Abstract
Background
Alopecia areata (AA) is a non-scarring hair loss condition that usually affects the scalp. The exact pathogenesis is poorly understood; however, multiple factors like genetics, environmental, psychological, and immunological factors may have a role. The purpose of this study was to look into possible links between the functional interleukin-4 (IL-4) gene intron 3 variable number of tandem repeats (VNTR) and TNF-(rs1799964) gene polymorphism and AA susceptibility. This case–control study consisted of 79 unrelated patients and 156 age- and sex-matched healthy individuals as a control group. The Severity of Alopecia Tool was used to assess the extent of hair loss from the scalp. Polymerase chain reaction (PCR) with specific primers was used to determine IL-4 gene 70-bp VNTR polymorphism while polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP) was used to investigate TNF-α (rs1799964) gene polymorphism.
Results
None of the selected polymorphisms for both genotypes and alleles had statistical significance when patients and controls were compared with each other (p-values for IL-4 VNTR were 0.11, 0.74, 0.052 and 0.27 and for TNF-α polymorphism was 0.71, 0.43, 0.65 and 0.55, respectively, for codominant, dominant, recessive and overdominant models of inheritance, respectively). Furthermore, the same results were retrieved when the genotypes were compared with the patient’s clinical and demographic data (p-value > 0.05).
Conclusion
The findings indicate that IL-4 VNTR intron 3 and TNF-α (rs1799964) gene polymorphisms are not linked to the development of AA in the Egyptian population.
Similar content being viewed by others
Introduction
Alopecia areata (AA) is a non-scaring inflammatory hair loss disorder and is considered the second most common cause of hair loss after androgenic alopecia [1]. The prevalence of AA is 0.1–0.2%, with a lifetime risk of 2% [2]. It affects the younger age group of the population. About 66% of patients are younger than 30 years old [3]. However, it rarely affects children under 3 years of age. Moreover, less than 20% of affected patients are older than 40 years [4]. According to a Chinese study, the male-to-female incidence ratio was 1.4:1 [5]. Another study showed a higher incidence in females, but this may be due to a high female concern regarding hair loss [6]. Female patients are diagnosed more commonly in adolescence and commonly have nail involvement and other autoimmune diseases, while male patients are mainly diagnosed in childhood. Generally, the earlier onset is associated with a more severe disease [7].
AA may begin with localized hair loss, commonly in the scalp, and then the condition may spread to involve the whole scalp (Alopecia Totalis) or the whole epidermis (Alopecia Universalis). The etiology of AA has been studied in numerous works, and various associations have been established. Autoimmune theory is one of the strongest suggestions, and this was supported by the association of AA with different autoimmune disorders like autoimmune thyroiditis [8], vitiligo [9], pernicious anemia [10], systemic lupus erythematosus (SLE) [11], and lichen planus [12]. Moreover, the overall increased risk of autoimmune disorders with AA is about 16% [13]. Genetic factors are also supposed to have a role in AA, based on different observational studies which found the incidence of AA in patients with a positive family history between 10 and 42% [14]. Different genes which involve the human leucocyte antigen (HLA) region, natural killer (NK) cells, and T regulatory cells have been studied in AA [15]. Environmental factors like vaccination, infection, stress, and diet may also have a role in AA [16].
In this study, we selected two cytokines, tumor necrosis factor-alpha (TNF-α) and interleukin-4 (IL-4) and investigated the association of their genetic polymorphisms and AA. TNF-α and IL-4 are secreted by T helper-1 (TH-1) cells and T helper-2 (TH-2) cells, respectively. The imbalance between TH-1 and TH-2 cells is one of the theories for the development of autoimmunity [17].
TNF-α is a major proinflammatory cytokine, synthesized in epidermal keratinocytes. It has different effects on hair: It inhibits proliferation, decreases the size of the hair follicle matrix, affects the keratinization of precortical cells, and inhibits melanogenesis by affecting the tyrosinase pathway [18]. Interleukin-4 (IL-4) is the major cytokine released from TH-2. It has anti-inflammatory and cytotoxic effects. Furthermore, it enhances IgE production. IL-4’s exact role in AA is not completely understood [19]. Polymorphisms of cytokine genes may influence gene transcription and cytokine production, hence influencing the development and progression of disease [20]. The purpose of this study is to look into the role of IL-4 gene intron 3 VNTR polymorphism and TNF-α (rs1799964) gene polymorphisms in the occurrence of AA.
Materials and methods
Subjects
This is a case–control study with 79 patients and 156 age and sex-matched healthy individuals as a control group. Both the patients and controls were recruited from the outpatient clinic of the Dermatology Department, Mansoura University, Egypt. The patients were either newly diagnosed or coming for regular follow-up and treatment.
