Abstract
Background
The genetic approach to Marfan syndrome (MFS) has evolved over the last few decades, as has our understanding of the variants’ potential structural and functional consequences. It has been proposed that next-generation sequencing be used to improve genetic diagnosis and patient management. To this end, we used a targeted NGS custom panel to perform genetic analysis in a patient with MFS and his or her family members.
Case presentation
Here, we describe a novel germ-line heterozygous missense variant (transversion c.5371 T > A) found in exon 43 of the FBN1 gene of a patient (proband) with MFS. FBN1 (ENSG0000166147) and TGFB2 (ENSG0000166147) were included in a targeted sequencing panel for MFS (ENSG0000163513). This new variant c.5371 T > A was identified only in the proband, not in unaffected family members or healthy controls.
Conclusions
Given the massive amount of data generated by gene panel analysis, clinical interpretation of genetic variants may become more difficult. As a result, 3D modeling and multidisciplinary approaches should be used in the analysis and annotation of observed variants. The analysis of the protein’s conformational structure in relation to the identified variant could provide useful information. These data can be used to classify observed variants (pathogenic vs non-pathogenic) linked to the MFS phenotype, as well as to track disease progression and potential target treatments.
Similar content being viewed by others
Background
Marfan syndrome (OMIM 154,700) is a genetic connective tissue disorder with an autosomal dominant inheritance pattern that affects the ocular, skeletal, and cardiovascular systems (prevalence 2–3/10000). [1] MFS is caused by pathogenic variants in the FBN1 gene (OMIM 134,797), which alter the FBN1 protein and cause misfolding. [2, 3]
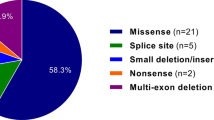
The FBN1 gene is found on the long arm of chromosome 15 (15q21.1) and is relatively large (237.5 kb), with 65 exons in its coding sequence. [4] FBN1 encodes profibrillin, which is converted to asprosin and fibrillin-1, a large glycoprotein of about 350 kDa (2871 amino acids) with multiple functional domains called fibrillin-1, which consists primarily of 6-cysteine epidermal growth factor (EGF)-like and calcium-binding EGF motifs, with a 8-cysteine motifs (TGF-beta binding/8-Cys) intermixed. [5] Different pathogenic variants have been identified in association with MFS, which have almost complete penetrance but phenotypic variability both within and between families. Almost 2000 pathogenic variants (missense, alternative splicing, out-of-frame deletions and deletions) are involved in defective protein folding, secretion, assembly, and degradation, resulting in weakened connective tissues. [4, 6] Furthermore, deletions of the entire gene have been reported, resulting in a decrease in the amount of protein produced. [7]
In subjects with MFS, fibrillin-1 levels are lower in tissues like blood vessels, lungs, skin, and ocular ligaments, which contributes to the functional reduction of microfibrils. [8]
Even within families, MFS clinical variability is noticeable in terms of age of onset, severity, and number of clinical manifestations. Except for neonatal forms of MFS [9, 10] and truncating variants with a more severe aortic phenotype, no strong genotype–phenotype correlation between MFS and FBN1 variants has been reported to date. [11, 12]
Pathogenic variants in the FBN1 gene have been reported in a variety of clinically distinct syndromes, including Weill–Marchesani syndrome, Shprintzen–Goldberg syndrome, acromelic dysplasia associated with family aortic aneurysms, and a wide range of skeletal, connective, and cutaneous tissue anomalies [13]. It is becoming clear that the expanded concept of fibrillinopathies entails complex mechanisms, such as tissue-specific fibrillin microfibril microenvironments, collaborative relationships between the structures of fibrillin microfibril networks, and biological functions like growth factor signaling regulation [14] . Here, we report on a novel germ-line heterozygous missense variant (transversion c.5371 T > A) identified in exon 43 of the FBN1 gene of patient (proband) with clinical suspect of MFS.
The new variant was classified as PM5, PP2, PP3 BP4, PP4 based on the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG) guidelines, as well as the fact that four other causative variants have been described in the same position [15]. By comparing the effects of all amino acids in the 1791codon (neutral variants, SNPs, and non-synonymous variants) and a 3D protein structure using a comparative approach of all known variants, bioinformatics analysis was carried out.
