Abstract
Background
Coronavirus Disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome-Coronavirus-2, still remains prevalent and severe. We aimed to evaluate the effects of pre-existing atrial fibrillation and new-onset atrial fibrillation (NOAF) on the clinical severity and mortality of COVID-19.
Results
Between April and December 2020, 5577 patients with positive PCR and/or COVID-19 compatible findings in computed tomography hospitalized were enrolled retrospectively. Total and in-hospital mortality, need for intensive care unit (ICU), need for mechanical ventilation, and recurrent hospitalization results of 286 patients with pre-existing AF before hospitalization and 82 patients with NOAF during hospitalization were evaluated. Preexisting AF was associated with a 2-fold increase in total and in-hospital mortality [OR (2.16 (1.62–2.89), 2.02 (1.48–2.76), P < 0.001, respectively]. NOAF was associated with a 14-fold increase in total mortality and a 12-fold increase in in-hospital mortality [OR(14.72 (9.22–23.5), 12.56 (8.02–19.68), P < 0.001], respectively]. However, pre-existing AF and NOAF resulted in increased ICU admission, mechanical ventilation, and recurrent hospitalization. In the Cox regression analysis, NOAF was observed as an independent risk factor for mortality.
Conclusions
Pre-existing AF and in-hospital NOAF were associated with increased mortality and severity in hospitalized COVID-19 patients. In addition, NOAF was observed as an independent prognostic indicator in terms of total mortality.
Similar content being viewed by others
Background
Coronavirus Disease-2019 (COVID-19) is a viral disease caused by Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-COV-2) and caused a pandemic [1]. SARS-COV-2 has led to the fact that about 215 million people have been infected worldwide and has caused the death of 4.4 million people [2]. The clinical spectrum of COVID-19 ranges from asymptomatic infection to acute respiratory distress syndrome (ARDS), multiorgan failure, and death [3]. COVID-19 can cause various clinical entities such as hypercoagulation, acute kidney injury, or cytokine storm [4]. Risk factors such as male gender, advanced age, and comorbidity are associated with COVID-19 severity [5]. Death occurs more frequently in older age or patients with comorbidities such as cardiovascular disease (CVD), arterial hypertension (HT), diabetes mellitus (DM), chronic obstructive lung disease (COPD), chronic kidney disease (CRF), obesity, or cancer. In addition, the rate of critical illness is higher among hospitalized patients, and approximately 30% of patients need intensive care [6]. Although COVID-19 mainly affects the lungs, Cardiovascular (CV) complications such as arrhythmia, acute myocardial injury, left ventricular dysfunction, acute pericarditis, venous and arterial thromboembolic events, and acute coronary syndrome may also develop. These conditions are associated with poor outcomes [7]. Atrial fibrillation (AF) has been frequently observed in COVID-19 patients [8]. The effect of this arrhythmia, which is so common and has significant clinical consequences, on the COVID-19 process has also aroused curiosity. We aimed to evaluate the impact of new-onset AF (NOAF) and pre-existing AF on COVID-19 clinical severity and mortality.
Methods
April-December 2020, the data of 5856 hospitalized patients diagnosed with COVID-19 were retrospectively analyzed, and 5577 patients, whose records are fully accessible, enrolled in the study. This study was conducted with the approval of the local ethics committee (Approval Number: 2021-2/28) and in accordance with the Helsinki Declaration. Because of the retrospective design, informed consent was not obtained.
Patient complaints, previous medical history, comorbidities, history of drug use, and laboratory parameters were determined from electronic medical records. The results containing laboratory parameters of the blood sample taken within the first 24 h after admission were examined. Electrocardiographs (ECG) were taken at the time of admission to the hospital and when the patients had symptoms and were recorded by accessing the patient files. Drug treatments in the last year and mortality records were determined and collected from the National Medical Record System using the Social Security Institution website.
The patients were diagnosed with COVID-19 based on their symptoms, examination findings, imaging findings, blood parameters, and PCR test results [9]. Patients with negative PCR tests and no findings consistent with COVID-19 on CT were excluded from the study.
Pre-existing AF was defined as patients who already used oral anticoagulants and had documented AF before hospitalization, regardless of AF type (paroxysmal, persistent, permanent, or permanent). NOAF was defined as occurs during hospitalization due to COVID-19 and lasting more than 30 s on the monitor, regardless of the duration of the arrhythmia or the presence and severity of symptoms [10].
The patients' data were recorded after an average of 6 months of follow-up. The endpoints of the study were determined as total mortality, in-hospital mortality, need for ICU admission and mechanical ventilation, and recurrent hospitalization.
