Abstract
Background
Routine thrombus aspiration during primary PCI does not improve clinical outcomes. Although recent guidelines for management of patient presented by ST-elevation myocardial infarction treated by primary PCI does not recommend routine use of thrombus aspiration and ranking it as class III recommendation. However, there is remaining uncertainty about rule of TA in group of patients presented by STEMI and their initial coronary angiogram shows large thrombus burden as there is a logical rationale for greater benefit, and still, there are no clear guidelines for management of this group of patients; the aim of this study is to evaluate the in-hospital and short-term outcome of using manual thrombus aspiration in STEMI patients undergoing primary PCI and showing large thrombus burden.
Results
The study was prospective observational study included 209 patients referred to coronary care unit (CCU) with diagnosis of STEMI who had undergone primary PCI; their initial coronary angiography show totally occluded infarct-related artery with heavy thrombus burden. Patients were divided into 2 groups: group (B) which included 73 patients, who had undergone PTCA and manual thrombus aspiration followed by stent to culprit lesion, and group (A) which included 136 patients, who had undergone conventional PTCA and stent of culprit lesion within the period from November 2016 till July 2018. Patients had a pre-discharge echo and were followed up for 4 weeks for major adverse cardiac events (MACE) and echo repeated after 1 month of discharge.
It was found that thrombus aspiration in heavy thrombus burden cases had improved in-hospital mortality and in-hospital secondary endpoints (TIMI flow, MBG, ST-segment resolution), as well as 30-day MACE and LV systolic function.
Conclusion
In patients presented with STEMI and heavy thrombus burden culprit artery, manual thrombus aspiration has great value in reducing index hospitalization and 1 month mortality and improve TIMI flow, MBG, ST-segment resolution, and left ventricular systolic function.
Similar content being viewed by others
Background
Primary percutaneous coronary intervention (PPCI) is a gold standard treatment for patients with ST-segment elevation myocardial infarction (STEMI) [1, 2]. PPCI is superior to fibrinolysis in improving epicedial flow and myocardial reperfusion and myocardial blush grade with more patency of the infarct-related artery, faster and more complete resolution of ST-segment elevation. In aggregate, these benefits translate into reduced infarct size and improved survival [3]. Fibrinolysis has higher rate of reocclusion and reinfection [4].
Value of thrombus aspiration (TA) depends on decreasing distal embolization and protection of microcirculation, which frequently occurs in patients presenting with ST-elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI) [3, 5,6,7,8,9,10,11]. In spite of its appealing conceptual value, there are conflicting data yielded in randomized clinical trials may be due to differences in clinical presentation of patients included in different studies and heterogeneity in angiographic characteristics mainly inclusion of both occluded and patent culprit vessels and different grade of thrombus burden at the time of the initial coronary angiography [12,13,14,15,16,17,18,19,20,21,22,23,24].
Results of routine thrombus aspiration during primary PCI was disappointing and did not improve clinical outcomes. However, there is remaining uncertainty about the potential benefit in those patients with high thrombus burden, where there is a biological rationale for greater benefit [25].
Aim of study
The aim of this study is to evaluate the in-hospital and short-term outcome of using manual thrombus aspiration in STEMI patients undergoing primary PCI and showing large thrombus burden.
Methods
We enrolled 209 patients referred to coronary care unit within 12 h of chest pain with diagnosis of STEMI patients; their initial coronary angiography show totally occluded infarct-related artery with heavy thrombus burden. Patients were divided into two groups based on whether thrombus aspiration was attempted. This decision was left at the operator’s discretion.
Patients were divided into 2 groups: group (B) which included 73 patients, who had under-gone PTCA and manual thrombus aspiration followed by stent to culprit lesion, and group (A) which included 136 patients, who had undergone conventional PTCA and stent of culprit lesion within the period from November 2016 till July 2018. Patients had echocardiography on day 1 of MI and were followed up after 4 weeks for SWMA, estimated EF by Simpson technique; patients were followed up for 4 weeks for major adverse cardiac events (MACE). Patients with small thrombus burden were excluded from the study. All selected patients have been subjected to complete history taking, full clinical examination, Lab workup, including CBC, kidney function test, and cardiac biomarkers. Resting 12 lead ECG and full echocardiographic study. All the patients received acetylsalicylic acid, P2Y12 inhibitors, and UFH during the procedure. During the procedure, the culprit vessel was determined and if there was any other vessel involvement either for intervention in the same session or later on. Also, the thrombus grading scale as well as TIMI flow and MBG were evaluated pre- and post-PCI. For patients assigned to thrombus aspiration, guidewire placement was followed by Diver C thrombus aspiration catheter then stent placement at culprit lesion.
