Abstract
Background
Men with non-obstructive azoospermia constitute a challenging subgroup of male infertility patients in whom a genetic cause of defective spermatogenesis may be a contributing factor. The aim of this prospective observational cohort study was to determine whether assessment of meiotic nuclear division 1 (MND1) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) gene expression (MND1/GAPDH) in testicular tissue could be a prognostic indicator for sperm retrieval and ICSI outcome in patients with non-obstructive azoospermia. The study participants underwent clinical evaluation, conventional semen analysis, serum follicular stimulating hormone (FSH), testosterone assay, scrotal ultrasound examination, microsurgical testicular sperm extraction (mTESE), and assessment of MND1/GAPDH gene expression levels in testicular tissue via quantitative polymerase chain reaction (qPCR) techniques.
Results
The MND1/GAPDH level was associated with the likelihood of identifying sperm in testicular biopsies (odds ratio (OR) 1.25, 95% confidence intervals (CI) 1.14 to 1.34, p < 0.0001), which was confirmed by the pairwise comparison of high vs. low levels of MND1/GAPDH (OR 5.34, 95% CI 1.97 to 13.16, p = 0.0006). The level of FSH was inversely associated with a lower chance of finding sperm (OR 0.37, 95% CI 0.20 to 0.65, p = 0.001). Compared with small testicular volume, normal volume was inversely associated with the chance of sperm presence (OR 0.16, 95% CI 0.06 to 0.47, p = 0.0002). However, there was no correlation between MND1/GAPDH levels and ICSI outcome.
Conclusion
Gene expression analysis to predict the likelihood of sperm retrieval following mTESE in patients with non-obstructive azoospermia provides a new avenue for future research, diagnosis and treatment of male factor infertility. Before its wider clinical application, however, this proof-of-concept should be tested in a large multinational, multicenter observational study.
Similar content being viewed by others
Introduction
Male factor infertility is an ongoing dilemma that has been partially addressed by assisted reproduction. However, azoospermia, which affects around 10% of infertile males, remains a challenge and requires further understanding to support treatment optimization (World Health Organization). For example, identifying genetic or epigenetic factors linked to azoospermia could lead to better patient care [1], allowing researchers to investigate whether specific gene expression patterns are linked to sperm presence and concentration in testicular tissue [2, 3], or the outcome of intracytoplasmic sperm injection (ICSI).
Testicular tissue is composed of many cell types, providing a supportive environment for male germ cell development [4,5,6]. It follows, then, that a testicular biopsy with a simple histological score for spermatogenesis can only provide limited prognostic information in certain patients, such as those with non-obstructive azoospermia who constitute a heterogeneous group with wide range of spermatogenic defects [7, 8]. Despite advances in diagnostic tools and the use of advanced surgical sperm retrieval techniques such as microsurgical testicular sperm extraction (mTESE), there is not yet a marker for quantitative and qualitative prediction of the presence of sperm, nor of ICSI outcome up to the delivery of healthy baby. Therefore, it could be of value to study the correlation between spermatogenesis and fertility outcomes with gene expression patterns.
Attempts to identify changes in gene expression associated with male factor infertility have previously been undertaken [9,10,11,12], with multiple gene clusters likely related to defects in spermatogenesis being identified [10]. Of these genes, 47 were differently expressed in mice, while 19 genes involved in DNA repair, spermatogenesis, and other crucial biological processes, had abnormal expression patterns in the human [13]. Genes related to human spermatogenesis include meiotic nuclear division 1 (MND1), spermatogenesis associated 22 (SPATA22), glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and acrosin (ACR) [5]. MND1 is expressed before meiotic division and its corresponding proteins are involved in meiotic progression during spermatogenesis, while GAPDH is highly expressed in haploid sperm and can affect sperm function [5]. Therefore, investigation of the expression patterns of MND1 and its housekeeping gene GAPDH in patients undergoing TESE could provide prognostic information related to the likelihood of sperm retrieval and on the embryological and clinical outcomes with ICSI in patients with sperm retrieved.