The sample size was calculated with G*power software version 3.1.9.7 [21]. The minimal sample size was 64 subjects in each group. The software parameters were adjusted as follows: The power level was 0.8, the alpha error probability was 0.05 (two-tailed), and the effect size was 0.5. We intended to increase the sample size for both groups to avoid missing values.
The exclusion criteria involved any other skin disorders, other autoimmune diseases, and any other causes of hair loss, and patients who received topical or systemic medications at least 3 months before sample collection.
All patients were subjected to a complete history involving name, age, sex, occupation, special habits such as smoking, history of present illness (onset, course, and duration), past and family history of the same or similar conditions, or any other autoimmune disorder. Full dermatological examination to detect site and number of lesions. The loss of hair from scalp, eyebrows, eyelashes, beard, body, and nail changes were evaluated. Hair loss from the scalp was assessed using the Severity of Alopecia Tool (SALT) [22]. The severity of AA was graded as mild, moderate and severe [23].
Ethical issues
This protocol was received and approved by Mansoura Faculty of Medicine Institutional Research Board, Mansoura, Egypt. Written consent was obtained from each adult individual participate in this study either inpatient group or control group. For children, written consent was taken from their parents or caregivers.
Genotyping
A 4 ml of whole blood was collected from participants and reserved at – 20C until use. The extraction of DNA was done using a Thermo Scientific DNA Purification mini kit (cat number: K0781; Thermo Scientific, Lithuania, EU). The polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP) assay was used to genotype TNF-α (rs1799964) [24], and a polymerase chain reaction (PCR) assay was used to genotype the IL-4 gene intron 3 VNTR polymorphism [25]. PCR for both polymorphisms was performed with a 25 μl reaction mixture containing 4 μl DNA, 4 μl nuclease-free water, 16 μl master mix (Thermo Scientific DreamTaq Green PCR Master Mix (2X), Catalog number: K1081) and 0.5 μl of each primer. The primer sequence, PCR conditions, and PCR products are explained in Table 1. TNF-α (rs1799964) PCR products were digested with BbsI restriction endonucleases (Catalog number: FD1014, Thermo Scientific Fast Digest, USA) (C allele, 161 and 109 bp; T allele, 270 bp). Digested PCR fragments were visualized on a 2% agarose gel.
Statistical analysis
All data were entered, tabulated, and organized using Microsoft Office 2019. The Statistical Package of Social Science (IBM-SPSS) version 20 for the Windows operating system (Chicago, IL, USA) was used for data analysis. The quantitative data were expressed as mean and standard deviation (SD). The chi-square (χ2) test was used to evaluate the Hardy–Weinberg equilibrium (HWE) for the distribution of the genotypes of the controls. Differences between patients and controls in frequencies of gene polymorphisms were compared using the chi-square (χ2) test or Fisher’s exact test as appropriate. The odds ratio and 95% confidence interval (CI) were calculated for risk assessment. All p-values less than 0.05 were considered statistically significant.
Results
Table 2 shows the demographic and clinical data for AA patients and controls. All cases and controls were randomly selected from the same locality. The mean age of AA patients (MEAN ± SD) was 28.67 ± 8.37 years, males were higher (54.4%) than females (45.6%), and the mean disease duration (MEAN ± SD) was 3.88 ± 2.21 months. In the control group, the mean age of participants was 28.03 ± 7.26 years, and males represented 60.5% of the control group while females were 39.5%. The patients were graded according to SALT score to mild (46.8%), moderate (26.6%), and severe (26.6%).
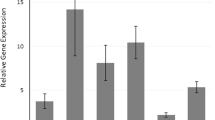
The genotype distributions of studied polymorphisms are shown in Table 3. The frequencies of R1R1, R1R2, and R2R2 genotypes of IL-4 gene intron 3 VNTR polymorphism in the patients were 1.3%, 41.8%, and 57.0% and in the controls were 6.4%, 34.4%, and 59.2%. R1 and R2 allele frequencies were 22.2% and 77.8% in patient group and 23.6% and 76.4% in the control group. In terms of the TNF- α (rs1799964) polymorphism, the patient group had 3.8%, 38%, and 58.2% of the CC, CT, and TT genotypes, while the control group had 5.1%, 42%, and 52.9%. The C and T alleles frequencies in the patient group were 22.7% and 77.3%, while in the control group they were 26.1% and 73.9%. For IL4, codominant, dominant, recessive and overdominant models of inheritance were applied with no significant association in genotype distribution in both groups (p 0.11, 0.74, 0.052 and 0.27, respectively) even after sex and gender adjustment no significant association was observed (p 0.11, 0.66, 0.059 and 0.23, respectively). For TNF-α, the same modes of inheritance were applied with no significant relation was observed (p 0.71, 0.43, 0.65 and 0.55, respectively). Also, after sex and gender adjustment no association was observed (p 0.73, 0.46, 0.65 and 0.58, respectively). The HWE was applied in the control group and there was no deviation for both expected and observed frequencies (p > 0.24 and 0.26 for IL4 and TNF, respectively).
