Abstract
Background
The complexity of infection in malaria-endemic areas is exacerbated by the presence of genetically diverse Plasmodium falciparum strains. There is a risk that more virulent or drug-resistant versions of the disease may arise. Therefore, we reviewed most reported molecular markers that have been detailed to date in Nigeria.
Main body of the abstract
In this review, we have summarized the genetic diversity of P. falciparum in Nigeria using the two well-reported genes (msp1 and msp2) as genetic diversity biomarkers. The review includes the findings obtained from research conducted in all major geopolitical regions of the country. We found that MSP-2 infection complexity is generally moderate to high in the North-central region. However, in the South-West, there were several regions where the multiplicity of infection (MOI) was either low or extremely high.
Conclusion
Understanding how Nigeria's malaria situation fits into various reports on P. falciparum genetic variation can improve treatment and immunization options. This review will be helpful for future treatment strategies that would be tailored to the specific needs of Nigeria's malaria-endemic populations.
Similar content being viewed by others
Background
Malaria is one of the world's most serious public health problems, with over 200 million annual cases. According to recent statistics, malaria infections are expected to reach 241 million in 2020, up from 227 million cases in 2019. The WHO African area accounted for the majority of this rise [1]. About 93% of all malaria cases are reported in Sub-Saharan Africa. Malaria is caused by Plasmodium sp. parasites, which are spread by the bite of infected female Anopheles mosquitoes. While there are multiple Plasmodium species that cause malaria, P. falciparum is responsible for the majority of the cases in Nigeria and most of Sub-Saharan Africa. Moreover, P. falciparum is the most virulent Plasmodium strain, responsible for the bulk of malaria-related deaths [2]. An infected female Anopheles mosquito injects sporozoites into the circulation of a human while feeding. The sporozoites subsequently travel to the hepatocytes of the liver, where they reproduce asexually, resulting in merozoites. After 7–10 days in the liver, these merozoites are discharged into the bloodstream and infect red blood cells, initiating the symptomatic erythrocytic cycle. Some merozoites reproduce asexually to enhance infection load and symptoms, while others change into immature male and female gametocytes that mosquitoes consume during feeding. These gametocytes fuse into a zygote during sexual reproduction in the mosquito stomach, then reproduce asexually in the salivary gland, creating sporozoites that continue the malaria cycle. Despite global attempts to lower the disease burden, malaria remains endemic in several nations and kills over 500,000 people each year [1]. Nigeria, with a population of slightly more than 200 million people, accounts for more than 30% of malaria deaths globally [1]. The rising genetic diversity of P. falciparum, which influences characteristics like its resistance to drugs, rate of transmission, and severity of symptoms, is one of the reasons why this parasite has proven difficult to eliminate in Nigeria. In order to circumvent the adaptive responses of the host immune system, P. falciparum undergoes antigenic flipping in infected hosts. Several clones emerge as a result of these modifications, which recombine in the mosquito gut during the zygote formation stage [3]. This mechanism results in parasite strains with more genetic variations. The evolution of the consequent resistance to several antimalarial drugs has made the management of malaria infection a major public health problem, particularly for children and pregnant women. The emergence and spread of drug resistance are key challenges to the fight against malaria [1,2,3]. There are numerous advantages of using molecular markers to assess antimalarial drug resistance in routine surveillance, particularly in areas with high endemicity, where there is a greater probability of the development of drug resistance. This review would help contextualize the malaria situation in Nigeria and might pave the way for improved treatment options.
Why it is vital to study genetic variation in malarial parasites
The increase in the genetic diversity of P. falciparum burdens the current malaria eradication efforts in Nigeria. As a result, a better understanding of the genetic variation in P. falciparum is critical for assessing the efficacy of antimalarial drugs and developing more successful eradication strategies [3].
Antimalarial medications function by targeting specific parasite loci. Each new P. falciparum strain, on the other hand, evolves a modification of these pharmacological targets, making current antimalarial medicines less effective [3].