Materials and methods
Study design
This prospective cohort study was conducted at the IbnSina IVF Centre, Sohag, Egypt, in collaboration with the Zoology Department, Faculty of Science, Assiut University, and the Dermatology & Andrology Department, Faculty of Medicine, Assiut University. The study was prospectively approved by the Ethics Review Board of Assiut University (no. 17100808; 18 August 2019). Eligible participants gave written informed consent for participation after receiving detailed explanations on the study. The study had no interventions or assignment to any study arms.
Study participants
Men with non-obstructive azoospermia were eligible if they were aged between 25 and 55 and were undergoing a mTESE procedure. They were invited to participate in the study if they had a clinical diagnosis of non-obstructive azoospermia. The exclusion criteria were presence of a varicocele, exposure to reproductive toxicants, or having a systemic disease known to affect spermatogenesis. When sperm were identified in the testicular tissues, they were retrieved for use in an ICSI cycle. Women were eligible provided they were 18 to 40 years of age and were undergoing an ICSI attempt. Causes of infertility were male factor only or combined with female factor. Surgically retrieved sperm, either fresh or frozen-thawed, were suitable for the study. Patients who refused to take part in the study were deemed ineligible. Women with thin endometrium (≤ 7 mm), uterine anomalies, untreated hydrosalpinx or a severe medical condition were accounted for during the study.
Initial evaluation of male patients
A clinical history was taken for all eligible men. A genital and scrotal ultrasound examination was performed to measure testicular size and rule out any pathologies. Men were diagnosed as being azoospermic if no spermatozoa were found in three conventional semen analyses that included centrifugation and examination of the pellet according to the WHO protocol (WHO 2010). Each man’s serum levels of follicular stimulating hormone (FSH) and testosterone were determined by automated immunoassay assay (MINI VIDAS®, Biomerieux, France).
mTESE procedure
All trials for sperm extraction were performed under surgical microscopy by microsurgical testicular sperm extraction (mTESE) as described earlier [14]. Briefly, under surgical microscopy (MS-1600, Medical Microsurgery, Medical sources Limited Co.) and local anesthesia, we began with the testis that had the larger volume, otherwise the right testis. The testis was visualized via a scrotal midline incision, followed by transverse incision of the tunica vaginalis. Using a magnification power of × 20–50, the thicker and more opaque seminiferous tubules were identified and biopsied for determination of sperm presence.
In a 30-mm Petri dish (Falcon, BD, USA), testicular tissues were washed in 3 mL Global Total HEPES medium (LifeGlobal, CooperSurgical, USA), then transferred to a clean dish containing 3 mL Global Total HEPES medium and dissected with small scissors, followed by vigorous mechanical milking and mincing of the tissue with two needles of insulin syringes. The dish contents were then examined under an inverted microscope (× 40, Olympus IX 71, Japan) at room temperature. The surgical procedure was halted as soon as sperm were detected. If sperm were not detected, further biopsies from a different area of the testis, and from the other testis underwent the same preparation and examination procedures.
The sperm-positive biopsies were minced, and the sperm suspension was separated from the tissue remnants using a glass Pasteur pipette. The sperm suspension was then diluted with Sperm CryoProtec medium (Nidacon, Mölndal, Sweden) in a 2:1 ratio before being cryopreserved in cryovials according to the manufacturer’s protocol. A small fraction of the cryopreserved processed testicular tissue from each biopsy was retained for later gene expression analysis [15], while the rest of the sperm remained frozen until they were thawed for use in an ICSI cycle.
Part of the testicular tissue was fixed in Bouin’s solution for histopathological examination in all patients.