Table 4 shows the possible combined genotypes of the two selected polymorphisms. Nine possible combined genotypes were detected. Among the observed genotypes, TT/R2R2 was the most frequent in both the patient and control groups. The least frequent inpatient group was TT/R1R1 and in the control group was CT/R1R1. The combined genotype CC/R1R1 was not detected in both groups. There is no combined genotype significantly associated with AA (p > 0.05).
The relation between both genotypes and different patient data involving family history, gender, alopecia subtypes, area of involvement, nail dystrophy, stress, and severity are explained in Tables 5 and 6. No statistically significant data were detected between any of genotype and data of AA patients (p > 0.05).
Table 7 shows the relationship between different genotypes of IL-4 gene intron 3 VNTR and TNF-α (rs1799964) with the degree of hair loss assessed by SALT score (p 0.221 and 0.22, respectively) and the number of attacks (p 0.466 and 0.604, respectively).
Discussion
AA is a disease with an immunological base in different studies [26,27,28]. The exact pathophysiology is still unclear and has not been determined [29]. It has been suggested that AA is an autoimmune process mediated by T cells and triggered by different stimuli, either endogenous and/or exogenous, with the interaction of different molecules like cytokines [30]. The hair follicle has an immune-privileged nature that protects it from autoimmune attacks. Different mechanisms are responsible for this, as the low number of T cells in anagen hair bulb, absent major histocompatibility complex (MHC I) expression, melanocytes are MHC I negative, very low NK cell content in the anagen hair follicle, and multiple immunosuppressant molecules produced by anagen hair bulb [31, 32]. When there is a breakage of this immune balance, there will be lymphocyte infiltration in the hair follicle that appears as a “swarm of bees” pattern [33]. The infiltration was markedly observed in the acute stage, with an accumulation of T helper and T cytotoxic cells. The role of T cell subtypes and their cytokines in AA is still questionable and not well documented [29].
In this study, two cytokines (TNF-α and IL-4) produced by T cells were chosen to study their polymorphisms (TNF-α rs1799964 and IL-4 gene intron 3 VNTR) in patients with AA. None of the selected have statistical significance when patients with AA are compared with normal controls. Moreover, we got the same results when the genotypes were compared with the patient’s clinical and demographic data.
The TNF-α gene is located on the short arm of chromosome 6 next to the HLA class II region, which is highly polymorphic and contains many linkages disequilibrium, making it a major challenge [34]. TNF-α expression is regulated by several single nucleotide polymorphisms (SNPs) in the promoter region, the most important of which are 238, 308, 863, 857, and 1031 [35]. TNF-α − 1031 (T/C; rs1799964) is considered as a functional SNP affecting gene expression as it lies close to the binding sites of 2 important transcriptional factors-kB and octamer binding transcription factor 1(OCT-1) [36]. The minor allele frequency (1031 C) is 22% in the 1000 Genome Database, and some studies have found that the C allele has higher transcriptional activity than the T allele [37]. To our knowledge, this is the first time this polymorphism has been tested in AA. However, it has been investigated in different autoimmune, inflammatory and malignant disorders, either alone or associated with other polymorphisms, with conflicting results [38]. Moreover, its role in other skin diseases has been reported. A study from India involved 733 patients showed the significant association of − 1031 with the other four promotor polymorphisms are significantly associated with generalized vitiligo [39]. In Bullous pemphigoid, the minor C allele might be protective [40]. A study on Spanish patients showed that − 238 and − 1031 polymorphisms might be risk factors in moderate and sever forms of psoriasis [41].
The role of the other TNF-α promotor gene polymorphisms in AA has been studied. Galbraith and Pandey studied the association of − 238 and − 308 with AA and found no differences between patients and controls as regard − 238, while for − 308 there was a significant difference between patchy AA patients and controls [42]. The same results for − 308 were obtained from a study on 59 Mexican patients [43]. A study on Turkish patients found an association of − 238 with AA and individuals with the GA genotype have a higher risk for AA [44]. On the other hand, two studies from Egypt and one study from Iran found no association between − 308 polymorphism and AA [45,46,47].
