic work interference with family, and 11% of nurses experience chronic family interference with work [8]. Work–family conflict has a variety of negative consequences. Sleep quality is linked to work–family conflict. The worsening of sleep quality is proportional to the severity of work–family conflict [9]. Furthermore, WFC have been found to be positively connected to depressive symptoms in previous studies [3, 10].
The quality of one’s sleep has a big impact on one’s physical and mental health. It includes both quantitative and qualitative sleep parameters including sleep length, sleep latency, and the number of arousals, as well as more subjective features like “depth” or “restfulness.” [11] As a result of their heavy workload, nurses suffer from a variety of sleep disorders, including poor sleep quantity and quality, acute and chronic sleep loss, and sleep interruptions [12]. In addition to the sleep challenges that confront most shift workers, nurses frequently have family responsibilities such as child and/or elder care that interfere with daily sleep. Work–family conflict has been recognized as a possible cause of sleep problems among patient care employees [7].
The correlation between WFCs and sleep is extensively documented. Working women’s sleep disturbance is greatly increased when their WFCs have a high level of different dimensions [13]. Nurses are a high-risk group for developing depressive symptoms. Nurses work in hospitals under extreme physical and psychological stress as an essential part of the healthcare system. Negative psychosocial aspects in the workplace have been related to poor mental and physical health in nurses in several nations [14]. People who have a lot of work–family conflict have more depressive symptoms, marital issues, poor health, and lower life satisfaction, well-being, and family life quality [15].
Nurses who do not get enough sleep have a higher risk of depression, poor interpersonal relationships, burnout, and even medical errors [16]. Sleep problems, especially insomnia, have been related to an increased risk of depression. According to a meta-analysis based on 21 studies, people with insomnia are twice as likely to develop depression as people who do not have sleep problems [17].
According to a study on the impact of sleep quality on work, safety, psychology, and other aspects, nurses with poor sleep quality are more likely to suffer from depression and inattention at work. Their sense of personal identity will be harmed as a result of their sleep problems, and they will become more frustrated. As a result, nurses gradually lose interest in their jobs [18]. Previous studies have shown that a poor work environment can cause sleep difficulties and that sleep disturbances might anticipate specific working situations [19]. Similarly, bidirectional associations between working conditions and depressive symptoms, as well as sleep problems and depressive symptoms, may exist [20].
Significance of the study
Work–family conflict can arise from a lack of ability to balance work and home commitments. For nurses, role conflict is a source of stress. The stressor has a negative impact on both physical and mental health [21]. As a result, a high level of work–family conflict has been related to a variety of physical and mental health problems [15].
Many studies have explored the correlation between work–family conflict, sleep problems, and depression among nurses in general, but there is a lack of literatures which studied these variables together in the mental health nursing population. Thus, this study aims to fill gaps in existing researches by examining the relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses.
Aim of the study
This study aimed to examine the relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses.
Methods
Research questions
-
What is work–family conflict encountered by mental health nurses?
-
What is the type of sleep quality among mental health nurses?
-
Are there depressive symptoms among mental health nurses?
-
What is the relation between work–family conflict, sleep quality, and depressive symptoms among mental health nurses?
Research design
A descriptive cross-sectional study design was used in this study.
Subjects
A convenience sample of 139 nurses working at Al Azazi Hospital for Mental Health at Abo-Hamad City in Al-Sharkia Governorate, Egypt.
Sample size
The total number of nurses working in the previously mentioned setting is 150 nurses. The study sample consisted of 139 nurses who agreed to participate in the study. All nurses available (139), in the previously mentioned setting, who agreed to participate in the study with no age limit of both sexes, and all educational levels were recruited for this study.
Tools of data collection
Four tools were used for data collection.
Tool I: Socio-demographic data sheet
It includes personal characteristics of the studied nurses such as age, sex, educational level, years of experience, marital status, residence, income, and shift manner.
Tool II: Work–Family Conflict Scale
The WFC Scale was developed by Carlson, Kacmar, and Williams [22]. This scale measures two types of conflicts with three dimensions: time-based, strain-based, and behavior-based work that interferes with family (WIF), and time-based, strain-based, and behavior-based that family interferes with work (FIW). There are three statements to reflect each direction and dimension. The WFC Scale contained two subscales: the WIF and the FIW subscales. The two subscales comprised 18 items, and each of the two subscales included nine items. The WIF subscale measured the extent to which work demands interfere with family-related responsibilities, whereas the FIW subscale measured the extent to which family demands interfere with work-related responsibilities. The scale was translated using the translate-back-translate technique to ensure its content validity by the researchers. The tool was then revised by a group of experts in the fields of psychiatry and psychiatric nursing for further face and content validation.
Scoring system
Each item was scored on a Likert scale of 5 points ranging from 1 “strongly disagree”; to 5 “strongly agree.” A higher score indicates a greater WFC.
Tool III: Arabic Pittsburgh Sleep Quality Index
Nurses’ sleep quality was evaluated using the Arabic Pittsburgh Sleep Quality Index (A-PSQI) [23]. The original PSQI was developed by Buysse et al. [24] to reflect the sleep quality of an individual in the past month. It contains 19 questions and addresses seven dimensions: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction.