Testicular gene expression analysis
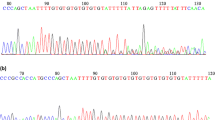
To isolate the RNA, all tissue samples from each patient were treated with Qiazol lysis reagent with RNase inhibitor (Qiagen, Germany). The redissolved RNA in RNase free water was then cleaned using a miRNeasy Mini kit (Qiagen, Germany) to remove all contaminants, inhibitors, and residuals before processing. This step was followed by cDNA synthesis for each extracted sample by high-capacity cDNA reverse Transcription with RNase inhibitor kit (Applied Biosystems, UK)
Expression level of the MND1 target gene was measured using SYBR Green-based real-time PCR, and consequent relative quantification analysis with the aid of GAPDH as a housekeeping gene on the Step-One real time PCR system (Applied Biosystems, UK). The 20 μL PCR reaction mixture for the target gene and the corresponding housekeeping gene for each sample included 15 μL master mix with 9 μL PCR-grade water, 1 μL forward primer for each parameter and the housekeeping gene (20 pmol/μL), 1 μL reverse primer for each parameter and the housekeeping gene (20 pmol/μL), 4 μL ready to use SYBR Green universal master mix (Applied Biosystems, UK), and 50 ng cDNA. The thermal profile was as follows: initial denaturation at 95 °C for 10 min, followed by 45 cycles of amplification, starting with denaturation at 95 °C for 10 s, annealing at 66 °C for 20 s and extension at 72 °C for 25 s. Following amplification, an extra cycle of melting curve analysis was done for product characterization by heating the reaction mixture from 65 °C to 95 °C at a rate of 0.2 °C/s. The Step-One real time PCR system software automatically calculated the gene expression values by relative quantitative analysis.
ICSI protocol
Stimulation cycles were controlled with either GnRH agonist (Decapeptyl 0.1 mg, Ferring) started on day 21 of the preceding cycle, or GnRH antagonist (Cetrotide® 0.25 mg, Merck Serono) started on stimulation cycle day 6. For ovarian stimulation, patients received 150–300 IU rFSH (Gonal-F, Merck Serono) and hMG (Menogon, Ferring) in a 2:1 ratio, with the dose adjusted according to the response. Oocyte retrieval took place 37 h after the GnRh agonist (Decapeptyl 0.1 mg, Ferring) or hCG (500 g, Ovitrelle, Merck Serono) maturation trigger was given. Follicles were aspirated into 14 ml tubes containing 1 ml Global HEPES Total medium (LifeGlobal, USA), held in a 37 °C tube warmer (IVFtech, Denmark).
Oocytes were denuded 39 h after the hCG trigger, in Global Total HEPES medium (LifeGlobal) containing 40 IU hyaluronidase (Irvine, USA), using a 170-μm denuding pipette (Cook, USA). Oocyte denudation was performed at 37 °C. All MII oocytes underwent ICSI in Global Total HEPES (LifeGlobal) immediately post denudation.
All cryopreserved testicular samples were thawed as per our standard protocol [16]. Briefly, samples were removed from cryostorage and incubated in a 37 °C water bath for 20 min, followed by centrifugation and washing twice in PureSperm Wash media (Nidacon, Mölndal, Sweden) at room temperature. The washed pellet was suspended in 0.5 mL PureSperm Wash supplemented with 2 mg/mL pentoxifylline 15 min before use. Sperm were then washed to remove the pentoxifylline (Sigma) before use in ICSI. Search dishes for sperm contained 5 × 20 μl droplets surrounding 2 × 2 μl PVP droplets. We chose motile sperm (if available) with normal morphology, or as close to normal morphology as possible, for ICSI using an inverted microscope (40X lens, IX 71, Olympus, Japan). As per our standard protocol, using a Sunlight injection pipette (Sunlight, USA), we deposited each immobilized spermatozoon into the cytoplasm after mechanical piercing of the zona pellucida and cytoplasmic membrane [17].
From days 0 to 5 or 6 after injection, all injected oocytes were cultured in Global Total medium (LifeGlobal) in a microdroplet dish (Vitrolife), three per 20 μl droplet, overlaid with 5 ml oil (NidOil, Nidacon, Mölndal, Sweden), without medium renewal. A fertilization check and embryo grading were performed on days 1, 3, and 5 of culture as per the Istanbul Consensus [18]. Oocyte and embryo culture was performed at 37 ± 0.1 °C in a Minc-1000 incubator (Cook, USA) supplied with premixed gas (7.5% CO2, 5% O2 and 87.5% N2) to achieve pH 7.25 ± 0.02. One to two blastocysts were transferred to each woman under ultrasound guidance using a Sydney IVF embryo transfer catheter (Cook, USA). All women received intramuscular progesterone (100 mg, Prontogest, IBSA) started from the day after oocyte retrieval until the 12th week of gestation or a negative pregnancy test.