The IL-4 gene is located on the long arm of the fifth chromosome 5 (q23-31) [48]. It is about 10 kb in size, with four exons and three introns [49]. It lies in a cluster of genes related to other cytokines; most of these cytokines are related to TH-2 cells (IL-3, IL-5, IL-9, IL-13, and IL-15, granulocyte colony-stimulating factor) [50]. The third intron contains a VNTR polymorphism span of about 70 bp. IL-4 VNTR may alter the splicing site of mRNA, which produces different variants [51]. There are two alleles for this polymorphism: one with a 70-bp deletion and the other with a 70-bp insertion. The deletion allele is rare, has 2 repeats with 183 bp, and is assigned as R1. The insertion allele is the frequent one, has 3 repeats with 253 bp, and is assigned as R2 [52]. The R1 allele was suggested to increase the expression of IL-4 and the R2 allele has a protective role in some studies [53]. Moreover, the R2R2 genotype is associated with decreased IL-4 levels [54].
The role of IL-4 VNTR has been evaluated in different disorders with or without an immunological basis with different results like prostate cancer [55], dysmenorrhea [56], end‐stage renal disease [57], type 2 diabetes mellitus and its complication [58], autoimmune hepatitis type 1 [59], rheumatoid arthritis [60], immune thrombocytopenic purpura [61] and multiple sclerosis [50]. In AA, there are very few studies regarding the role of this polymorphism. A case–control study from Turkey involving 116 patients with AA and 125 healthy controls showed that the R1 allele was statistically higher in patients with the R2R2 genotype when compared with the R1R2 + R1R1 genotype, a statistically significant difference was present. On the other hand, our study did not find any significant association when patients were compared with controls. This polymorphism was investigated in other dermatological disorders based on the immune system. In vitiligo, a study on the Gujarati Indian population found that both alleles and genotypes were significantly different when patients were compared with controls [62]. In systemic lupus patients with cutaneous manifestation, the R1 allele was significantly different between patients and controls [63].
The study of cytokines is very essential as their role is very critical in the regulation of immune system response. Any change in cytokine levels either by increasing or decreasing, leads to immune system disturbance and may precipitate autoimmune response. Genetic polymorphisms are one of the most important mechanisms that affect cytokine levels by affecting gene expression. IL-4 is an immunomodulatory cytokine. It stimulates the differentiation of naïve CD4 T cells to TH-2 cells and enhances the differentiation and maturation of TH-2, and maintains its cytokines secretion. This leads to impairment of the balance between TH-1 and TH-2 cells, which precipitates an autoimmune response [64]. Moreover, it stimulates B cell immunoglobulin heavy chain class switch to IgE and increases IgE levels, which is the principal mediator of immediate hypersensitivity reactions [62]. This may be an explanation for disease susceptibility and the association with atopic dermatitis. Also, it seems that TNF-α and IL-4 play in a harmony. TNF-α makes the surrounding micro-environment rich in IL-4 cytokine which facilitates IgE class switching. Moreover, it was found that the B cell-activating factor, which is considered one of the TNF-α family, increased in the sera of severe AA patients [30].
In conclusion, our results did not suggest any association between IL-4 gene intron 3 VNTR and TNF-α (rs1799964) gene polymorphisms and the occurrence of AA in Egyptian patients. The main limitations of this study are that it was self-funded, which explains the small sample size plus the limited numbers of SNPs selected. Second, the disease pathology is complex and may involve environmental factors that were not evaluated. Third, all patients were from one canter, which means selection bias is unavoidable. Fourth, the previous studies regarding this issue were very few. Fifth is the limitation of the genotyping method.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AA:
-
Alopecia areata
- SLE:
-
Systemic lupus erythematosus
- HLA:
-
Human leucocyte antigen
- NK:
-
Natural killer
- TNF-α:
-
Tumor necrosis factor-alpha
- TH-1:
-
T helper-1
- TH-2:
-
T helper-2
- IL-4:
-
Interleukin-4
- VNTR:
-
Variable number of tandem repeats
- SALT:
-
Severity of Alopecia Tool
- PCR–RFLP:
-
Polymerase chain reaction-restriction fragment length polymorphism
- HWE:
-
Hardy–Weinberg equilibrium
- SNPs:
-
Single-nucleotide polymorphisms
- MHC I:
-
Major histocompatibility complex
References
Sterkens A, Lambert J, Bervoets A (2021) Alopecia areata: a review on diagnosis, immunological etiopathogenesis and treatment options. Clin Exp Med 21(2):215–230. https://doi.org/10.1007/s10238-020-00673-w
Zhou C, Li X, Wang C, Zhang J (2021) Alopecia areata: an update on etiopathogenesis, diagnosis, and management. Clin Rev Allergy Immunol 61(3):403–423. https://doi.org/10.1007/s12016-021-08883-0
Gilhar A, Etzioni A, Paus R (2012) Alopecia areata. N Engl J Med 366(16):1515–1525. https://doi.org/10.1056/NEJMra1103442
Lazzarini R, Oliari CB, Erthal AL (2016) Late-onset alopecia areata: descriptive analysis of 30 cases. An Bras Dermatol 91(6):844–845. https://doi.org/10.1590/abd1806-4841.20165184
Pratt CH, King LE, Messenger AG, Christiano AM, Sundberg JP (2017) Alopecia areata. Nat Rev Dis Primers 3(1):17011. https://doi.org/10.1038/nrdp.2017.11
Lundin M, Chawa S, Sachdev A, Bhanusali D, Seiffert-Sinha K, Sinha AA (2014) Gender differences in alopecia areata. J Drugs Dermatol 13(4):409–413
Darwin E, Hirt PA, Fertig R, Doliner B, Delcanto G, Jimenez JJ (2018) Alopecia areata: review of epidemiology, clinical features, pathogenesis, and new treatment options. Int J Trichol 10(2):51–60. https://doi.org/10.4103/ijt.ijt_99_17
Noso S, Park C, Babaya N, Hiromine Y, Harada T, Ito H et al (2015) Organ specificity in autoimmune diseases: thyroid and islet autoimmunity in alopecia areata. J Clin Endocrinol Metab 100(5):1976–1983. https://doi.org/10.1210/jc.2014-3985
Mohan GC, Silverberg JI (2015) Association of vitiligo and alopecia areata with atopic dermatitis: a systematic review and meta-analysis. JAMA Dermatol 151(5):522–528. https://doi.org/10.1001/jamadermatol.2014.3324
Thompson JM, Mirza MA, Park MK, Qureshi AA, Cho E (2017) The role of micronutrients in alopecia areata: a review. Am J Clin Dermatol 18(5):663–679. https://doi.org/10.1007/s40257-017-0285-x
Kridin K, Shalom G, Comaneshter D, Cohen AD (2020) Is there an association between alopecia areata and systemic lupus erythematosus? A population-based study. Immunol Res. https://doi.org/10.1007/s12026-020-09115-x
Nasreen S, Ahmed I, Wahid Z (2016) Associations of lichen planus: a study of 63 cases. J Pak Assoc Dermatol 17(1):17–20
Chu S-Y, Chen Y-J, Tseng W-C, Lin M-W, Chen T-J, Hwang C-Y et al (2011) Comorbidity profiles among patients with alopecia areata: the importance of onset age, a nationwide population-based study. J Am Acad Dermatol 65(5):949–956. https://doi.org/10.1016/j.jaad.2010.08.032
Biran R, Zlotogorski A, Ramot Y (2015) The genetics of alopecia areata: new approaches, new findings, new treatments. J Dermatol Sci 78(1):11–20. https://doi.org/10.1016/j.jdermsci.2015.01.004
Ho C-Y, Wu C-Y (2023) Clinical and genetic aspects of alopecia areata: a cutting edge review. Genes 14(7):1362
Rajabi F, Drake LA, Senna MM, Rezaei N (2018) Alopecia areata: a review of disease pathogenesis. Br J Dermatol 179(5):1033–1048. https://doi.org/10.1111/bjd.16808
Basu A, Ramamoorthi G, Albert G, Gallen C, Beyer A, Snyder C et al (2021) Differentiation and regulation of TH cells: a balancing act for cancer immunotherapy. Front Immunol. https://doi.org/10.3389/fimmu.2021.669474