Scoring system
Each dimension is scored on a 4-point Likert scale (0–3). The sum of scores for these seven dimensions gives a total score that ranges between 0 and 21, with higher scores indicating poorer sleep quality. The cut-off level of A-PSQI: good sleep quality (0–5) and poor sleep quality (6–21).
Tool IV: Arabic Center for Epidemiologic Studies Depression Scale
The Arabic version of the Center for Epidemiologic Studies Depression Scale (CES-D) was used to measure the depressive symptoms of nurses [25]. The CES-D is a 20-item self-report instrument developed by Radloff [26] to detect current depression symptomatology in persons aged 18 and older throughout the past week. The CES-D comprises four aspects: depressed affect (blue, depressed, lonely, cry, sad—items 1, 3, 6, 9, 10, 14, 17, 18); positive affect (good, hopeful, happy, enjoy—items 4, 8, 12, 16); somatic and retarded activity (bothered, appetite, effort, sleep, get going—items 2, 5, 7, 11, 13, 20); interpersonal (unfriendly, dislike—items 15 and 19). The scoring of positive items (4, 8, 12, 16) is reversed.
Scoring system
Each item is rated on a 4-point Likert scale (0) “rarely or none of the time”; (1) “some or a little of the time”; (2) “occasionally or a moderate amount of the time”; and (3) “most or all of the time.” The maximum score on this scale is 60, and higher scores are associated with depression. The cut-off level of CES-D: non-depressed subjects (0–20); depressed (21–60).
Pilot study
A pilot research was conducted on 10% of the total sample (14 nurses) before the main study began to test the tools’ clarity and applicability, as well as to estimate the time required for data collection. Participants were told to fill out the questionnaire and write down any questions that were unclear or difficult to answer. Because the data collecting forms did not need to be updated, the nurses who participated in the pilot study were included in the main study sample.
Content validity and reliability
The tools’ content validity was assessed by a panel of, three experts, professors of psychiatric nursing and nursing administration, who amended them for clarity, relevance, applicability, inclusivity, understanding, and simplicity of use, and minor changes were made based on their feedback. Tools II, III, and IV reliability was assessed by Cronbach’s alpha coefficient test through their internal consistency. They presented a good level of reliability as follow: The WFC scale has been found to have a good level of reliability in this study as Cronbach’s alpha was 0.87 for the WIF section and 0.89 for the FIW section, A-PSQI score (α = 0.70), and CES-D score (α = 0.84)
Fieldwork
After receiving permission to proceed with the study, the researchers presented the study’s objectives and procedures, as well as information collection forms, to the administrators of El-Azazi Hospital for Mental Health. The questionnaires were then distributed to nurses who agreed to participate in the study after giving their informed consent. The questionnaires took an average of 30 to 45 min to complete. Data were collected over 2 months from the beginning of May until the end of June 2020.
Statistical analysis
All data were collected, tabulated, and statistically analyzed using the Statistical Package for Social Sciences (SPSS) version 20.0 for Windows (SPSS Inc., Chicago, IL, USA 2011). Quantitative data were expressed as the mean ± SD, and range and qualitative data were expressed as absolute frequencies (number) and relative frequencies (percentage). Continuous data were checked for normality by using Shapiro–Wilk’s test. Student’s t test was used to compare between two groups for normally distributed variables. F (ANOVA) test was used to compare between more than two groups for normally distributed variables. Percent of categorical variables were compared using a chi-square test or Fisher’s exact test when appropriate. Power of test was 80%. All tests were two-sided, and p-value < 0.05 was considered statistically significant (S), p-value ≥ 0.05 was considered statistically insignificant (NS).
Multilinear regression
Situations frequently occur in which we are interested in the dependency of a dependent variable on an independent variable.
Formally, the model for multiple linear regression, given n observations, is:
Y = a + β1*X1 + β2*X2+ β3*X3
Y = the variable that we are trying to predict
X = the variable that is used to predict
a = the intercept (constant)
β = coefficient of X represents the mean change in the dependent variable for one unit of change in the predictor variable (independent)
t test = test of significance
Results
Table 1 shows that slightly less than three-quarters (74.8%) of the studied nurses’ age was less than 30 years with a mean age of 28.46 ± 6.28. As regards gender, less than three-quarters (73.4%) of them were female. Majority of studied nurses were married and working at shift manner (87.8% & 95.7 respectively). More than half of them had technical institute level of education and have sufficient income (54.0% & 59% respectively). Regarding experience (in years), more than three-fifths (63.3%) of the studied nurses have a work experience less than 10 years with a mean of 8.14 ± 5.14 years. According to residence, more than three-quarters (77.7%) of the studied nurses were from rural areas.
Table 2 reveals that more than three quarters (78.4%) of studied nurses had poor sleep quality with the mean score of 8.14 ± 3.1. The same table also shows that, slightly less than two-thirds (64.7%) of studied nurses suffered from depressive symptoms with a mean score of 25.3 ± 9.73.
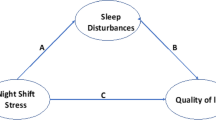
Figure 1 demonstrates that, the mean score of nurses as regards work interference with family (WIF) was 29 ± 7.49, family interference with work (FIW) was 26.295 ± 5.95, and overall work–family conflict (WFC) was 55.295 ± 12.62.