Statistical analysis
Statistical analyses were performed using SPSS 23.0 software (SPSS Inc., Chicago, IL, USA). All continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range [IQR]). Baseline features were evaluated by appropriate statistical tests; t-test for continuous variables with normal distribution, Mann–Whitney U test for continuous variables with non-normal distribution, chi-square for categorical variables, and ANOVA for parametric variables with three independent groups. The Kruskal–Wallis test was used to analyze the three groups that did not have a normal distribution. Regression analysis was performed for statistically significant parameters obtained from the univariate analysis, and independent predictors of 6 month mortality were examined. The effect of AF types on total mortality in the entire cohort in patients with Pre-existing AF, patients with NOAF, and patients with non-AF was investigated by using Kaplan–Meier analysis. A P-value ≤ 0.05 was considered significant.
Results
The mean age of 5577 patients included in our study was 61.4 ± 16.4, and 49.8% were male. 286 patients had pre-existing AF (5.1%), and 82 patients had NOAF (1.5%). The incidence of pre-existing and NOAF increased with increasing age and was more common in males. PCR test was positive in 3809 (68.3%) patients, and radiological signs of infection were observed in 4753 (85.2%) patients. Hypertension (HT), coronary artery disease (CAD), heart failure (HF), COPD, and cerebrovascular events (CVE) were observed more frequently in patients with pre-existing AF and NOAF. In addition, Ferritin, D-dimer, c-reactive protein (CRP) troponin, N-terminal pro-brain natriuretic peptide (NTproBNP) were higher, especially in NOAF patients. Baseline demographic data and laboratory parameters of the study population are shown in Table 1.
Considering the study's endpoints, the total mortality rate in the patients was 13.5%, and the in-hospital mortality was 11.2%. The rate of patients needing intensive care was 16.1%, the rate of intubation was 8.8%, and the rate of recurrent hospitalization was 10.4%. Total mortality rate in patients without AF, pre-existing AF and NOAF was 12.2% (633), 23.1% (66), 67.1% (55), in-hospital mortality rate 10.1% (526), 18.5% (53), 58.5% (48), need for intensive care unit 14.7% (766), 27.6% (79), 63.4% (52) mechanical ventilation need 7.9% (410), 15 (43), 48.8% (40), recurrent hospitalization rate was 9.9% (518), 15.7% (45), 19.5% (16), mean hospital stay was 8 days, 9 days, 17 days (respectively).
Pre-existing AF was associated with a 2-fold increase in total and in-hospital mortality [OR (2.16 (1.62–2.89), 2.02 (1.48–2.76), P < 0.001], respectively). Likewise, it was associated with an increased need for ventilation and recurrent hospitalizations [OR (2.21, 2.07, 1.69, P < 0.001, respectively). It was found that NOAF increased total mortality 14 times and in-hospital mortality 12 times [OR(14.72 (9.22–23.5), 12.56 (8.02–19.68), P < 0.001]). It was also observed that the need for ventilation and the need for re-hospitalization increased significantly [OR(10.05, 11.14, 2.19, respectively, P < 0.001)] (Tables 2 and 3).
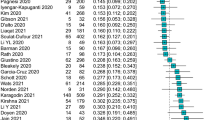
The regression analysis, performed to investigate the effect of AF and other comorbid diseases on total mortality, determined that AF increased mortality 1.5 times. In the analysis of which of the AF subtypes the increase in mortality was related to, it was observed that this increase was caused by NOAF and was an independent risk factor in predicting mortality. In addition, the effects of non-AF, NOAF, and pre-existing AF on survival in Kaplan–Meier analysis are shown in Fig. 1.
Discussion
Our study revealed that there was a significant increase in total and in-hospital mortality, need for intensive care, requiring mechanical ventilation, and recurrent hospitalizations with NOAF and pre-existing AF in hospitalized COVID-19 patients.
AF is more common in those with comorbidities such as male gender, advanced age, heart failure (HF), HT, coronary artery disease (CAD), heart valve disease, cerebrovascular events (CVE), obesity, DM, and CRF [11]. In addition, the frequency of NOAF increases in patients with ARDS and sepsis, as well as in patients with viral respiratory infections [12]. Similarly, comorbidities with pre-existing AF and NOAF were more common in our study.