Outcomes
The non-obstructive azoospermia is defined as the absence of spermatozoa in the ejaculate due to lack of production of mature spermatozoa. The primary endpoint of this study was presence or absence of sperm after the mTESE procedure, defined as the detection of at least one spermatozoon using an inverted microscope (× 40 lens, IX 71, Olympus, Japan). Secondary endpoints for cases with sperm retrieved and used in a subsequent ICSI cycle included the rates of fertilization (oocytes with two pronuclei as a function of the number of MII oocytes injected), blastocyst formation (the proportion of oocytes with two pronuclei that had formed a blastocyst by days 5/6), and ongoing pregnancy (fetal heartbeat at ≥ 12 weeks of gestation per oocyte retrieval).
Statistical analysis
Baseline characteristics were summarized as mean and standard deviations (SDs), median and interquartile range, and number with percentages, where appropriate. We performed all comparisons using the cluster bootstrap regression model. For the ICSI cycles, we analyzed the embryo development at the per woman and per oocyte level. We performed a backward comparison of the regression model to identify the confounders to be included. We found the model analyzing embryo development and clinical pregnancy should be adjusted for maternal age as covariate. The model comparing the presence or absence of sperm in testicular biopsies was adjusted for the paternal age as covariate after standardization. At the per woman level, fertilization and embryo development were compared using Poisson regression analysis, summarizing the effect size as relative risk (RR) with 95% confidence intervals (CIs). At the oocyte level, fertilization and embryo development were compared using logistic regression, summarizing the effect size as odds ratio (OR) with 95% confidence intervals (CIs). We used the R Statistical Package [19] for all analyses.
Results
Between 25 August 2019 and 5 November 2019, a total of 217 azoospermic men received detailed information on the study and were screened for non-obstructive azoospermia. Of these men, 193 were eligible for inclusion in the study, with 106 undergoing mTESE and completing the study. Sperm were recovered from 59 participants.
Male age, female age, testosterone level, and normal testicular volume were comparable between the sperm-positive and negative groups (Table 1). In contrast, the level of gene expression—either numerical (mean difference [MD] 10209, 95% CI 6705 to 13712) or categorical including the high (70% vs 30%) and moderate (72% vs 28%) subgroups—and the proportion of small for testicular size (81% vs 19%) were higher in patients from whom sperm were recovered. Patients who had sperm with mTESE had significantly lower FSH levels (MD – 8, 95% CI – 11.7 to – 4.3).
The level of gene expression had a strong asymmetrical distribution, needing logarithmic transformation before being entered as predictor into a cluster-bootstrap logistic regression. The log transformed level of gene expression was a strong predictor for finding sperm in a testicular biopsy (odds ratio [OR] 1.25, 95% CI 1.14 to 1.34, p < 0.0001: Table 2). When transformed into a categorical variable, the pairwise comparison showed that sperm retrieval was higher in patients with high and moderate levels of gene expression (OR 5.34, 95% CI 1.97 to 13.16, p = 0.0006 and OR 7.04, 95% CI 1.47 to 24.36, p = 0.005) compared to those with a low level of gene expression. However, there was no difference between high versus moderate gene expression level in predicting the likelihood of retrieving sperm from a testicular biopsy (p = 0.82). Normal testicular size and high FSH level were negative predictors for testicular sperm retrieval in patients with non-obstructive azoospermia (OR 0.16, 95% CI 0.06 to 0.47, p = 0.0002 and OR 0.37, 95% CI 0.20 to 0.65, p = 0.001), while testosterone level and male age were not correlated with sperm retrieval (both p = 0.12). For the positive sperm group, the level of log transformed gene expression and the pairwise comparison of its categorical conversion did not show any relationship with testicular volume or sperm concentration (all p > 0.05; Table 2). Similarly, there was no correlation between gene expression levels and male age, FSH, or testosterone levels (all p > 0.05; Table 2).