Table 3 shows that there was statistically significant relationship between sleep quality among nurses and their gender (p < 0.05) as majority (84.3%) of female nurses have poor sleep quality. Concerning education, the same table also reveals that there was a statistically significant relationship between sleep quality among nurses and their educational level (p < 0.05) where poor sleep quality was evident among technical institute graduate nurses (85.3%) and bachelor degree nurses (83.3%). As well, the same table demonstrates that there was a statistically significant relationship between sleep quality among nurses and their income level (p < 0.05) as majority (89.5%) of studied nurses who have insufficient income have poor sleep quality.
Table 4 indicates that there was a highly statistically significant relationship between depression among nurses and their age (p < 0.001), where all nurses whose age was 30 years or more suffered from depressive symptoms. The table also reveals that there was a highly statistically significant relationship between depression among nurses and their marital status (p < 0.001) as majority (82.4%) of single nurses were not depressed, while 71.3% of married nurses were depressed. The same table also shows that there was a statistically significant relationship between depression among nurses and their years of experience (p < 0.05), where majority (80.4%) of nurses who have 10 years of experience or more suffered from depressive symptoms.
Table 5 shows that there were highly statistically significant relationships between nurses’ age and each of Work Interference with family, family interference with work and overall work–family conflict (p < 0.001), where nurses whose age was 30 years or more were affected more than nurses who were less than thirty, with mean scores 34.25 ± 5.39, 30.6 ± 4.36 and 64.85 ± 8.35 compared to 27.23 ± 7.29, 24.84 ± 5.73, and 52.07 ± 12.19 respectively.
As regards marital status, the table reveals statistically significant relationships between nurses’ marital status and each of work interference with family, family interference with work, and overall work–family conflict (p < 0.01), as married nurses manifested more disturbance than single with mean scores 29.63 ± 7.54, 26.85 ± 5.59, and 56.49 ± 12.33 compared to 24.41 ± 5.43, 22.29 ± 7.06, and 46.70 ± 11.55 respectively.
The same table also indicates a statistically significant relationship between nurses’ educational level and family interference with work (p < 0.05), where technical institute graduate nurses experienced more family interference with work than Diploma and Bachelor nurses, with a mean score 27.18 ± 5.87 for technical institute graduate nurses compared to 25.82 ± 6.32 and 22.75 ± 2.63 for diploma and bachelor nurses respectively.
Table 6 points out that, there were highly statistically significant positive correlations between depression and each of WIF, FIW, overall WFC, and PSQI. As well, highly statistically significant positive correlations were found between WIF and each of FIW, overall WFC, and PSQI. Additionally, there were highly statistically significant positive correlations between FIW and both overall WFC and PSQI. Besides, a significant positive correlation was found between FIW and nurses’ age. This table also reveals that WFC was highly statistically significantly positively correlated with overall WFC and PSQI and significantly positively correlated with nurses’ age. Also, PSQI was highly statistically significantly positively correlated with nurses’ age and significantly positively correlated with nurses’ years of experience.
Table 7 demonstrates multivariate linear regression to predict depression score from Family interference with work score, sleep quality score, and work interference with family score. These variables statistically significantly predicted depression score, f = (43.5), p = .0001, R2 = 0.492. All three variables added statistical significance to the prediction.
Discussion
Due to demanding work schedules (e.g., shift work, long work hours, and overtime) and a variety of physical and psychosocial occupational stresses, nurses are at a high risk for work–family conflict and its negative consequences (e.g., workload and time pressure). Work–family conflict has been studied in the nursing staff and has been linked to mental disorders such as emotional tiredness and depressive symptoms [14]. Nurses with sleep difficulties due to excessive workload were at a higher risk of work stress and burnout as a result of their work and the patients [27].
The aim of this study was to examine the relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses. The findings generally answered research questions.
The current study found that nurses had a mean age of 28.46 ± 6.28 with a range of 21 to 50 years that less than three-quarters of them were female, that the majority of them were married, and that their mean working experience score was 8.14 ± 5.14. Similarly, it was reported that the mean working experience in nursing was 15.73 years (SD = 5.64 years) in a study conducted in Greece, where the majority of those who took part were women (64.5%) and married (59.1%) [28].
Furthermore, Chueh, Chen, and Lin [29] found that the 119 participants’ mean age was 31.6 (SD = 7.6) years, with a range of 20 to 50 years, and that more than half of them were married. However, their result is lower than the mean working experience score reported in previous studies among nurses. In a similar study, Christina and Konjengbam [11] reported a greater mean score of 12.90 ± 8.057 among nursing staff at a tertiary hospital in Manipur, based on Cheng et al. [30], whose observations revealed that the mean job experience was 6.7 ± 6.4 years and more nurses who working in teaching medical center were female.
According to the current study findings, the nurses’ work interference with family mean score was 29 ± 7.49, family interference with work mean score was 26.295 ± 5.95, and work–family conflict mean score was 55.295 ± 12.62. As a result, WIF was found to be more significant than FIW. The first research question was answered by this result. In accordance with this study results, Sugawara et al. [4] found that, the WIF mean score was 23.4 ± 8.1 and the FIW mean score was 18.7 ± 6.2 among mental health nurses. As well, previous and recent researches conducted in China indicated that work–family conflict was more significant than family–work conflict [18, 31].