A 3-dimensional modeling was performed because this variant was not previously reported, as well as changes on the molecular level—the loss of disulfide bridges of the EGF-like 29 domain between TB7 and TB8, (TB8). Based on the results of 3D modeling and genetic and phenotypic data, this variant is strongly indicated as a fully causative pathogenetic variant.
Case presentation
Our Medical Genetics Unit received a referral for a 10-year-old female patient who was suspected of having MFS. MFS was not present in the family. She was the second child of non-consanguineous parents and was born after a physiological pregnancy via spontaneous delivery. During the neonatal and infant period, no clinical problems were referred. She was diagnosed with juvenile idiopathic scoliosis at the age of six and treated with a Milwaukee brace. Furthermore, at the age of six, 2D transthoracic echocardiography revealed mitral valve prolapse and a normal aortic root diameter. When the patient was 10, a general examination revealed a marfanoid habitus with slender limbs and a thin body (BMI < 3°ct). She was measured at 159 cm in height (75rd–90th percentile), 27.5 kg in weight (3rd–10th percentile), and 53.5 cm in occipital frontal circumference (OFC) (50th percentile). She showed an arm span-to-height ratio (L/D) of 1.053, chest deformity (pectus excavatum), kyphoscoliosis, and plain flat feet (pes planus). Additionally, the patient showed a positive wrist (Walker’s sign) and thumb (Steinberg) sign. She had a dolichofacial shape, a high-arched palate, and a malocclusion of the teeth. Out of an unconfirmed TSH increase, laboratory tests were within normal limits (complete blood count, urea and electrolytes, calcium, magnesium, and phosphate, liver function tests, creatine kinase, homocysteine). Her total systemic score was 9 based on the revised Ghent nosology, which took into account the previously noted mitral valve prolapse. At the age of ten, a new transthoracic echocardiography revealed the prolapse of both mitral valve leaflets with mild mitral regurgitation, as well as a 25-mm aortic root with a Z-Score of 1.78. At the age of ten, an ophthalmology examination revealed mild bilateral astigmatism (< 1 diopter) as well as a “slit lamp” evaluation. Based on anamnestic data, pre-test genetic counseling, objective examination (based on the presence of a systemic score > 7), and consideration of all possible differential diagnoses, including MFS, a genetic test was performed using a targeted sequencing panel that included two genes that predispose to MFS, FBN1 and TGFBR2. After obtaining informed consent, genomic DNA from three members of the family was extracted. All 65 coding exons and flanking intronic regions including splice sites of FBN1 were analyzed using a specific targeted sequencing panel designed to include two genes predisposing to MFS, FBN1 (ENSG0000166147) and TGFB2 (ENSG0000163513).
The variant was confirmed by bidirectional sequencing (Fig. 1), and the prediction of the functional effect of the c.5371 T > A variant on the FBN1 gene was performed using the “SNAP2” a trained classifier based on a neural network tool (https://www.rostlab.org/services/snap/). SNAP2 produce a heatmap of prediction scores effect of each variant from the wild-type amino acid (x-axis) to any other amino acid (y-axis) (Fig. 2). The scores are reported in Table 1 [15]. Furthermore, in consideration that this variation has not been reported before, structural characteristics such as secondary structure, accessibility to solvents and, if available, annotations on known functional residues, patterns, homologous regions are considered [16]. At the protein level, the consequences of the p.Cys1791Ser substitution on FBN1 tertiary structure were evaluated using Phyre2 software (Protein Homology‐fold Recognition Server; www.sbg.bio.ic.ac.uk/phyre2/) analyzing, in particular, the amino acid sequence between the TB7 and TB8 domain (AA 1500–2119) [17].