The prevalence of arrhythmias in COVID-19 patients is variable [8]. However, arrhythmias associated with COVID-19 are mostly atrial. In a study, atrial arrhythmia was observed in 15.8% of the patients, and 9.6% were newly diagnosed [13]. In another study, arrhythmia was observed in 18.5% of patients requiring invasive mechanical ventilation, and atrial arrhythmia was observed in 95.8% of them [14]. Various data are available on the prevalence of AF in COVID-19, and it is considered the most common arrhythmia to occur. The proportion of patients hospitalized for COVID-19 with a history of AF varies between 5 and 25% [8, 15]. However, there are limited reliable data on NOAF in COVID-19 patients, and its prevalence ranges from 3.5 to 5% [16]. In addition, it has been shown that the frequency of AF increases in ICU patients with COVID 19 [17]. In our study, 5.1% of COVID-19 patients had pre-existing AF, and NOAF developed in 1.4%.
Although the exact mechanisms of AF remain unclear, ion channel dysfunction, Ca (2 +) processing abnormalities (handling abnormalities), structural remodeling, and autonomic dysfunction play a role in its pathophysiology. The pathophysiology of cardiac manifestations and arrhythmias in COVID-19 is uncertain, but the mechanisms explaining the pathogenesis are direct viral myocardial damage, hypotension, and angiotensin-converting enzyme 2 (ACE2) receptor downregulation, increased inflammatory state, increased endogenous catecholamine and adrenergic status, and electrolyte abnormalities [18]. SARS-CoV-2 uses ACE2 receptors to enter host cells, including type 2 pneumocytes, cardiomyocytes, pericytes, macrophages, and endothelial cells. ACE2 also plays an important role in angiotensin II regulation and protects against the detrimental effect of the renin–angiotensin–aldosterone system (RAAS) on the cardiovascular system [19]. RAAS has an important role in the development of AF. RAAS modulates the electrical and mechanical properties of the atrium. RAAS dysregulation causes the release of angiotensin II further contributing to AF [20]. It can be thought that SARS-CoV-2 may induce AF by its effect on ACE2 and RAAS. Increased metabolic stress resulting from systemic infections and sepsis may lead to the development of AF [12]. In addition, patients hospitalized for pneumonia have an increased risk of developing AF. Furthermore, it is believed that the increased inflammatory state and cytokine storm observed in COVID-19 patients lead to the development of AF. In another study, it was suggested that SARS-COV-2 virus pericytes could contribute to the pathogenesis of AF by binding, causing inflammation of the heart tissue, and altering atrial cellular electrophysiology [21].
Regardless of COVID-19, AF is associated with high mortality and risk of CV complications in the general population. AF is a predictor of mortality for patients presenting with myocardial infarction, HF, and ischemic stroke, and the presence of comorbidities are associated with worse outcomes in patients with AF [22]. In addition, AF increases mortality, especially in patients hospitalized for sepsis [23]. However, the development of AF in severe COVID-19 patients is thought to increase the risk of adverse events in patients. Various studies have been conducted on the relationship between COVID-19 and AF. Some studies have shown that AF is associated with an increased risk of death in COVID-19 patients [13]. The presence of AF in COVID-19 is associated with the need for mechanical ventilation and increased mortality, especially in those with more serious diseases [24]. Similarly, in our study, it was observed that both pre-existing AF and NOAF significantly increased total and in-hospital mortality, intensive care hospitalization, and the need for mechanical ventilation. Unlike our study, in some studies, it was observed that AF did not affect in-hospital mortality in COVID-19 [16].
Advanced age and male gender have been shown to be predictors of mortality in COVID-19. In a meta-analysis, it was shown that advanced age and male gender are associated with HT and severe disease and increase all-cause mortality in patients with AF [25]. Similarly, advanced age and male gender were observed more frequently in pre-existing AF and NOAF patients in our study, and comorbidities such as HT, CAD, HF, COPD, and CVE were observed at a higher rate. Our study is consistent with research suggesting that AF is a risk factor independent of age and comorbidities [26].
Thromboembolic complications resulting in death have increased in COVID-19 patients. The high level of D-dimer, which indicates increased hypercoagulation, is associated with an increase in infection, sepsis, and mortality in COVID-19 patients. In addition, increased inflammation during COVID-19 has been associated with more severe disease and an increased risk of death [27]. Elevated levels of CRP and interleukin-6 (IL-6) were observed in AF patients accompanying COVID-19, indicating increased inflammation [28]. In our study, ferritin, troponin, and NTproBNP were found to be high as well as high CRP and D-dimer in pre-existing AF and NOAF patients, which shows the effect of increased inflammation on mortality.
In addition to inflammatory and comorbid conditions, AF is associated with hemodynamic instability and thromboembolism, and the presence of AF can directly worsen the prognosis [29]. In another study, it has been shown that patients who develop NOAF in COVID-19 have a high risk of embolic events [30]. The thromboembolic event data in our study are limited, but embolic complications may be one of the reasons for the increased mortality in NOAF and pre-existing AF.