In the present study, nurses’ marital status was found to have statistically significant relations with WIF, FIW, and overall WFC. This could be explained by the fact that married nurses were more disturbed than unmarried ones due to that nurses with small children, those with employee husbands, nurses who work rotational shifts, and those who work in wards where patients are hurried leading to that those nurses are overworked much consequently experienced more role challenges. This finding is consistent with that of a study conducted in Iran, which showed that family influences include family members’ expectations of the nurse, as well as conflicts between family and professional roles [21].
The age of nurses under study was found to have highly statistically significant relations with work interference with family, family interference with work, and overall work–family conflict, with nurses aged 30 years or more being influenced more than nurses aged less than thirty. This could be due to that older nurses are given more duties and roles. However, this result contradicted with findings of a recent research carried out on Filipino nurses, which found that nurses’ age strongly predicted WFC, with newly qualified nurses showing higher levels of WFC than older nurses [32].
The current study result revealed that a statistically significant relation was detected between nurses’ educational level and family interference with work, with technical institute graduate nurses having the highest mean as experiencing the most family interference with work, followed by diploma nurses, and bachelor’s nurses were experiencing the least. This result is consistent with that of a study on Filipino nurses, with a B.Sc.N degree who reported a higher level of WFC when compared to nurses with higher education [32]. As previously clarified, higher education is required for the development of improved cognitive capacities, strong clinical judgment, and problem-solving ability, all of which are crucial when dealing with work–family conflict [33]. Furthermore, a much higher education can boost personal resources like self-efficacy or confidence, professional autonomy, and skill mastery [34].
According to this study results, more than three-quarters of studied nurses had poor sleep quality. The second research question was answered by this result. This could be due to that the current study is carried on mental nurses, who work in difficult working conditions and have long working hours with limited flexibility. In a related survey conducted in China, the sleep quality of medical nurses was poor [35]. As well, in Korea, 79.8% of clinical nurses reported having poor sleep quality [36] which is greater than the prevalence of 69.9% poor sleep quality among Saudi nursing students [37].
However, these findings are higher than the prevalence reported among nurses by previous studies. Using the Chinese version of the PSQI, the incidence of poor sleep quality among nurses in North China was 56.7% [38], an even higher prevalence of 65% among nursing professionals in Southeastern Brazil [39], and the prevalence of 46% among South Indian nurses [40].
As well, these previous results agreed with several scattered researches which found a relatively higher percentage more than 70% of nurses who work in general hospitals and emergency departments had poor sleep quality [41,42,43,44]. Similarly, 71.3% of nurses working in teaching medical centers in Taiwan reported poor sleep quality [30]. Poor sleep quality is a common health problem among staff nurses, according to the current study data. However, if nurses experience poor sleep quality on a regular basis, it may influence their professional and family life, as well as their health.
The current study results indicated that, the nurses’ sleep quality mean score was 8.14 ± 3.1, which agrees with those of a research conducted in a tertiary hospital in Manipur about sleep quality among nurses which found that the mean sleep quality score was 4.98 ± 3.123 [11]. Similar research in Istanbul indicated that the average age of the nurses on the PSQI scale was 6.65 ± 3.48, and 61.9% of the nurses reported poor sleep quality [45]. Furthermore, Dong et al. [46] detected that the average PSQI score among clinical nurses in general hospitals was 7.32 ± 3.24, with 3163 participants receiving a PSQI ≥ 5, while Chueh, et al. [29] revealed that sleep status had an average PSQI score of 7.2 (SD = 3.1) points.
The current study results revealed that, there was a statistically significant relation between nurses’ poor sleep quality and representing majority female sex, as well as a statistically significant relation between nurses’ sleep quality and their educational level, with the majority of technical institute graduates and bachelor degree nurses having poor sleep quality. As well, there was a statistically significant relation between sleep quality and their income level among nurses, with the majority of nurses with insufficient income having poor sleep quality.
As expected, working more night shifts a month is connected with an increase in sleep disturbances, as shown by several large studies on clinical nurses in general hospitals [43, 46, 47], while the current study result showed that, nurses’ sleep quality had no statistically significant relation with shift manner. This could be explained as most of them are taking daily naps during a night shift which may reduce sleep disturbances. Similarly, another research conducted in a tertiary hospital located in Imphal, Manipur, India, found no difference between nurses who performed only day shifts and those whose shifts included night, with regard to sleep quality [11].
According to the present study results, the nurses’ depressive symptoms mean score was 25.3 ± 9.73, with slightly less than two-thirds of them experiencing depressive symptoms. The third research question was answered by this result. This could be explained by the fact that nurses working in mental hospitals and clinics are more likely to suffer from depressive symptoms as a result of the stressful working conditions, job uncertainty, and life pressures they face. This finding is to some extent, similar to that of a previous study conducted in Japan in 2017, which reported that, the mean score of nurses’ depression was 16.7 ± 10.5 [4]. However, according to one other previous study conducted in the same year in Iran, the frequency of depression among Iranian nurses was only 22%. Furthermore, the average score of nurses’ depression was 10.5 (SD = 7.2) points among nurses working in general hospitals [48], which was greater than that of a very recent study research conducted in northern Taiwan [29].