The Diver CE (Invatec, Brescia, Italy) is a rapid-exchange, 6-F compatible, and thrombus-aspirating catheter. It has a central aspiration lumen and a soft, flexible, 0.026-inch, non-traumatic tip with multiple holes (one large anterior and three smaller lateral ones) communicating with the central lumen. A 30-ml lower lock syringe is connected to the proximal hub of the central lumen for thrombus-aspiration [26].
Analytical statistics
-
1-
Chi-square test was used to examine the relationship between two qualitative variables but when the expected count is less than 5 in more than 20% of the cells; Fisher’s exact test was used.
-
2-
Independent sample t test was used to assess the statistical significance of the difference of a parametric variable between two independent means of two study groups.
P value: Level of significance
-
P > 0.05: non significant (NS)
-
P < 0.05: significant (S)
-
P < 0.01: highly significant (HS)
Results
1—Baseline clinical features (Table 1)
2—Location of myocardial infarction (Table 2)
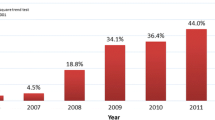
3—Type of used stent (Table 3) (Fig. 1)
4—Relation between the 2 groups, regarding primary endpoints MACE (mortality, non-fatal MI, stroke, target vessel revascularization) (Table 4) (Fig. 2)
5—Comparison between the 2 groups, regarding secondary end-points (Table 5)
There was a statistical significant difference between 2 groups regarding TIMI flow, MBG, and ST-segment resolution. TIMI III flow had been achieved in 94.5% of group (B) but had been achieved in 80.1% of group (A). MBG 3 had been achieved in 82.2% of group (B) but had been achieved in 58.1% of group (A). ST-segment resolution > 70% had been achieved in 97.2% of group (B) that had been achieved in 86.8% in group (A).
6—Comparison between the two groups, regarding follow-up after 1 month: There were statistical significant results regarding clinical follow-up, while no adverse outcome had developed in 91.8% of group (B), no adverse outcome had developed in 77.9% of group (A). Mortality had occurred in 6.8% of group (B), but in 21.6% of group (A). Stroke had occurred in 1 case of group (A). Non-fatal MI had occurred in 1 case of group (B).
7—Comparison between the 2 groups, regarding follow-up echocardiography data: Improvement in left ventricular systolic function detected in day 1 of MI and after 1 month follow-up, there were highly significant results in both groups (A) and (B). In group (B), LVEF% had improved from 42.08%+/−8.7 to 51.68%+/−9.5, but had improved from 41.57%+/−9.34 to 46.74%+/−9.38 in group (A) (Table 6).
Discussion
Management of STEMI has been developed over the last years and primary percutaneous coronary intervention, where available, has become the therapy of choice. However, there are some obstacles to achieve successful myocardial reperfusion. One of the most famous obstacles is high thrombus burden which is present in a significant proportion of patients, wire manipulation and balloon dilatation and stent placement in culprit vessel with high thrombus burden cause distal embolization of thrombus particles and atherosclerotic plaque debris impaired myocardial perfusion resulting in poorer short- and long-term outcomes, including heart failure and death.
Management of culprit lesions with high thrombus burden including both pharmacological and mechanical measures to decrease distal embolization and microvascular obstruction these measures includes pharmacological measures, such as adequate antiplatelet therapy, glycoprotein IIb/IIIa antagonists, and coronary vasodilators as adenosine, adrenalin, and verapamil, mechanical evacuation of thrombus as devices dedicated to evacuating or trapping thrombus during intervention to reduce the risk of distal embolization during percutaneous coronary intervention.
One of the most appealing devices dedicated to evacuate thrombi from culprit artery is thrombus aspiration (TA) devices which have been proposed as adjunctive therapy to protect microcirculation from distal embolization [3, 11].
Thrombus aspiration has appealing conceptual value but also conflicting results yielded in randomized clinical trials so this therapy receives only a class of recommendation IIa, level of evidence B according to European Guidelines 2008 [24], and class III recommendation in European Guidelines 2017.
A number of small-scale or single-center studies and one meta-analysis of 11 small trials suggested that there could be benefits from routine manual thrombus aspiration during primary PCI [27].