SNAP2 heatmap of FBN1 gene prediction scores. The predicted effect of each variant from the wild-type amino acid (x-axis) to any other amino acid (y-axis) The color red denotes a strong signal for effect, the color white denotes a weak signal (inconclusive prediction), and the color blue denotes a strong signal for neutral variants. All amino acid substitutions with a score of 88 or higher were highlighted in red in position 1971 (highlighted in yellow box)
Discussion and conclusions
In this case report, we identified a novel, apparently de novo, germ-line heterozygous variant in FBN1 gene (c.5371 T > A) in a female proband with suspect of MFS.
This missense variant determines the replacement of conserved cysteine residue with a serine and remove one of the six characteristic disulfide bridges within the EGF-like 29 domain.
Other four different amino acid substitutions in particular p.Cys1791Arg, p.Cys1791Tyr, p.Cys1791Phe, p.Cys1791Trp associated with MFS as reported in Universal Mutation Database (UMD) (http://www.umd.be/) [18] in the same position have been previously described. Despite the pathogenicity of the variants, the analysis reported in Ensembl (https://www.ensembl.org/index.html), associated with the 1791 codon, provides conflicting data. In particular, the variant p.Cys1791Trp (reported in Ensembl) is classified as pathogenetic for SIFT, probably damaging for Polyphen and likely benign for CADD confirming the variability of results of predictive tools.
To understand and classify this novel variant, considering the possible effects of all the amino acid changes reported at position 1791, an in silico comparative analysis was performed (Fig. 3).
The structure of the missense pathogenic variant in the amino acid sequence between the TB7 and TB8 domains was analyzed (AA 1500–2119). The variant p.Cys1791Ser found in the EGF-like domains 29 interferes with the formation of a disulfide bond between the two cysteines. (Residues 1777 and 1791 were highlighted in blue space filling mode.) The new pathogenic variant p.Cys1791Ser (panel B) causes an 8 per cent lengthening of the region between the TB6 and TB8 domains. The total length of the analyzed amino acid fragment changes from 126.80 Å in the wild-type protein to 136.70 Å in the mutant protein. The effect of the new variant is comparable to that of the variant p.Cys1791Phe (panel C), which causes an elongation of the analyzed region. The amino acidic changes to Thr and Arg (panels E and F) appear to be the least tolerated. These two pathogenic variants caused TB8 module misfolding with a rotation of about 90°, as indicated by the yellow circle. The final variant, p.Cys1791Tyr (panel D), appears to have no effect on protein length while causing a critical misfolding of the EGF-like 29 domain
SNAP2 as prediction software was used. This tool is able to distinguish between the effect of neutral variants, SNPs and non-synonymous variants taking in consideration evolutionary information and comparing the effect of all amino acids in the same codon. In a second step, 3D structure of the protein was analyzed by means of a comparative approach of all known variants in codon 1791.
Our results show how a single amino acidic change could induce considerable variation on the protein structure and stability due to crucial role of disulfide bridge between residues 1777 and 1791. As highlighted in Fig. 3, the new variant p.Cys1791Ser (panel B) determines an overall lengthening of the region between the TB7 domain and TB8 by 8%, comparable to the effect of the variant p.Cys1791Phe (Fig. 3 panel C). This fibrillin stretch is compatible with a limited amount of fibrillin in extracellular matrix with long, smooth, and thin fibers in the extracellular area. Furthermore, amino acidic change in Thr or Arg (respectively, Fig. 3 panel E and F) seems to be the least tolerated. As highlighted into yellow circle, these two pathogenic variants induced a TB8 module misfolding, with a rotation of about 90° and consequent deleterious effects on the packing of global fibrillin structure. These two pathogenic variants might also alter the volume of the calcium-binding pocket of the adjacent EGF-like domain with a consequent endoplasmic reticulum retention of the protein and an increase of fibrillin peptides proteolysis. Finally, the last variant p.Cys1791Tyr seems to have no effect on the length of the protein while produce a critical misfolding of the EGF-like 29 domain.
Evidence from our case and published data strongly supported that the p.Cys1791Ser is a new pathogenic variant of MFS, present only in the proband and absent in the other unaffected family members and healthy controls. The causal role of this variant is supported from the substitution in EGF-like domains 29 of FBN1 gene that plays a critical role in the pathogenesis of MFS producing different structural and functional consequences. The mutant residue substitutes a conserved 157 cysteine residue, with a serine removing one of the six characteristic disulfide bridges. The variant, in addition to a conformational change of the same domain, induces also a misfolding of neighboring domains causing a possible anomalous elongation of microfibrils [19, 20].