The present study results revealed that, nurses’ depressive symptoms had highly statistically significant relations with their age. This means that all nurses aged 30 years or more suffered from depressive symptoms. This result is consistent with that of a research about sleep disturbance and depression in Iranian nurses, which revealed that age was positively associated with depression [27]. Additionally, a study conducted in China aimed to assess the association between work-family conflict and depressive symptoms among female nurses found that people under the age of 40 were more likely to have depressive symptoms [14]. Similarly, a study conducted in Malayer, Iran reported that work experience was positively associated with depression among nurses in general hospitals [27].
The current study findings confirmed that the majority of nurses having 10 years of experience or more suffered from depressive symptoms. This may be due to experiencing work stress, role overload, and a lack of compliment. Nurses’ depressive symptoms were found to have highly statistically significant positive relationships with their age, as well as with marital status, while with years of experience, it was only a statistically significant relation. This finding is consistent with that of Tsaras et al., who investigated “Predicting Factors of Depression and Anxiety in Mental Health Nurses,” in Greece, and found that age, marital status, educational level, and nursing experience were all associated with elevated depressive symptoms in mental health nurses [28].
In the same line, work–family conflict was positively associated with depressive symptoms among nurses in a previous study conducted in the northeastern United States [3], which is also consistent with other previous studies’ results in nursing populations [14, 49]. Moreover, an earlier study conducted in Malaysia found strong associations among work–family conflict, psychological strain, stress, anxiety, and depression [50].
Nurses’ family interference with work was shown to be highly statistically significantly positively correlated with sleep quality and their age in the current study. This highlighted that nurses beyond the age of 30 had a greater impact than nurses under the age of thirty. This study result is congruent with that of Aazami et al., who in their study on Malaysian working women found that high levels of strain-based FIW impact the sleep quality of women in their 30s. They explained that women in their 30s have often established their jobs and are well-versed in their fields. As a result, stress from home responsibilities interferes with job performance, and the magnitude of this type of conflict is strong enough to disrupt sleep among women working as civil servants [13].
The current study result showed that highly statistically significantly positive correlation between overall WFC and Pittsburgh Sleep Quality Index, which means that work–family conflict leads to poor sleep quality. The fourth research question was answered by this result. The preceding finding is consistent with that of Zhang, et al. [3], who found that sleep disturbances are related to both work–family conflict and depressive symptoms in nurses, verifying justifying their hypothesis. Sleep quantity and quality have previously been linked to work–family conflict among nurses [51].
Work–family conflict was found to be positively related to the Pittsburgh Sleep Quality Index in a study of Chinese nurses working in comprehensive tertiary hospital [18], and a previous study found a link between work–family conflicts and sleep issues [52]. However, a study of 744 nursing assistants in 15 non-unionized facilities in Maryland and New England found that the relationship between work–family conflict and sleep quantity or quality was not statistically significant (p > .05). The difference could be attributed to various settings. Generally, WFCs of hospital nurses working in nursing homes must be reduced, according to hospital management [8].
In this study, highly statistically significant correlation was found between depressive symptoms and overall work family conflict. This study result answered the fourth research question. This result agrees with that of a study on Chinese female nurses which showed that high levels of WFCs can affect work performance, and as a result, lead to psychological depression among female Chinese nurses [14]. In addition, Zhang et al. reported that there was a significant a correlation between work–family conflict and depressive symptoms in nurses (β = 2.22, p < .001) [3].
The current study findings demonstrated that depressive symptoms and Work Interference with Family are highly statistically significantly positively correlated. This finding was comparable to that of Zhang et al., who found that more work–family interference was linked to higher physical and psychological demands at work [8].
Concerning the nurses’ depressive symptoms, the current study found that depression symptoms among nurses were very statistically significantly positively correlated with sleep quality. This finding is consistent with the findings of a study conducted among Saudi nursing students, which found a weak positive correlation between sleep quality and depression (r = 0.274, p < 0.001) [37]. Similarly, a very recent study conducted in northern Taiwan that tried to examine which psychological distress variables are associated with sleep difficulties among female nurses, found that depression (β = 0.15, p = .007) was significantly associated with sleep disturbance [29].
According to the findings of this study, family interference with work was extremely statistically significantly positively correlated with work interference with family. This result could be seen as a conflict between work and family responsibilities, as high work demands deplete time and energy that could otherwise be employed for family responsibilities. As a result, the family’s role will be threatened. This result differed from that found in Jakarta, which indicated a negative and substantial link between both directions of work–family conflict (WIF & FIW) among working mother [5].
Finally, a multi variate linears regression was used to predict nurses’ depressive symptoms score from Family interference with work score, sleep quality score, and Work interference with family score in the current study. These variables predicted depressive symptoms score as statistically significantly (f = 43.5, p = .0001, R2 = 0.492). In comparing this result with that of a study done in Maryland and New England, showed that Sleep quality was introduced into the multivariate linear regression model for work–family conflict and mental health. Poor sleep quality was linked to lower mental health scores (model 2, R2 = 16.1%, β = − 5.22, p < .01), and it reduced the link between work–family conflict and mental health by 5.5% [8].
Similarly, Christina and Konjengbam [11], found in their study that, Poor sleep quality, can lead to depression in their study. Moreover, depression is exacerbated by poor sleep quality [45]. Additionally, a significant relationship was found between work–family conflict and sleep disruptions (model 2, R2 = .15, F [11, 346] = 5.71, β = 3.67, p < .001) [3], as well as between sleep disturbances and depressed symptoms (model 3, R2 = .32, F[11, 341] = 14.33, β = .27, p < .001) and nurses are more likely to suffer from depression and lack of concentration in their everyday work if their sleep quality is poor [18].