Likely due to the pilot sample size, there was no correlation of gene expression level with the rates of fertilization, blastocyst utilization, good concentration of sperm, or ongoing pregnancy (all p > 0.05; Table 3).
Discussion
The lack of a predictive method for the prognosis of azoospermic men is a compelling problem. In this study, we found a positive correlation between the expression levels of MND1/GAPDH and the presence of sperm in the testicular tissue of patients with non-obstructive azoospermia. This could have the potential of transforming the traditional testicular biopsy by introducing a new test to better understand the genes contributing to azoospermia. Despite this promising result, our study did not identify any prognostic value on clinical outcomes following the use of these sperm, likely due to the sample size and broad endpoints.
MND1 and GAPDH were chosen for our study because of the theoretical difference in their expression in azoospermic men. The results of the present study supported this concept, with different levels of MND1/GAPDH found in testicular biopsies. This could potentially offer a diagnostic alternative to inaccurate clinical and laboratory hormonal predictors of spermatogenesis. The two genes in our study were investigated previously in a small retrospective study of gene expression and IVF outcomes [5], although MND1 was included in a panel and not assessed individually. Our study was more focussed and evaluated the MND1 gene expression level on testicular function.
We categorized the level of gene expression as high, moderate, or low, and found that high and moderate levels of expression predicted the successful retrieval of sperm from testicular biopsies, compared to samples with low expression levels. This provided further validation for the concept of gene expression analysis as a predictor of sperm retrieval.
Despite previous reports linking positive testicular biopsy results to normal testicular size [20], in our study average testicular volume was negatively correlated with the presence of sperm while small testicular volume was positively correlated (Table 1). This suggests that in non-obstructive azoospermia, we cannot predict testicular function by measuring testicular volume. Non-obstructive azoospermia is likely to have deeper underlying causes, with gene expression being one of them. More mechanistic research is needed to figure out why testicular volume does not correlate with function.
FSH level was another predictor of locating sperm in testicular biopsies (Table 1). Together, we found that a combination of high FSH, a low level of gene expression, and normal testicular volume in men with non-obstructive azoospermia indicates a poor prognosis for sperm recovery, although we cannot rule out the possibility of finding sperm in further testicular biopsies after medical or hormonal therapies or with future gene therapy [21,22,23].
Our study accounted partially for the small sample size by using the bootstrap approach with 5000 iterations to augment confidence in our findings. Although we were unable to establish any correlation between gene expression levels and pregnancy outcome, we cannot rule out that this was due to the small sample size. The post hoc power analysis for the ongoing pregnancy in our study was 12% at the 5% significance level, which is very low. This is in agreement with the very low power for the previous study that included these two genes along with another three [5]. This would suggest the need for a study with sample size of ~ 550 to be able to draw solid conclusions on likely clinical outcomes after ICSI. The same concept holds true for detecting differences in embryo development patterns.
Our study carried no extra risks for participants as they were already scheduled to undergo a micro-TESE procedure, irrespective of whether they were participating in the study. They chose to participate in this prospective observational study in the hope of gaining a better understanding of their own cases as well as of contributing to their peers’.
This study has some limitations. It included only two genes, based on the results from a previous pilot study [5]; however, we have proved the concept to support further research. Although next generation sequencing is currently the superior method for specific gene expression or whole exome sequencing, qPCR is a rapid, effective, less costly method with reasonable accuracy for testing the selected genes. Given the possibility of different gene expression across different populations, and as this study included only Egyptians, the generalizability of our findings needs to be investigated through a larger, multinational study.
This study also has some strengths, establishing a new, more advanced diagnostic and prognostic tool for non-obstructive azoospermia. The protocol used for surgical sperm retrieval along with the tissue handling across the study period was stringent. All samples were examined for the level of gene expression at the same time and in one laboratory with a high standard of professionalism, which is likely to have been reflected in the validity of the results obtained. Although the samples were identified as having been positive or negative for sperm, they were coded before being sent to the laboratory for gene expression, which would further increase the validity of the results.