Only a broad integrated approach (such as data collection, phenotypic characteristics evaluation, bioinformatics approach, and protein modeling) can help in understanding molecular mechanisms and genotype–phenotype relationships.
Using simple prediction software, the conflicting data could be discovered. As a result, combining analysis and the creation of protein structural models may be advantageous. The visualization of three-dimensional models provides useful information on possible protein domain conformational changes those are directly related to pathogenicity and metabolic pathway modifications. These changes were linked to the clinical and/or phenotypic manifestations [21, 22].
This study emphasizes the importance of close collaboration between clinicians and laboratories throughout the diagnostic process, from clinical suspect to genetic variant identification, interpretation, and clinical contextualization, with the unavoidable introduction of functional investigations into the diagnostic workflow. Diagnostic algorithms are used in situations where the diagnosis is not immediately clear in Clinical Genetics Genetic Syndrome “gestalt.” Diagnoses still start with the recognition of a clinical situation based on observation of symptoms and signs, even with the current understanding of a greater variety of genetic pathologies and the recent understanding of the molecular basis of many of these illnesses. Even though some signs unquestionably match clinical hypotheses, they are still only speculative hypotheses [23, 24].
Availability of data and material
All the data and executed analyses are available and can be provided upon official request from the requesting institution.
References
Collod-Béroud G, Boileau C (2002) Marfan syndrome in the third Millennium. Eur J Hum Genet 10(11):673–681
Zeyer KA, Reinhardt DP (2015) Fibrillin-containing microfibrils are key signal relay stations for cell function. J Cell Commun Signal 9(4):309–325
Xiao Y, Liu X, Guo X, Liu L, Jiang L, Wang Q et al (2017) A novel FBN1 mutation causes autosomal dominant Marfan syndrome. Mol Med Rep 16(5):7321–7328. https://doi.org/10.3892/mmr.2017.7544
Fusco C, Morlino S, Micale L, Ferraris A, Grammatico P, Castori M (2019) Characterization of two novel intronic variants affecting splicing in FBN1-related disorders. Genes (Basel) 10(6):442
Wu YS, Bevilacqua VL, Berg JM (1995) Fibrillin domain folding and calcium binding: significance to Marfan syndrome. Chem Biol 2(2):91–97
Abramowicz A, Gos M (2018) Splicing mutations in human genetic disorders: examples, detection, and confirmation. J Appl Genet 59(3):253–268
Hilhorst-Hofstee Y, Hamel BC, Verheij JB, Rijlaarsdam MEB, Mancini MS, Cobben JM et al (2011) The clinical spectrum of complete FBN1 allele deletions. Eur J Hum Genet 19(3):247–252
Thomson J, Singh M, Eckersley A, Cain SA, Sherratt MJ, Baldock C (2019) Fibrillin microfibrils and elastic fibre proteins: functional interactions and extracellular regulation of growth factors. Semin Cell Dev Biol 89:109–117
Aubart M, Gazal S, Arnaud P, Benarroch L, Gross MS, Buratti J et al (2018) Association of modifiers and other genetic factors explain Marfan syndrome clinical variability. Eur J Hum Genet 26:1759–1772
Faivre L, Masurel-Paulet A, Collod-Béroud G, Callewaert B, Child AH, Stheneur C et al (2009) Clinical and molecular study of 320 children with Marfan syndrome and related type I fibrillinopathies in a series of 1009 probands with pathogenic FBN1 variants. Pediatrics 123:391–398
Baudhuin LM, Kotzer KE, Lagerstedt SA (2015) Increased frequency of FBN1 truncating and splicing variants in Marfan syndrome patients with aortic events. Genet Med J Am Coll Med Genet 17:177–187
Franken R, Groenink M, de Waard V, Feenstra HMA, Scholte AJ, van den Berg MP et al (2016) Genotype impacts survival in Marfan syndrome. Eur Heart J 37:3285–3290
Cecchi A, Ogawa N, Martinez HR, Carlson A, Fan Y, Penny DJ et al (2013) Missense mutations in FBN1 exons 41 and 42 cause Weill-Marchesani syndrome with thoracic aortic disease and Marfan syndrome. Am J Med Genet A 161A(9):2305–2310