Conclusions
We observed an increase in disease severity and mortality in patients with NOAF and pre-existing AF hospitalized due to COVID-19. We determined that the prognosis was worse and was an independent predictor of mortality, especially in patients who developed NOAF.
Limitations
Our study has some limitations. Retrospective design is the main limitation of this study, there may be hidden confusion, and the reliability of the results is questionable. Moreover, our study is observational and therefore cannot show the cause-effect relationship between the clinical prognosis of COVID-19 patients, and it needs to be confirmed by randomized controlled trials. Second, there is a lack of long-term ECG monitoring, and silent AF is likely to go unnoticed. Again, echocardiography data could not be reached. Third, being a single-center study, it may not apply to other populations because it is represented by a population with a specific geographic region and socio-economic conditions. Fourth, hospitalized patients due to COVID-19 were included in the study, so the generalizability of our findings to asymptomatic or symptomatic COVID-19 patients who were not hospitalized may be limited. However, we believe that our findings contribute to chronic and AF prevalence data in COVID-19 patients, identifying risk factors causing the development of NOAF, and its impact on the mortality and severity of COVID-19.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus Disease-2019 (COVID-19),
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome-Coronavirus-2
- AF:
-
Atrial fibrillation
- NOAF:
-
New-onset atrial fibrillation
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- ARDS:
-
Acute respiratory distress syndrome
- CVD:
-
Cardiovascular disease
- HT:
-
Arterial hypertension
- DM:
-
Diabetes mellitus
- COPD:
-
Chronic obstructive lung disease
- CRF:
-
Chronic kidney disease
- ECG:
-
Electrocardiography
- CRP:
-
C-reactive protein
- NTproBNP:
-
N-terminal probrain natriuretic peptide
- CAD:
-
Coronary artery disease
- CVE:
-
Cerebrovascular accident
- ACE2:
-
Angiotensin-converting enzyme 2
- RAAS:
-
Renin-angiotensin-aldosterone system
- HF:
-
Heart failure
- IL:
-
Interleukin
References
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W et al (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579(7798):270–273. https://doi.org/10.1038/s41586-020-2012-7
Coronavirus disease (COVID-19) Weekly epidemiological update and weekly operational update 29/08/2021 Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan China. JAMA 323(11):1061–1069. https://doi.org/10.1001/jama.2020.1585
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ et al (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395(10229):1033–1034. https://doi.org/10.1016/S0140-6736(20)30628-0
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 323(13):1239–1242. https://doi.org/10.1001/jama.2020.2648
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y et al (2020) Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York city: prospective cohort study. BMJ 369:m1966. https://doi.org/10.1136/BMJ.m1966
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE et al (2020) Factors associated with COVID-19-related death using OpenSAFELY. Nature 584(7821):430–436. https://doi.org/10.1038/s41586-020-2521-4
Gopinathannair R, Merchant FM, Lakkireddy DR, Etheridge SP, Feigofsky S, Han JK et al (2020) COVID-19, and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J Interv Card Electrophysiol 59(2):329–336. https://doi.org/10.1007/s10840-020-00789-9
TC. Sağlik Bakanliği Halk Sağliği Genel Müdürlüğü.Covid-19 (Sars-Cov-2 Enfeksiyonu) Genel Bilgiler, Epidemiyoloji Ve Tani 2020.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C et al (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J 42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612
Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S (2014) Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol 6:213–220. https://doi.org/10.2147/CLEP.S47385
Klein Klouwenberg PM, Frencken JF, Kuipers S, Ong DS, Peelen LM, Van Vught LA et al (2017) Incidence, predictors, and outcomes of new-onset atrial fibrillation in critically ill patients with sepsis a cohort study. Am J Respir Crit Care Med 195(2):205–211. https://doi.org/10.1164/rccm.201603-0618OC
Peltzer B, Manocha KK, Ying X, Kirzner J, Ip JE, Thomas G et al (2020) Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19. J Cardiovasc Electrophysiol 31(12):3077–3085. https://doi.org/10.1111/jce.14770
Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A et al (2020) Clinical characteristics of Covid-19 in New York city. N Engl J Med 382(24):2372–2374. https://doi.org/10.1056/NEJMc2010419