The implication of this study is the justification of germ cell-specific gene expression analysis in testicular samples to improve the prediction of positive testicular biopsy outcome in non-obstructive azoospermia. Non-obstructive azoospermia is a complex pathophysiological state with altered gene expression in the testes. Understanding this process could ultimately lead to the identification of molecular markers of spermatogenesis.
In summary, the results of our study show that evaluation of the level of gene expression in patients with non-obstructive azoospermia can predict the chance of sperm retrieval during testicular sperm extraction. There was no increase in the incidence of adverse events in patients undergoing the gene expression analysis. Overall, our data support the addition of gene expression analysis to the current standard of care in patients with non-obstructive azoospermia. Our study may provide initial evidence to create a better understanding of the underlying genetic defects in non-obstructive azoospermia, and to support further mechanistic studies, which may in turn lead to the new treatment methods for patients with this type of male factor infertility.
Availability of data and materials
Data are available upon reasonable request.
Abbreviations
- MND1:
-
Meiotic nuclear division 1
- GAPDH :
-
Glyceraldehyde-3-phosphate dehydrogenase
- FSH:
-
Follicular stimulating hormone
- TESE:
-
Testicular sperm extraction
- qPCR:
-
Quantitative polymerase chain reaction
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ICSI:
-
Intracytoplasmic sperm injection
- SPATA22:
-
Spermatogenesis associated 22
- ACR:
-
Acrosin
- RR:
-
Relative risk
- MD:
-
Mean difference
References
Ghieh F, Mitchell V, Mandon-Pepin B, Vialard F (2019) Genetic defects in human azoospermia. Basic Clin Androl 29. https://doi.org/10.1186/s12610-019-0086-6
Vogt PH, Edelmann A, Kirsch S, Henegariu O, Hirschmann P, Kiesewetter F et al (1996) Human Y chromosome azoospermia factors (AZF) mapped to different subregions in Yq11. Hum Mol Genet 5:933–943. https://doi.org/10.1093/hmg/5.7.933
Feig C, Kirchhoff C, Ivell R, Naether O, Schulze W, Spiess A-N (2007) A new paradigm for profiling testicular gene expression during normal and disturbed human spermatogenesis. MHR Basic Sci Reprod Med 13:33–43. https://doi.org/10.1093/molehr/gal097
Stukenborg J-B, Kjartansdóttir KR, Reda A, Colon E, Albersmeier JP, Söder O (2014) Male Germ Cell Development in Humans. Horm Res Paediatr 81:2–12. https://doi.org/10.1159/000355599
Dorosh A, Tepla O, Zatecka E, Ded L, Koci K, Peknicova J (2013) Expression analysis of MND1/GAJ, SPATA22, GAPDHS and ACR genes in testicular biopsies from non-obstructive azoospermia (NOA) patients. Reprod Biol Endocrinol 11:42. https://doi.org/10.1186/1477-7827-11-42
Shima JE, McLean DJ, McCarrey JR, Griswold MD (2004) The murine testicular transcriptome: Characterizing gene expression in the testis during the progression of spermatogenesis. Biol Reprod 71:319–330. https://doi.org/10.1095/biolreprod.103.026880
Dohle GR, Elzanaty S, Van Casteren NJ (2012) Testicular biopsy: clinical practice and interpretation. Asian J Androl 14:88–93. https://doi.org/10.1038/aja.2011.57
Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G et al (2012) European association of urology guidelines on male infertility: The 2012 update. Eur Urol 62:324–332. https://doi.org/10.1016/j.eururo.2012.04.048
Ellis PJI, Furlong RA, Conner SJ, Kirkman-Brown J, Afnan M, Barratt C et al (2007) Coordinated transcriptional regulation patterns associated with infertility phenotypes in men. J Med Genet 44:498–508. https://doi.org/10.1136/jmg.2007.049650
Okada H, Tajima A, Shichiri K, Tanaka A, Tanaka K, Inoue I (2008) Genome-Wide Expression of Azoospermia Testes Demonstrates a Specific Profile and Implicates ART3 in Genetic Susceptibility. PLoS Genet 4:e26. https://doi.org/10.1371/journal.pgen.0040026