Gohary YM, Abdel Fattah DS (2017) Detection of tumor necrosis factor-alpha in nonlesional tissues of alopecia areata patients: a prove for a systemic disease. Int J Trichology 9(4):154–159. https://doi.org/10.4103/ijt.ijt_47_17
Kalkan G, Karakus N, Baş Y, Takçı Z, Özuğuz P, Ateş Ö et al (2013) The association between Interleukin (IL)-4 gene intron 3 VNTR polymorphism and alopecia areata (AA) in Turkish population. Gene 527(2):565–569. https://doi.org/10.1016/j.gene.2013.05.086
Abd El-Raheem T, Mahmoud RH, Hefzy EM, Masoud M, Ismail R, Aboraia NMM (2020) Tumor necrosis factor (TNF)-alpha- 308 G/A gene polymorphism (rs1800629) in Egyptian patients with alopecia areata and vitiligo, a laboratory and in silico analysis. PLoS ONE 15(12):e0240221. https://doi.org/10.1371/journal.pone.0240221
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191. https://doi.org/10.3758/bf03193146
Wyrwich KW, Kitchen H, Knight S, Aldhouse NVJ, Macey J, Nunes FP et al (2020) The alopecia areata investigator global assessment scale: a measure for evaluating clinically meaningful success in clinical trials. Br J Dermatol 183(4):702–709. https://doi.org/10.1111/bjd.18883
Bakry OA, Basha MA, El Shafiee MK, Shehata WA (2014) Thyroid disorders associated with alopecia areata in Egyptian patients. Indian J Dermatol 59(1):49–55. https://doi.org/10.4103/0019-5154.123494
Kamoun M, Chelbi H, Houman MH, Lacheb J, Hamzaoui K (2007) Tumor necrosis factor gene polymorphisms in Tunisian patients with Behcet’s disease. Hum Immunol 68(3):201–205. https://doi.org/10.1016/j.humimm.2006.12.006
Mout R, Willemze R, Landegent JE (1991) Repeat polymorphisms in the interleukin-4 gene (IL4). Nucleic Acids Res 19(13):3763. https://doi.org/10.1093/nar/19.13.3763
Leung MC, Sutton CW, Fenton DA, Tobin DJ (2010) Trichohyalin is a potential major autoantigen in human alopecia areata. J Proteome Res 9(10):5153–5163. https://doi.org/10.1021/pr100422u
Wang EHC, Yu M, Breitkopf T, Akhoundsadegh N, Wang X, Shi FT et al (2016) Identification of autoantigen epitopes in alopecia areata. J Invest Dermatol 136(8):1617–1626. https://doi.org/10.1016/j.jid.2016.04.004
Gilhar A, Laufer-Britva R, Keren A, Paus R (2019) Frontiers in alopecia areata pathobiology research. J Allergy Clin Immunol 144(6):1478–1489. https://doi.org/10.1016/j.jaci.2019.08.035
Gautam RK, Singh Y, Gupta A, Arora P, Khurana A, Chitkara A (2020) The profile of cytokines (IL-2, IFN-gamma, IL-4, IL-10, IL-17A, and IL-23) in active alopecia areata. J Cosmet Dermatol 19(1):234–240. https://doi.org/10.1111/jocd.12970
Ito T, Kageyama R, Nakazawa S, Honda T (2020) Understanding the significance of cytokines and chemokines in the pathogenesis of alopecia areata. Exp Dermatol 29(8):726–732. https://doi.org/10.1111/exd.14129
Welker P, Foitzik K, Bulfone-Paus S, Henz BM, Paus R (1997) Hair cycle-dependent changes in the gene expression and protein content of transforming factor beta 1 and beta 3 in murine skin. Arch Dermatol Res 289(9):554–557. https://doi.org/10.1007/s004030050239
Kiselev A, Park S (2024) Immune niches for hair follicle development and homeostasis. Front Physiol. https://doi.org/10.3389/fphys.2024.1397067
Genedy RM, Badran FK, Tayae EM, Sabra HN (2021) Lesson to learn from cellular infiltrate in scalp biopsy of alopecia areata. Am J Dermatopathol 43(12):e158–e164. https://doi.org/10.1097/dad.0000000000001929
Asghar T, Yoshida S, Kennedy S, Negoro K, Zhuo W, Hamana S et al (2004) The tumor necrosis factor-α promoter −1031C polymorphism is associated with decreased risk of endometriosis in a Japanese population. Hum Reprod 19(11):2509–2514. https://doi.org/10.1093/humrep/deh478
Ghavami SB, Chaleshi V, Derakhshani S, Aimzadeh P, Asadzadeh-Aghdaie H, Zali MR (2017) Association between TNF-α rs1799964 and RAF1 rs1051208 MicroRNA binding site SNP and gastric cancer susceptibility in an Iranian population. Gastroenterol Hepatol Bed Bench 10(3):214