Bertini M, Ferrari R, Guardigli G, Malaga M, Vitali F, Zucchetti O et al (2020) Electrocardiographic features of 431 consecutive, critically ill COVID-19 patients: an insight into the mechanisms of cardiac involvement. Europace 22(12):1848–1854. https://doi.org/10.1093/Europace/euaa258
Russo V, Di Maio M, Mottola FF, Pagnano G, Attena E, Verde N et al (2020) Clinical characteristics and prognosis of hospitalized COVID-19 patients with incident sustained tachyarrhythmias: a multicenter observational study. Eur J Clin Invest 50(12):e13387. https://doi.org/10.1111/eci.13387
Reinelt P, Karth GD, Geppert A, Heinz G (2001) Incidence and type of cardiac arrhythmias in critically ill patients: a single-center experience in a medical-cardiological ICU. Intensive Care Med 27(9):1466–1473. https://doi.org/10.1007/s001340101043
Kochi AN, Cagliari AP, Forleo GB, Fassini GM, Tondo C (2020) Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol 31(5):1003–1008. https://doi.org/10.1111/jce.14479
Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD (2020) Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N Engl J Med 382(17):1653–1659. https://doi.org/10.1056/NEJMsr2005760
Jansen HJ, Mackasey M, Moghtadaei M, Belke DD, Egon EE, Tuomi JM et al (2018) Distinct patterns of atrial electrical and structural remodeling in angiotensin II-mediated atrial fibrillation. J Mol Cell Cardiol 124:12–25. https://doi.org/10.1016/j.yjmcc.2018.09.011
Kennedy-Lydon T (2017) Immune functions and properties of resident cells in the heart and cardiovascular system: pericytes. Adv Exp Med Biol 1003:93–103. https://doi.org/10.1007/978-3-319-57613-8_5
Friberg L, Rosenqvist M, Lip GY (2012) Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish atrial fibrillation cohort study. Eur Heart J 33(12):1500–1510. https://doi.org/10.1093/eurheartj/ehr488
Gandhi S, Litt D, Narula N (2015) New-onset atrial fibrillation in sepsis is associated with increased morbidity and mortality. Neth Heart J 23(2):82–88. https://doi.org/10.1007/s12471-014-0641-x
Abdulrahman A, Hussain T, Nawaz S, AlShaikh S, Almadani A, Bardooli F (2021) Is atrial fibrillation a risk factor for worse outcomes in severe COVID-19 patients: a single-center retrospective cohort. J Saudi Heart Assoc 33(2):160–168. https://doi.org/10.37616/2212-5043.1255
Romiti GF, Corica B, Lip GYH, Proietti M (2021) Prevalence and impact of atrial fibrillation in hospitalized patients with COVID-19: a systematic review and meta-analysis. J Clin Med 10(11):2490. https://doi.org/10.3390/jcm10112490
Spinoni EG, Mennuni M, Rognoni A, Grisafi L, Colombo C, Lio V et al (2021) Contribution of atrial fibrillation to in-hospital mortality in patients with COVID-19. Circ Arrhythm Electrophysiol 14(2):e009375. https://doi.org/10.1161/CIRCEP.120.009375
Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS et al (2021) C-reactive protein and clinical outcomes in patients with COVID-19. Eur Heart J 42(23):2270–2279. https://doi.org/10.1093/eurheartj/ehaa1103
Zylla MM, Merle U, Vey JA, Korosoglou G, Hofmann E, Muller M et al (2021) Predictors and prognostic implications of cardiac arrhythmias in patients hospitalized for COVID-19. J Clin Med 10(1):133. https://doi.org/10.3390/jcm10010133
Bikdeli B, Madhavan MV, Jimenez D, Church T, Dreyfus I, Driggin E et al (2020) COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 75(23):2950–2973. https://doi.org/10.1016/j.jacc.2020.04.031
Pardo Sanz A, Salido Tahoces L, Ortega Perez R, Gonzalez Ferrer E, Sanchez Recalde A, Zamorano Gomez JL (2021) New-onset atrial fibrillation during COVID-19 infection predicts poor prognosis. Cardiol J 28(1):34–40. https://doi.org/10.5603/CJ.a2020.0145
Acknowledgements
Not applicable
Funding
No funds were received to fulfill this work.
Author information
Authors and Affiliations
Contributions
SA: Study design, data analyze and drafting of manuscript. EA: Data analyze, statistical analysis. OG, İS, SŞA: Data interpretation and analysis FA, RD, ML, KK: Study supervision, text writing, proofreading. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was received from the local ethical committee of Medical School of Erzurum Education and Research Hospital (Approval Number: 2021-2/28). Because of the retrospective design informed consent was not obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aydemir, S., Aksakal, E., Aydınyılmaz, F. et al. Does new onset and pre-existing atrial fibrillation predict mortality in COVID-19 patients?. Egypt Heart J 74, 53 (2022). https://doi.org/10.1186/s43044-022-00291-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-022-00291-9