Conclusions
Working with psychiatric patients affected their nurses, which disturbed their sleep quality and led to depressive symptoms. as well, increasing work–family conflict in mental health nurses leads to poor sleep quality and depressive symptoms. Family interference with work, sleep quality, and work interference with family were statistically significant predictors of depressive symptoms.
Based on the current study findings, the following recommendations are suggested: Evidence-based interventions for mental health nurses to encourage healthy sleeping habits (e.g., sleep hygiene education and stress management programs); To relieve the impacts of work–family conflict and increase overall health in nurses, sleep education and training in the workplace, such as cognitive behavioral therapy and complementary and integrative health techniques, is recommended; involving nurses in work scheduling decisions, lowering nurses’ burden by increasing staffing, and honestly listening to nurses’ hopes and perspectives when difficulties occur from their job or family life are all ways to improve the work environment and reduce work–family conflict; improving the level of nurses’ mindfulness and reducing work–family conflict are recommended to improve nurses’ sleep quality and alleviate depressive symptoms; replicating the research using a longitudinal design provides stronger evidence of its important findings to generalize them.
Availability of data and materials
As detailed in the “References” section, all data was accessible through the Internet.
Abbreviations
- WFCS:
-
Work
Family Conflict Scale
- FIW:
-
Family interferes with work
- WIF:
-
Work interferes with family
- A-PSQI:
-
Arabic Pittsburgh Sleep Quality Index
- CES-D:
-
Center for Epidemiologic Studies Depression
References
Jordan TR, Khubchandani J, Wiblishauser M (2016) The impact of perceived stress and coping adequacy on the health of nurses: a pilot investigation. Nurs Res Pract 1–11. https://doi.org/10.1155/2016/5843256
Ghislieri C, Gatti P, Molino M, Cortese CG (2017) Work-family conflict and enrichment in nurses: between job demands, perceived organisational support and work-family backlash. J Nurs Manage 25:65–75. https://doi.org/10.1111/jonm.12442
Zhang Y, Duffy JF, De Castillero ER (2017) Do sleep disturbances mediate the association between work-family conflict and depressive symptoms among nurses? A cross-sectional study. J Psychiatr Ment Health Nurs 24:620–628. https://doi.org/10.1111/jpm.12409
Sugawara N, Danjo K, Furukori H, Sato Y, Tomita T, Fujii A, Nakagami T, Kitaoka K, Yasui-Furukori N (2017) Work–family conflict as a mediator between occupational stress and psychological health among mental health nurses in Japan. Neuropsychiatr Dis Treat 13:779–784. https://doi.org/10.2147/NDT.S127053
Bramadewandhana P, Parahyanti E (2018) Moderating role of psychological capital on relationship between work-family conflict and job satisfaction among working mothers. Adv Soc Sci Educ Hum Res 139:297–304. https://doi.org/10.2991/uipsur-17.2018.15
Greenhaus HJ, Beutell NJ (1985) Sources of conflict between work and family roles. Acad Manag Rev 10(1):76–88. https://doi.org/10.5465/amr.1985.4277352
Jacobsen HB, Reme SE, Sembajwe G, Hopcia K, Stoddard AM, Kenwood C, Buxton OM (2014) Work-family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health Safety 62(7):282–291. https://doi.org/10.1177/216507991406200703
Zhang Y, Punnett L, Nannini A (2016) Work-family conflict, sleep, and mental health of nursing assistants working in nursing homes. Workplace Health Safety 65(7):295–303. https://doi.org/10.1177/2165079916665397
Chen SS, Zheng DY, Chen QY (2017) Study on the relationship between work-family conflict and sleep quality for operating room nurses. Hospital Manag Forum 34(6):44–47 http://www.oaj.pku.edu.cn/wk3/yygllt/EN/Y2017/V34/I6/44
Obidoa C, Reeves D, Warren N, Reisine S, Cherniack M (2011) Depression and work-family conflict among corrections officers. J Occup Environ Med 53:1294–1301. https://doi.org/10.1097/JOM.0b013e3182307888
Christina S, Konjengbam S (2019) Sleep quality among nurses in a tertiary hospital in Manipur. J Med Soc 33(3):146–151. https://doi.org/10.4103/jms.jms_80_20www.jmedsoc.org
Geiger-Brown J, Rogers VE, Trinkoff AM, Kane RL, Bausell RB, Scharf SM (2012) Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol Int 29(2):211–219. https://doi.org/10.3109/07420528.2011.645752
Aazami S, Mozafari M, Shamsuddin K, Akmal S (2016) Work-family conflict and sleep disturbances: the Malaysian working women study. Ind Health 54(1):50–57. https://doi.org/10.2486/indhealth.2015-0086
Hao J, Wu D, Liu L, Li X, Wu H (2015) Association between work-family conflict and depressive symptoms among Chinese female nurses: the mediating and moderating role of psychological capital. Int J Environ Res Public Health 12(6):6682–6699. https://doi.org/10.3390/ijerph120606682