Calven P, Rolland AD, Jégou B, Pineau C (2010) Testicular postgenomics: targeting the regulation of spermatogenesis. Philos Trans R Soc B Biol Sci 365:1481–1500. https://doi.org/10.1098/rstb.2009.0294
Gatta V, Raicu F, Ferlin A, Antonucci I, Scioletti AP, Garolla A et al (2010) Testis transcriptome analysis in male infertility: new insight on the pathogenesis of oligo-azoospermia in cases with and without AZFc microdeletion. BMC Genomics 11. https://doi.org/10.1186/1471-2164-11-401
Rockett JC, Patrizio P, Schmid JE, Hecht NB, Dix DJ (2004) Gene expression patterns associated with infertility in humans and rodent models. Mutat Res Fundam Mol Mech Mutagen 549:225–240. https://doi.org/10.1016/j.mrfmmm.2003.11.017
Schlegel PN (1999) Testicular sperm extraction: Microdissection improves sperm yield with minimal tissue excision. Hum Reprod 14:131–135. https://doi.org/10.1093/humrep/14.1.131
Gianaroli L, Magli MC, Selman HA, Colpi G, Belgrano E, Trombetta C et al (1999) Diagnostic testicular biopsy and cryopreservation of testicular tissue as an alternative to repeated surgical openings in the treatment of azoospermic men, vol 14
Björndahl L, Mortimer D, Barratt CLR, Castilla JA, Menkveld R, Kvist U et al (2010) A practical guide to basic laboratory andrology. https://doi.org/10.1017/CBO9780511729942
Palermo G, Joris H, Devroey P, Van Steirteghem AC (1992) Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340:17–18. https://doi.org/10.1016/0140-6736(92)92425-F
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology (2011) Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Reprod BioMed Online 22:632–646. https://doi.org/10.1016/j.rbmo.2011.02.001
R Core Team (2019). R: A language and environment for statistical computing. Accessed 1 Apr 2019. 2019
Li H, Chen LP, Yang J, Li MC, Chen RB, Lan RZ et al (2018) Predictive value of FSH, testicular volume, and histopathological findings for the sperm retrieval rate of microdissection TESE in nonobstructive azoospermia: A meta-analysis. Asian J Androl 20:30–36. https://doi.org/10.4103/aja.aja_5_17
Vernaeve V, Tournaye H, Schiettecatte J, Verheyen G, Van Steirteghem A, Devroey P (2002) Serum inhibin B cannot predict testicular sperm retrieval in patients with non-obstructive azoospermia. Hum Reprod 17:971–976. https://doi.org/10.1093/humrep/17.4.971
Samli MM, Dogan I (2004) An artificial neural network for predicting the presence of spermatozoa in the testes of men with nonobstructive azoospermia. J Urol 171:2354–2357. https://doi.org/10.1097/01.ju.0000125272.03182.c3
Tsujimura A (2007) Microdissection testicular sperm extraction: Prediction, outcome, and complications. Int J Urol 14:883–889. https://doi.org/10.1111/j.1442-2042.2007.01828.x
Acknowledgements
We thank IbnSina IVF team for their support and thank Dr. Sharon Mortimer for critically appraising this manuscript.
Funding
The study received no funding.
Author information
Authors and Affiliations
Contributions
ME was the primary investigator, designed the study and drafted the manuscript. HO was the senior author and research leader. AK was senior author and critically reviewed the study protocol. EA was senior researcher and critically reviewed the manuscript. EAT was senior investigator and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Board of Assiut University (no. 17100808; 18 August 2019). All included participants provided written consent.
Consent for publication
All relevant bodies and authors gave consent for publication Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Emad, M., Omar, H.ED., Khalifa, AR. et al. Predicting the testicular function in non-obstructive azoospermia via targeted gene panel. Middle East Fertil Soc J 26, 43 (2021). https://doi.org/10.1186/s43043-021-00087-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-021-00087-y