Sakai LY, Keene DR, Renard M, De Backer J (2016) FBN1: The disease-causing gene for Marfan syndrome and other genetic disorders. Gene 591(1):279–291
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med Off J Am Coll Med Genet 17(5):405–424
Bromberg Y, Rost B (2007) SNAP: predict effect of non-synonymous polymorphisms on function. Nucleic Acids Res 35(11):3823–3835
Kelley LA, Mezulis S, Yates CM, Wass MN, Sternberg MJ (2015) The Phyre2 web portal for protein modeling, prediction and analysis. Nat Protoc 10(6):845–858
Béroud C, Collod-Béroud G, Boileau C, Soussi T, Junien C (2000) UMD (Universal mutation database): a generic software to build and analyze locus-specific databases. Hum Mutat 15(1):86–94
Schrijver I, Liu W, Brenn T, Furthmayr H, Francke U (1999) Cysteine substitutions in epidermal growth factor-like domains of fibrillin-1: distinct effects on biochemical and clinical phenotypes. Am J Hum Genet 65(4):1007–1020
Piersall LD, Dietz HC, Hall BD, Cadle RG, Pyeritz RE, Francomano CA et al (1994) Substitution of a cysteine residue in a non-calcium binding, EGF-like domain of fibrillin segregates with the Marfan syndrome in a large kindred. Hum Mol Genet 3(6):1013–1014
Wojcik MH, Thiele K, Grant CF, Chao K, Goodrich J, Odonnell-Luria A et al (2019) Genome sequencing identifies the pathogenic variant missed by prior testing in an infant with Marfan syndrome. J Pediatr 213:235–240
Ackerman JP, Bartos DC, Kapplinger JD, Tester DJ, Delisle BP, Ackerman MJ (2016) The promise and peril of precision medicine: phenotyping still matters most. Mayo Clin Proc 91:1606–1616
Homolak J, Kodvanj I. Possible marfanoid habitus of Cesare Alessandro Scaglia di Verrua evidenced in portraits of Sir Anthony van Dyck Am J Med Genet A. 2022 Sep 21.
Bukvic N, Elling WJ (2015) Genetics in the art and art in genetics. Gene Gene 555:14–22
Acknowledgements
No acknowledgements
Funding
No funding for the study should be declared.
Author information
Authors and Affiliations
Contributions
All persons who meet authorship agreement criteria are listed as authors and all authors certify that they have participated in the concept, design, analysis, writing and revision of work. MO contributed to original draft preparation. MT was involved in data curation and reviewing and editing. MR contributed to draft editing. CP was involved in conceptualization, draft editing, and investigation. MTP contributed to draft editing. NB was involved in reviewing, editing, and data analysis. MDM contributed to supervision. MC was involved in conceptualization, bioinformatics analysis, and original draft preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was carried out in accordance with the 2013 Revised Declaration of Helsinki of the World Medical Association. Appropriate informed consent for sequencing analysis was obtained from all family members. Parental approval was also obtained for the inclusion of the genetic data in a scientific publication. The informed consent used has been approved by the Ethics Committee “Cardarelli-Santobono” which specifies the possible use for experimentation and biomedical research activities that take place at the A.O.R.N. A. Cardarelli and A.O.R.N. Santobono-Pausilipon. There is no additional ethics statement or approval required for this study because no animals were used in it.
Consent to publish
According to the informed consent, the patient or study participant agrees to the publication of their personal information for scientific reports.
Competing interests
The authors declare no potential conflicts of interest with respect to research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oro, M., Tarsitano, M., Rivieccio, M. et al. An integration into the diagnostic workflow in a pediatric patient suspected of having Marfan syndrome. Egypt J Med Hum Genet 23, 152 (2022). https://doi.org/10.1186/s43042-022-00365-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00365-y