Zhou S, Da S, Guo H, Zhang X (2018) Work–family conflict and mental health among female employees: a sequential mediation model via negative affect and perceived stress. Front Psychol 9:544. https://doi.org/10.3389/fpsyg.2018.00544
Lu L, Lok KI, Zhang Q, Zhang L, Xiang Y, Ungvari GS, Hall BJ, An FR, Xiang YT (2021) Sleep disturbance and its association with quality of life among psychiatric nurses in China. Peer J 9:e10659. https://doi.org/10.7717/peerj.10659
Baglioni C, Riemann D (2012) Is chronic insomnia a precursor to major depression? Epidemiological and biological findings. Curr Psychiatry Rep 14:511–518. https://doi.org/10.1007/s11920-012-0308-5
Liu K, Yin T, Shen Q (2020) Relationships between sleep quality, mindfulness and work-family conflict in Chinese nurses: a cross-sectional study. Appl Nurs Res 55. https://doi.org/10.1016/j.apnr.2020.151250
Akerstedt T, Garefelt J, Richter A, Westerlund H, Hanson LLM, Sverke M, Kecklund G (2015) Work and sleep – a prospective study of psychosocial work factors, physical work factors, and work scheduling. Sleep 38:1129–1136. https://doi.org/10.5665/sleep.4828
Tang K (2014) A reciprocal interplay between psychosocial job stressors and worker well-being. A systematic review of the “reversed” effect. Scand J Work Environ Health 40:441–456 https://www.jstor.org/stable/43188043
Alhani F, Mahmoodi-Shan GR (2018) Work–family conflict as a stressor in the lifestyle of nurses: a content analysis. J Nurs Midwifery Sci 5(3):79–88. https://doi.org/10.4103/JNMS.JNMS_26_18
Carlson DS, Kacmar KM, Williams LJ (2000) Construction and initial validation of a multidimensional measure of work-family conflict. J Vocat Behav 56(2):249–276. https://doi.org/10.1006/jvbe.1999.1713
Suleiman KH, Yates BC, Berger AM, Pozehl B, Meza J (2010) Translating the Pittsburgh sleep quality index into Arabic. West J Nurs Res 32(2):250–268. https://doi.org/10.1177/0193945909348230
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Beshai S, Dobson SK, Adel A (2013) Psychometric properties of the Center for Epidemiologic Studies Depression Scale in an Egyptian student sample: a preliminary report. Middle East Current Psychiatry 20:223–228. https://doi.org/10.1097/01.XME.0000433324.92161.6d
Radloff LS (1977) The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401. https://doi.org/10.1177/014662167700100306
Ariapooran S (2019) Sleep problems and depression in Iranian nurses: the predictive role of workaholism. Iran J Nurs Midwifery Res 24:30–37. www.ijnmrjournal.net. https://doi.org/10.4103/ijnmr.IJNMR_188_17
Tsaras K, Papathanasiou LV, Vus V, Panagiotopoulou A, Katsou MA, Kelesi M, Fradelos EC (2018) Predicting factors of depression and anxiety in mental health nurses: a quantitative cross-sectional study. MED ARCH 72(1):62–67. https://doi.org/10.5455/medarh.2017.72.62-67
Chueh KH, Chen KR, Lin YH (2021) Psychological distress and sleep disturbance among female nurses: anxiety or depression? J Transcult Nurs 32(1):14–20. https://doi.org/10.1177/1043659619881491
Cheng SY, Lin PC, Chang YK, Lin YK, Lee PH, Chen SR (2018) Sleep quality mediates the relationship between work–family conflicts and the self-perceived health status among hospital nurses. J Nurs Manag 27:381–387. https://doi.org/10.1111/jonm.12694
Guo YA, Xu L, Wang PL, Zou LL, Bao SS (2018) Work-family conflict and associated factors among nurses at different reproductive states. J Nurs Sci 33(19):58–60
Labrague LJ, Ballad CA, Fronda DC (2021) Predictors and outcomes of work–family conflict among nurses. Int Nurs Rev 68(3):349–357. https://doi.org/10.1111/inr.12642
AllahBakhshian M, Alimohammadi N, Taleghani F, Nik AY, Abbasi S, Gholizadeh L (2017) Barriers to intensive care unit nurses’ autonomy in Iran: a qualitative study. Nurs Outlook 65(4):392–399. https://doi.org/10.1016/j.outlook.2016.12.004
Labrague LJ, McEnroe-Petitte DM, Tsaras K (2019) Predictors and outcomes of nurse professional autonomy: a cross-sectional study. Int J Nurs Pract 25(1):e12711. https://doi.org/10.1111/ijn.12711
Li Y, Li XF, Xie L, Shao L, Dong Y (2018) Analytical survey to assess factors associated with sleep quality in registered medical nurses in tertiary first-class hospitals in Shenyang. J China Med Univ 47(7):666–669. https://doi.org/10.12007/j.issn.0258-464
Park E, Lee HY, Park CSY (2018) Association between sleep quality and nurse productivity among Korean clinical nurses. J Nurs Manag 26(8):1051–1058. https://doi.org/10.1111/jonm.12634
AlAmer M, Shdaifat E, Alshowkan A, Eldeen AG, Jamama A (2020) Exploring associations between internet addiction, depressive symptoms, and sleep disturbance among Saudi nursing students. Open Nurs J 14(1):29–36. https://doi.org/10.2174/1874434602014010029
Wang Y, Xie J, Yang F, Wu S, Wang H, Zhang X, Liu H, Deng X, Xie W, Yu S (2015) Comorbidity of poor sleep and primary headaches among nursing staff in north China. J Headache Pain 16(88):1–6. https://doi.org/10.1186/s10194-015-0571-z