Furthermore, the existence of multiple genetically diverse parasites in a population might increase the complexity of infection (COI) within its members [4]. The number of genetically diverse strains of one parasite simultaneously active in a single host is referred to as multiplicity of infection (MOI) or COI [5]. Genotyping can also provide valuable information regarding the diversity of antigenic alteration in immunological studies. More importantly, genotyping enables the determination of the MOI, which can be used to assess the efficacy of different interventions, such as drug trials, vaccine trials, or exposure-reduction strategies. Infected populations are generally genotyped utilizing genetic polymorphism to discriminate among genetically diverse P. falciparum isolates. Merozoite surface protein (msp) genes are the most commonly utilized markers in defining P. falciparum genetic diversity due to their high genetic variability [2,3,4,5]. MOI is an important parameter in malaria epidemiology. Thus, a person could be infected with many strains of P. falciparum at the same time. This can make treating the infection extremely difficult. When only one or two of the numerous strains are treatment-resistant or particularly virulent, these issues are more confounding. The failure to detect the drug-resistant strain, for example, can result in relapse, which can be mistakenly recorded as a new infection, resulting in an overestimate of treatment failure. Individual parasite clones can be tracked over time, allowing thorough analyses of the infection dynamics.
Role of merozoites and merozoite surface proteins (MSPs) in malaria infections
P. falciparum merozoites are an invasive life stage of the parasite that multiplies inside red blood cells before destroying them. This phenomenon activates host immune responses and leads to the pathophysiological symptoms associated with malaria [6]. The two key proteins on the plasma membrane of the parasite that perform critical roles in red blood cell invasion and the stimulation of inflammatory responses during the erythrocytic stage are MSP-1 and MSP-2 [7, 8]. These antigenic surface proteins are responsible for P. falciparum's successful evasion and drug resistance strategies [9]. MSPs are carried in unique organelles known as rhoptries and micronemes found at the apex of the merozoite and are linked to the surface of merozoites by glycophosphatidylinositol (GPI)-anchored proteins [8]. When the infected cells burst, these parasite proteins are released [10]. MSP-1 and MSP-2 are commonly exploited as vaccine targets [11], but they are also significant in identifying genetically different P. falciparum strains. For example, PCR–RFLP genotyping of parasites for MSP-2 allows researchers to discriminate between the different parasite strains present in a single blood sample. MSP-1 is the more frequent of the two MSPs and is found on chromosome 9 [12]. It is encoded by the msp-1 gene and has 17 sequence blocks, the most polymorphic of which is block 2. K1, MAD20, and ROC33 are three allelomorphic families found in this highly polymorphic block. MSP-2 is encoded by the msp-2 gene and has five blocks, the most polymorphic of which is block 3. FC27 and 3D7 are two allelomorphic families found in block 3. The genetic diversity is measured based on the variation in the distribution of these allelomorphic families within infected populations.
Several studies have found that the genetic diversity of this parasite varies depending on a variety of parameters, including the degree of infection, the age of the infected persons, and their geographic location [13,14,15,16]. In malaria-endemic countries like Nigeria, where transmission rates are higher, this diversity is greater [17].
Materials and methods
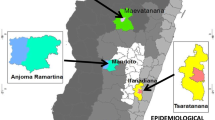
Nigeria has the seventh-largest population in the world and is one of Africa's most populous countries. It is also one of Africa's most densely populated countries, home to over 200 million people spread across a landmass of 920,000 square kilometers (360,000 square miles). Nigeria is in West Africa and borders the countries of Benin, Chad, Cameroon, and Niger. The country is divided into six geopolitical zones (Fig. 1) and there are more than 500 ethnic groups and languages in the 36 states and the Federal Capital Territory (FCT) of Nigeria. The Yoruba, the Hausa, and the Igbo are the most common ethnic groups in Nigeria.
A literature search was conducted to correlate the genetic diversity of merozoite surface proteins with infection multiplicity in Nigeria. The combination of keywords searched on Google Scholar and PubMed were 'Merozoite surface proteins,' 'Multiplicity of infection, 'monoclonal,' 'polyclonal,' and 'Nigeria. A range of related articles was collected but only articles that mentioned diversity in subfamilies of either Msp-1 or Msp-2 or both were mostly included in this review.