One of the earlier trials is REMEDIA trial which was published in JACC 2005; this trial randomized 100 consecutive patients with STEMI to either standard PCI or PCI with manual thrombus aspiration. Primary endpoints of the study were ST-segment resolution (STR) ≥ 70% and post-procedural rates of myocardial blush grade (MBG) ≥ 2 and which were respectively, 44.9% and 68.0% in the thrombus-aspiration group compared with 36.7% and 58.0% in the standard PCI group. Moreover, the rate of patients achieving both the angiographic and electrocardiographic (ECG) criteria of optimal reperfusion was significantly higher in the thrombus-aspiration group compared with standard PCI: 46.0% versus 24.5% [28].
TAPAS trial which was a relatively large randomized trial; it was published in 2008 randomized 1071 STEMI patients assigned for primary PCI to the thrombus-aspiration group or the conventional-PCI group before undergoing coronary angiography. A myocardial blush grade of 0 or 1 occurred in 26.3% of the patients in the conventional-PCI group and in 17.1% of those in thrombus-aspiration group (P < 0.001). Complete resolution of ST-segment elevation occurred in 44.2% and 56.6% of patients, respectively (P < 0.001). At 30 days, the rate of death in patients with a myocardial blush grade of 0 or 1, 2, and 3 was 5.2%, 2.9%, and 1.0%, respectively (P = 0.003), and the rate of adverse events was 14.1%, 8.8%, and 4.2%, respectively (P < 0.001) [22].
Recently, two large randomized controlled trials > 7000 patients, which were adequately powered to detect value of routine manual thrombus aspiration in PPCI versus conventional primary PCI procedure and influence the guidelines recommendation, unfortunately, both trials showed no benefit on clinical outcomes of routine aspiration strategy. Also, there are safety concerns that emerged in the trial of routine aspiration thrombectomy with PCI versus PCI alone in patients with STEMI (TOTAL) trial (n = 10 732), with an increase in the risk of stroke [29].
We suppose these disappointing results may be yielded by two main causes, the first cause is heterogeneity of patients and wide scale of thrombus burden and heterogeneity of coronary anatomy, second cause is concept of routine use of thrombus aspiration. So we think if we limiting the use of thrombus aspiration device to patients with totally occluded culprit artery by large thrombus burden, we may get the expected benefits of this technique.
In the subgroup of TOTAL trial with high thrombus burden [TIMI (thrombolysis in myocardial infarction) thrombus grade 3], thrombus aspiration was associated with fewer cardiovascular deaths [170 (2.5%) vs. 205 (3.1%); hazard ratio (HR) 0.80, 95% confidence interval (CI) 0.65–0.98; P = 0.03] and with more strokes or transient ischemic attacks [55 (0.9%) vs. 34 (0.5%); odds ratio 1.56, 95% CI 1.02–2.42, P = 0.04]. However, the interaction P values were 0.32 and 0.34, respectively.
In the taste and TOTAL trials, 1–5% of randomized patients crossed over from PCI alone to thrombus aspiration. Based on these data and the results of a recent meta-analysis, the last European guidelines for the management of STEMI patients which was published in 2017 stated that routine thrombus aspiration is not recommended, but in cases of large residual thrombus burden after opening the vessel with a guidewire or a balloon, thrombus aspiration may be considered [30].
In our study, we tried to evaluate the rule of thrombus aspiration therapy in improving the outcome of primary PCI in STEMI patients with high thrombus burden. Patients were divided into 2 groups: group (B) which included 73 patients, who had undergone PTCA and manual thrombus aspiration followed by stent to culprit lesion when needed, and group (A) which included 136 patients, who had undergone conventional PTCA and stent of culprit lesion within the period from November 2016 till July 2018.
There was no significant difference between both groups as regard clinical background or location of myocardial infarction. The number of needed stents in the thrombus aspiration group is significantly less than conventional PCI group.
Cardiovascular mortality was significantly lower in the thrombus aspiration group that had occurred in 2.7% of patients, but in 11.8% of conventional PCI group. There was a non-significant difference between the two groups as regard other complication (stroke, non-fatal MI, and target vessel revascularization).
There was a statistical significant difference between 2 groups regarding TIMI flow, MBG, ST-segment resolution. TIMI III flow had been achieved in 94.5% of the thrombus aspiration group but had been achieved in 80.1% of conventional PCI group. MBG III had been achieved in 82.2% of the thrombus aspiration group but had been achieved in 58.1% of the conventional PCI group. ST-segment resolution > 70% had been achieved in 97.2% of thrombus aspiration group that had been achieved in 86.8% in conventional PCI group.