Sandoval-Pinto E, Padilla-Gutiérrez JR, Valdés-Alvarado E, García-González IJ, Valdez-Haro A, Muñoz-Valle JF et al (2016) Association of the − 1031 T > C polymorphism and soluble TNF-α levels with acute coronary syndrome. Cytokine 78:37–43. https://doi.org/10.1016/j.cyto.2015.11.014
Zhou X, Wang C, Chen Z, Peng Y, Peng H, Hou X et al (2018) Association of TNF-α rs1799964 and IL-1β rs16944 polymorphisms with multiple system atrophy in Chinese Han population. Int J Neurosci 128(8):761–764. https://doi.org/10.1080/00207454.2017.1418346
Marabi MH, Mozaffari HR, Ghasemi H, Hatami M, Yari K (2024) Evaluation of the association between TNF-α-1031 T/C polymorphism with oral lichen planus disease. BMC Oral Health 24(1):189. https://doi.org/10.1186/s12903-024-03939-x
Laddha NC, Dwivedi M, Begum R (2012) Increased Tumor Necrosis Factor (TNF)-alpha and its promoter polymorphisms correlate with disease progression and higher susceptibility towards vitiligo. PLoS ONE 7(12):e52298. https://doi.org/10.1371/journal.pone.0052298
Tabatabaei-Panah PS, Moravvej H, Sadaf Z, Babaei H, Geranmayeh M, Hajmanouchehri S et al (2019) Proinflammatory cytokine gene polymorphisms in bullous pemphigoid. Front Immunol 10(636):636. https://doi.org/10.3389/fimmu.2019.00636
Gallo E, Cabaleiro T, Román M, Abad-Santos F, Daudén E (2012) Study of genetic polymorphisms in the tumor necrosis factor α promoter region in Spanish patients with psoriasis. Actas Dermosifiliogr 103(4):301–307. https://doi.org/10.1016/j.ad.2011.10.002
Galbraith GM, Pandey JP (1995) Tumor necrosis factor alpha (TNF-alpha) gene polymorphism in alopecia areata. Hum Genet 96(4):433–436. https://doi.org/10.1007/BF00191802
Cristina CS, Mauricio SS, Armando LR, Celia SD, Clara RI, Rocio OL et al (2012) Tumor necrosis factor alpha promoter-308G/A polymorphism in Mexican patients with patchy alopecia areata. Int J Dermatol 51(5):571–575. https://doi.org/10.1111/j.1365-4632.2011.05291.x
Namdar ND, Akcilar R (2021) The association of TNFα-238 G/A gene polymorphism with alopecia areata. J Surg Med 5(5):463–466. https://doi.org/10.28982/josam.892542
El Sayed MH, El-Hefnawy A-HM, Al-Mashaiky FS, El Sayed SB (2014) Tumor necrosis factor α promoter− 308G/A polymorphism in patients with patchy alopecia areata. Egypt J Dermatol Venerol 34(1):36. https://doi.org/10.4103/1110-6530.137295
Abd El-Raheem T, Mahmoud RH, Hefzy EM, Masoud M, Ismail R, Aboraia NM (2020) Tumor necrosis factor (TNF)-α-308 G/A gene polymorphism (rs1800629) in Egyptian patients with alopecia areata and vitiligo, a laboratory and in silico analysis. PLoS ONE 15(12):e0240221
Moravvej H, Tabatabaei-Panah PS, Ebrahimi E, Esmaeili N, Ghaderian SMH, Ludwig RJ et al (2018) TNF-alpha -308G/A gene polymorphism in bullous pemphigoid and alopecia areata. Hum Antibodies 26(4):201–207. https://doi.org/10.3233/HAB-180339
Kalkan G, Yigit S, Karakus N, Bas Y, Seckin HY (2013) Association between interleukin 4 gene intron 3 VNTR polymorphism and recurrent aphthous stomatitis in a cohort of Turkish patients. Gene 527(1):207–210. https://doi.org/10.1016/j.gene.2013.05.053
Elsaid A, Shoaib RMS, Badr SS, Wahba Y, Ayyad SN (2021) Polymorphisms of interleukin 4 and interleukin 4 receptor genes and bronchial asthma risk among Egyptian children. Clin Biochem 93:66–72. https://doi.org/10.1016/j.clinbiochem.2021.04.006
Karakus N, Yigit S, Kurt GS, Cevik B, Demir O, Ates O (2013) Association of interleukin (IL)-4 gene intron 3 VNTR polymorphism with multiple sclerosis in Turkish population. Hum Immunol 74(9):1157–1160. https://doi.org/10.1016/j.humimm.2013.05.011
Elghoroury EA, Fadel FI, Farouk H, Elshamaa MF, Kamel S, Kandil D et al (2018) Association of variable number tandem repeats polymorphism in the IL-4 gene with end-stage renal disease in children. Egypt J Med Hum Genet 19(3):191–195. https://doi.org/10.1016/j.ejmhg.2017.08.009
Kuran G, Aslan H, Haytoglu S, OzalpYuregir O, Tug BS (2019) IL-1RN VNTR, IL-2(-330), and IL-4 VNTR gene polymorphisms in patients with chronic rhinosinusitis with sinonasal polyposis. Turk J Med Sci 49(5):1411–1417. https://doi.org/10.3906/sag-1710-186