Results and discussion
Malaria-endemic communities with genetically heterogeneous P. falciparum strains increase the complexity of infection within such communities. This could result in the emergence of more virulent or drug-resistant forms, posing a threat to eradication efforts [18]. The msp1 and msp2 genes were used as genetic diversity biomarkers in this work to interrogate the genetic diversity of P. falciparum in Nigeria. This analysis examines the findings obtained from studies conducted across the country's major geopolitical zones. Because genetically diverse malaria strains may respond differently to treatment [8], the eradication attempts that do not consider the diversity of P. falciparum within-country zones may have a lower success rate. As a result, it is critical to comprehend these distinctions. This will ensure that future treatment strategies are tailored to the specific needs of Nigeria's malaria-endemic populations. Understanding how Nigeria's malaria situation fits into the worldwide discussion on P. falciparum genetic variation can assist in the design of stronger global treatment and immunization options, in addition to local applications.
In this review, the most common allelic families differed among geographies and malaria-endemic groups (Table 1). Dikwa et al. [19], in Kaduna, Nigeria, investigated the presence of P. falciparum among symptomatic and asymptomatic malaria-infected people, and the study observed that msp2 is the most common gene, accounting for more than two-thirds of all allelic variants observed. In symptomatic patients, where 3D7 was the most prevalent variant, genetic diversity was also higher. Asymptomatic individuals, on the other hand, had fewer allelic variations, with FC27 being the most common one. In both populations, RO33 was absent, whereas MAD20 was the most common msp1 allele. Unfortunately, there has been no additional research from this zone to compare these data with. However, reports from Myanmar, Ethiopia, and other Sub-Saharan African nations have found that 3D7 is the most common msp2 allele [20,21,22]. It also agrees with the findings of Oyedeji et al. [23, 24] in Nassarawa (North-Central), where 3D7 was found to be the most common msp2 allele in symptomatic uncomplicated malaria cases. These findings imply that the number of 3D7 alleles strongly correlates with symptomatic malaria. The higher number and heterogeneity of the identified alleles among symptomatic patients in the North-West of Nigeria further suggests that high genetic diversity may contribute to the intensity of the malaria infection, but this association has not been proved yet. For example, among the children with severe malaria in Nassarawa, the infections were mostly monoclonal, with little genetic variation and complexity [18]. However, because it does not address the msp1 gene, which may contain many more allelic families, the analyses from Oyedeji et al. [18] are insufficient to determine the impact of genetic diversity on malaria severity. The data from Amodu et al. [25] on children with severe malaria in the South-West state of Oyo back up this study, but it has the same limitations.
In Niger State, in North-Central Nigeria, Usman-Yamman et al. [15] found that msp1 was the most common allele among symptomatic patients, with MAD20 and FC27 as the most common msp1 and msp2 alleles, respectively (Table 1). Other findings in the North-West and North-Central regions contradict this [19, 23]. The low incidence of RO33, on the other hand, is consistent with observations in other parts of Nigeria and Cameroon [19, 26]. The findings are similarly consistent with those of Oyedeji et al. [24], who studied msp2 in Nassarawa (North-Central) and found extremely high polyclonal infections in homes with symptomatic uncomplicated malaria, with FC27 being the most common allele. The high number of polyclonal infections recorded in both experiments indicates that there is a lot of transmission in the zone, which could be due to strong genetic recombination occurring in the vectors or multiple infections from different vectors [27,28,29]. Despite the significant number of polyclonal infections observed in both studies, Oyedeji et al. [24] observed a much higher MOI and genetic diversity, implying that transmission regimes and parasite diversity in microenvironments differ from those in the general population.