After 1 month of primary PCI, while no adverse outcome had developed in 91.8% of the thrombus aspiration group and 77.9% of conventional PCI group. Mortality had occurred in 6.8% of thrombus aspiration group significantly less than conventional PCI group (21.6%). Stroke had occurred in 1 case of conventional PCI group. Non-fatal MI had occurred in 1 case of the thrombus aspiration group.
Conclusion
Our trial concluded that thrombus aspiration therapy improves outcome of primary PCI in STEMI patient with high thrombus burden without significant increase in the incidence of stroke and must be considered in selected patients with high thrombus burden.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PCI:
-
Percutaneous coronary intervention
- PTCA:
-
Percutaneous transluminal coronary intervention
- STEMI:
-
ST elevation myocardial infarction
- CCU:
-
Coronary care unit
- TIMI flow:
-
Thrombolysis in myocardial infarction flow
- MBG:
-
Myocardial blush grade
- TA:
-
Thrombus aspiration
- SWMA:
-
Segmental wall motion abnormality
- CBC:
-
Complete blood picture
- UFH:
-
Unfractionated heparin
- BW:
-
Body weight
- BMI:
-
Body mass index
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- IHD:
-
Ischemic heart disease
- MI:
-
Myocardial infarction
- BMS:
-
Bare metal stent
- DES:
-
Drug-eluting stent
References
Windecker S, Kolh P, Alfonso F et al (2014) ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). EuroIntervention 10(2015):1024–1094
O’Gara PT, Kushner FG, Ascheim DD et al (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61:e78–e140
Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361:13–20
Andersen HR, Nielsen TT, Rasmussen K et al (2003) A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 349:733–742
Antman EM, Anbe DT, Armstrong PW et al (2004) ACC/AHA guidelines for the management of patients with ST elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation 110:e82–e292
Topol EJ, Yadav JS (2000) Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation 101:570–580
Henriques JP, Zijlstra F, Ottervanger JP et al (2002) Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J 23:1112–1117
van’t Hof AW, Liem A, de Boer MJ et al (1997) Clinical value of 12-lead electrocardiogram after successful reperfusion therapy for acute myocardial infarction. Zwolle Myocardial infarction Study Group. Lancet 350:615–619
van’t Hof AW, Liem A, Suryapranata H et al (1998) Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation 97:2302–2306
McLaughlin MG, Stone GW, Aymong E et al (2004) Prognostic utility of comparative methods for assessment of ST segment resolution after primary angioplasty for acute myocardial infarction: the controlled abciximab and device investigation to lower late angioplasty complications (CADILLAC) trial. J Am Coll Cardiol 44:1215–1223
Costantini CO, Stone GW, Mehran R et al (2004) Frequency, correlates, and clinical implications of myocardial perfusion after primary angioplasty and stenting, with and without glycoprotein IIb/IIIa inhibition, in acute myocardial infarction. J Am Coll Cardiol 44:305–312
Napodano M, Pasquetto G, Sacca S et al (2003) Intracoronary thrombectomy improves myocardial reperfusion in patients undergoing direct angioplasty for acute myocardial infarction. J Am Coll Cardiol 42:1395–1402
Antoniucci D, Valenti R, Migliorini A et al (2004) Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol 93:1033–1035
Burzotta F, Trani C, Romagnoli E et al (2005) Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus aspiration in primary and rescue angioplasty (REMEDIA) trial. J Am Coll Cardiol 46:371–376
Stone GW, Webb J, Cox DA et al (2005) Distal microcirculatory protection during percutaneous coronary intervention in acute ST segment elevation myocardial infarction: a randomized controlled trial. JAMA 293:1063–1072
Lefevre T, Garcia E, Reimers B et al (2005) X sizer for thrombectomy in acute myocardial infarction improves ST segment resolution: results of the X sizer in AMI for negligible embolization and optimal ST resolution (X AMINE ST) trial. J Am Coll Cardiol 46:246–252
Silva-Orrego P, Colombo P, Bigi R et al (2006) Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEARMI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study. J Am Coll Cardiol 48:1552–1559
De Luca L, Sardella G, Davidson CJ et al (2006) Impact of intracoronary aspiration thrombectomy during primary angioplasty on left ventricular remodelling in patients with anterior ST elevation myocardial infarction. Heart 92:951–957