Giri PS, Shah F, Gupta B, Dhangar A, Pathak VN, Desai B et al (2021) Genetic association of interleukin-4 VNTR polymorphism with susceptibility to rheumatoid arthritis in South Gujarat population. Gene Rep 25:101322. https://doi.org/10.1016/j.genrep.2021.101322
Salimi S, Mohammadoo-Khorasani M, Namazi L, Naghavi A, Yaghmaei M (2014) Association between interleukin 4 gene seventy-base-pair variable number of tandem repeats polymorphism and uterine leiomyoma. Gene Cell Tissue. https://doi.org/10.17795/gct-19462
Bingöl G, Polat F, Diler SB (2020) Association of IL-1Ra and IL-4 gene VNTRs with susceptibility to prostate cancer in Turkish population. Cytol Genet 54(5):487–492. https://doi.org/10.3103/S0095452720050138
Esen M, Nursal AF, Duman E, Yiğit S (2020) The role of Interleukin-4 VNTR polymorphism in dysmenorrhea development. Med Bull Haseki 58(4):364–369. https://doi.org/10.4274/haseki.galenos.2020.6162
Ksiazek K, Blaszczak J, Buraczynska M (2019) IL4 gene VNTR polymorphism in chronic periodontitis in end-stage renal disease patients. Oral Dis 25(1):258–264. https://doi.org/10.1111/odi.12974
Ali R, El-Said A, El-Baz H, Settin A (2018) Ethnic variation of IL-4 intron 3 VNTR gene polymorphism; its association with type 2 diabetes mellitus and its complication (neuropathy) in Egyptian subjects. Am J Med Genet B Neuropsychiatr Genet 177(7):635–640. https://doi.org/10.1002/ajmg.b.32647
Mansour AI, Behairy OG, AbdAlmonaem ER, Abd-Rabuh RM, Ahmed IAE (2018) Association of interleukin (IL)-4 variable number of tandem repeats (VNTRs) and IL-4-590 promoter polymorphisms with susceptibility to pediatric autoimmune hepatitis type 1. Cytokine 110:243–247. https://doi.org/10.1016/j.cyto.2018.01.009
Beh-Pajooh A, Fasihi-Ramandi M, Tavallaie M (2017) Association analysis of IL-4 VNTR polymorphism with rheumatoid arthritis in Iranian patients. Russ J Genet 53(3):406–409. https://doi.org/10.1134/S1022795417030036
Makhlouf MM, AbdElhamid SM (2014) Expression of IL4 (VNTR intron 3) and IL10 (-627) genes polymorphisms in childhood immune thrombocytopenic purpura. Lab Med 45(3):211–219. https://doi.org/10.1309/LMB0QC5T1RXTTRZQ
Imran M, Laddha NC, Dwivedi M, Mansuri MS, Singh J, Rani R et al (2012) Interleukin-4 genetic variants correlate with its transcript and protein levels in patients with vitiligo. Br J Dermatol 167(2):314–323. https://doi.org/10.1111/j.1365-2133.2012.11000.x
Mohammadoo-khorasani M, Salimi S, Tabatabai E, Sandoughi M, Zakeri Z, Farajian-Mashhadi F (2016) Interleukin-1β (IL-1β) & IL-4 gene polymorphisms in patients with systemic lupus erythematosus (SLE) & their association with susceptibility to SLE. Indian J Med Res 143(5):591–596. https://doi.org/10.4103/0971-5916.187107
Iwaszko M, Biały S, Bogunia-Kubik K (2021) Significance of Interleukin (IL)-4 and IL-13 in inflammatory arthritis. Cells. https://doi.org/10.3390/cells10113000
Acknowledgements
Not applicable.
Funding
Self-funded.
Author information
Authors and Affiliations
Contributions
Maged Mostafa and Maha Abdelsalam contributed to conceptualization; Marwa Zohdy and Maha Abdelsalam contributed to methodology and writing—review and editing; Maged Mostafa contributed to formal analysis and writing—original draft preparation and supervised the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Mansoura Faculty of Medicine Institutional Research Board under proposal code R.20.08.968 at 2020/08/05.
Consent for publication
Not applicable.
Competing interests
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mostafa, M., Zohdy, M. & Abdelsalam, M. The evaluation of IL-4 VNTR intron 3 and TNF-α (rs1799964) gene polymorphisms in Egyptian patients with alopecia areata: a case–control study. Egypt J Med Hum Genet 25, 83 (2024). https://doi.org/10.1186/s43042-024-00558-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-024-00558-7