Palhares VDC, Corrente JE, Matsubara BB (2014) Association between sleep quality and quality of life in nursing professionals working rotating shifts. Rev Saude Publica 48:594–601. https://doi.org/10.1590/S0034-8910.2014048004939
Khade Y, Behera S, Korradi S (2018) Study of insomnia, day time sleepiness and sleep quality among south Indian nurses. J Clin Diagn Res 12:9–12. https://doi.org/10.7860/JCDR/2018/32602.11392
Chien PL, Su HF, Hsieh PC, Siao RY, Ling PY, Jou HJ (2013) Sleep quality among female hospital Staff Nurses. Sleep Disorders:1–6. https://doi.org/10.1155/2013/283490
Lee CY, Chen HC, Tseng MCM, Lee HC, Huang LH (2015) The relationships among sleep quality and chronotype, emotional disturbance, and insomnia vulnerability in shift nurses. J Nurs Res 23(3):225–235. https://doi.org/10.1097/jnr.0000000000000095
Lin SH, Liao WC, Chen MY, Fan JY (2014) The impact of shift work on nurses’ job stress, sleep quality and self-perceived health status. J Nurs Manag 22(5):604–612. https://doi.org/10.1111/jonm.12020
Weaver AL, Stutzman SE, Supnet C, Olson DM (2016) Sleep quality, but not quantity, is associated with self-perceived minor error rates among emergency department nurses. Int Emerg Nurs 25:48–52. https://doi.org/10.1016/j.ienj.2015.08.003
Tarhan M, Aydin A, Ersoy E, Dalar L (2018) The sleep quality of nurses and its influencing factors. Eurasian J Pulmonol 20:78–84. https://doi.org/10.4103/ejop.ejop_35_18www.eurasianjpulmonol.com
Dong H, Zhang Q, Sun Z, Sang F, Xu Y (2017) Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry 17(1):241. https://doi.org/10.1186/s12888-017-1402-3
Han Y, Yuan Y, Zhang L, Fu Y (2016) Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatr Danub 28:176–183 https://hrcak.srce.hr/file/258835
Shahri SSS, Ghashghaee A, Behzadifar M, Bragazzi NL, Behzadifar M, Mousavinejad N, Ghaemmohamadi MS, Ebadi F, Seyedin H (2017) Depression among Iranian nurses: a systematic review and meta-analysis. Med J Islamic Republic Iran (MJIRI) 31(130):1–9. https://doi.org/10.14196/mjiri.31.130
Leineweber C, Westerlund H, Chungkham HS, Lindqvist R, Runesdotter S, Tishelman C (2014) Nurses’ practice environment and work-family conflict in relation to burn out: a multilevel modeling approach. PLoS One 9(5):e96991. https://doi.org/10.1371/journal.pone.0096991
Amstad FT, Meier LL, Fasel U, Elfering A, Semmer NK (2011) A meta-analysis of work-family conflict and various outcomes with a special emphasis on cross-domain versus matching-domain relations. J Occup Health Psychol 16:151–169. https://doi.org/10.1037/a0022170
Berkman LF, Liu SY, Hammer L, Moen P, Klein LC, Kelly E, Buxton OM (2015) Work-family conflict, cardiometabolic risk, and sleep duration in nursing employees. J Occup Health Psychol 20(4):420–433. https://doi.org/10.1037/a0039143
Lallukka T, Rahkonen O, Lahelma E, Arber S (2010) Sleep complaints in middle-aged women and men: the contribution of working conditions and work-family conflicts. J Sleep Res 19:466–477. https://doi.org/10.1111/j.1365-2869.2010.00821
Acknowledgements
The authors would like to thank the entire administrative staff and participant mental health nurses for their cooperation with the research team.
Funding
This study received no particular grant from state, private, or non-profit funding agencies.
Author information
Authors and Affiliations
Contributions
The research concept was suggested by RF. All authors contributed to the collection, interpretation, and editing of the manuscript by designing the research methodology, writing the manuscript, editing the manuscript, developing the study methodology, revising the data analysis, and developing the study methodology. The final manuscript was read and accepted by all contributors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The researchers submitted an official letter from the scientific Research Ethics Committee in the Faculty of Nursing, Zagazig University, and the Dean of the Faculty of Nursing issued a formal letter to the Director of Al-Azazi Hospital for Mental Health in Abo Hamad City to obtain permission to conduct the study. The committee’s reference number is unavailable. Subjects who agreed to participate after learning about the study’s goals signed a written informed consent form, indicating that they were given the option to withdraw from the study at any time without explanation and that the information they provided would be kept confidential and used only for research purposes.
Consent for publication
Not applicable.
Competing interests
There is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamed, B.E.S., Ghaith, R.F.A. & Ahmed, H.A.A. Relationship between work–family conflict, sleep quality, and depressive symptoms among mental health nurses. Middle East Curr Psychiatry 29, 19 (2022). https://doi.org/10.1186/s43045-022-00183-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-022-00183-3