Ali A, Cox D, Dib N et al (2006) Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30 day results from a multicenter randomized study. J Am Coll Cardiol 48:244–252
Chevalier B, Gilard M, Lang I et al (2008) Systematic primary aspiration in acute myocardial percutaneous intervention: a multicentre randomised controlled trial of the export aspiration catheter. EuroIntervention 4:222–228
Javaid A, Siddiqi NH, Steinberg DH et al (2008) Adjunct thrombus aspiration reduces mortality in patients undergoing percutaneous coronary intervention for ST elevation myocardial infarction with high risk angiographic characteristics. Am J Cardiol 101:452–456
Svilaas T, Vlaar PJ, van der Horst IC et al (2008) Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med 358:557–567
Vlaar PJ, Svilaas T, van der Horst IC et al (2008) Cardiac death and reinfarction after 1 year in the thrombus aspiration during percutaneous coronary intervention in acute myocardial infarction study (TAPAS): A 1 year follow up study. Lancet 371:1915–1920
Sardella G, Mancone M, Bucciarelli Ducci C et al (2009) Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct related artery during primary percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol 53:309–315
Sanjit S, Cairns JA, Lavis S et al (2018) Thrombus aspiration in patients with high thrombus burden in the TOTAL trial. J Am Cardiol 72(14):1589–1596
Burzotta F, Trani C, Romagnoli E et al (2006) A pilot study with a new, rapid-exchange, thrombus-aspirating device in patients with thrombus-containing lesions: the Diver CE study. Catheter Cardiovasc Interv 67(6):887–893
Burzotta F, De Vita M, Gu YL, Isshiki T, Lefevre T, Kaltoft A, Dudek D, Sardella G, Orrego PS, Antoniucci D, De Luca L, Biondi-Zoccai GG, Crea F, Zijlstra F (2009) Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-datapooledanalysisof11trials. Eur Heart J 30(18):2193–2203
Francesco Burzotta, Carlo Trani, Enrico Romagnoli, Mario Attilio Mazzari, Antonio Giuseppe Rebuzzi, Maria De Vita, Barbara Garramone, Floriana Giannico, Giampaolo Niccoli, Giuseppe G.L.Biondi-Zoccai, Giovanni Schiavoni, Rocco Mongiardo, Filippo Crea. https://doi.org/10.1016/j.jacc.2005.04.057
Jolly SS, Cairns JA, Yusuf S, Meeks B, Gao P, Hart RG, Kedev S, Stankovic G, Moreno R, Horak D, Kassam S, Rokoss MJ, Leung RC, El-Omar M, Romppanen HO, Alazzoni A, Alak A, Fung A, Alexopoulos D, Schwalm JD, Valettas N, Dzavik V, TOTAL Investigators (2015) Stroke in the TOTAL trial: a randomized trial of routine thrombectomy vs. percutaneous coronary intervention alone in ST elevation myocardial infarction. Eur Heart J 36(35):2364–2372
Jolly SS, James S, Dzavik V, Cairns JA, Mahmoud KD, Zijlstra F, Yusuf S, Olivecrona GK, Renlund H, Gao P, Lagerqvist B, Alazzoni A, Kedev S, Stankovic G, Meeks B, Frobert O (2017) Thrombus aspiration in ST-segment-elevation myocar-dial infarction. An individual patient meta-analysis: thrombectomy Trialists Collaboration. Circulation 135(2):143–152
Acknowledgements
All members of the Cardiac Cath Lab of Ain Shams University specially nurses and technicians.
Funding
The authors did not receive any specific funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the research equally. All authors read and approved the final manuscript. MN select patients according inclusion criteria, take history, perform general, and local physical examination. EME revised patient’s data and coronary intervention details. RR revised patient’s data and coronary intervention details. AN supervise and coordinate the work and revise final edition of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval of the Ain Shams University ethical committee and approval of coronary intervention scientific group of cardiology department faculty of medicine Ain Shams University was obtained according to the ethical guidelines of the 1975 Declaration of Helsinki as revised in 2008. The committee’s reference number is not applicable. Informed written or oral approval consent was obtained from all patients included in this research.
Consent for publication
Written informed consent for publication was obtained.
Competing interests
The authors report no financial relationships or conflicts of interest regarding the content herein.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elfekky, E.M., Penjameen, M.N., Nassar, A.I. et al. Outcome of manual thrombus aspiration for patients undergoing primary PCI for acute STEMI showing large thrombus burden. Egypt Heart J 73, 8 (2021). https://doi.org/10.1186/s43044-020-00122-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-020-00122-9