Further south, the pattern of genetic diversity appears to vary dramatically. In contrast to earlier studies in the North-Central, Idakwo et al. [30] and Kolawole et al. [31], found a high prevalence of RO33 msp1 allelic families in three communities in Kogi and Kwara, respectively. In both investigations, K1 was the most common msp1 allele, while FC27 was the most common msp2 variant. Despite the fact that Kwara and Kogi states are in the North-Central zone, the genetic distribution pattern seen in the studied villages is similar to that reported in the southern states [28, 32–36]. This could be due to community transmission patterns being influenced by environmental factors. Environmental influences, like weather patterns, have been demonstrated to influence genetic diversity in studies [37, 38]. Despite their North-Central geopolitical zones, both states are located in the country's lower half, south of the Niger River, and have climatic characteristics similar to those of the southern states. It is also probable that this pattern of genetic dispersion is due to exchange between states south of the Niger River, which is fueled by socioeconomic activities [36, 39]. Both studies found that msp2 had a greater MOI and genetic diversity, though Kolawole et al. [31] found that Kwara had a larger genetic diversity. In both investigations, msp2 infections are primarily monoclonal. Idakwo et al. [30] found that the two riverine groups studied had lesser genetic diversity and a higher prevalence of monoclonal infections, which could indicate decreased transmission levels in the Niger River basin. It is also possible that the season in which the study was performed had an impact on it.
Intense human socioeconomic migration could possibly explain the similar genetic distribution pattern reported in different sections of the Southwest, where RO33 frequency was high, K1 and FC27 were the most common msp1 and msp2 allelomorphs, respectively [36, 40–42]. In some groups in the Southwest, however, RO33 or MAD20 was found to be the most common msp1 allele, whereas 3D7 was shown to be the most common msp2 allele [28, 33–35]. According to the findings of Oboh et al. [34], in a study on malaria transmission among pregnant and non-pregnant women in Lagos, RO33 and 3D7 were the most common msp1 and msp2 allelic families, but only among non-pregnant women. This is consistent with Funwei et al. [28] findings in Oyo urban and rural populations. Funwei et al. [28], on the other hand, found much more genetic diversity and MOI, implying higher transmission levels. In contrast to other research in the South-West, Abiodun et al.[26] found a low level of RO33 among asymptomatic sickle cell anemia patients in Lagos who were treated with various malaria prevention methods. In the trial, however, RO33 levels rose in patients who did not get chemoprophylaxis.
The prevalence of FC27 in studies among southern and middle belt populations, as well as asymptomatic patients in the north, could indicate that infections in these areas are more resistant to treatment with artemisinin combination therapy (ACT) [42], which is the most commonly used antimalarial drug in Nigeria. Ibara-Okabande et al. [43] reported that FC27 was the predominant allele in the majority of recurrent malaria cases among children treated with ACT in Southern Brazzaville (Congo), as opposed to the 3D7 alleles that were predominant in children who remained protected from infection for up to a year after treatment. While this shows that infections caused by FC27 are more difficult to treat, the study did not specify whether the recurrent malaria infections were new or old. Unfortunately, no recent research has examined this association in any of Nigeria's regions. In Nigeria, the studies most pertinent to this were conducted in the South-West by Amodu et al. [25] and Happi et al. [32]. Happi et al. [32] found that recrudescent malaria infections in children treated with chloroquine had lower but still significant msp2 prevalence and MOI. msp2 alleles did not properly predict the occurrence of severe malaria in the post-ACT population, according to Amodu et al. [25], who analyzed two groups before and immediately after the state-wide switch from chloroquine to ACT antimalarial medicines between 1998 and 2005. FC27 presence in several states may dampen the malaria eradication efforts in Nigeria, particularly because it is prevalent in asymptomatic people [19, 23, 44, 45]. Recurrent symptomatic infections, increased newborn and maternal mortality, cognitive impairments, and complicated infections involving bacteria are all common outcomes of asymptomatic malaria infections [44]. The recurring occurrences in Congo may have been caused by reinfection from asymptomatic patients with FC27. In Edo State (South-south), the research considered only the presence of Merozoite surface proteins and did not address the diversity of the genes coding for each merozoite surface protein, while in Plateau (North-central), the research focused on the diversity of one gene in msp2, (FC-27), which gives sparse information on the gene predominant in that region (Table 2). Another limitation is the small sample size that was found positive for the FC27 gene. In general, infection complexity was moderate to high in the North-West and North-Central in msp2 [15, 24, 31]. In the South-West, however, the results were mixed, with numerous regions reporting extremely low and very high MOI [25, 32, 34]. High MOI in the research studied could indicate high malaria transmission, which could have implications for both the epidemiology of drug-resistant P. falciparum malaria and the treatment outcomes in patients [35]. The incidence of RO33 was likewise determined to be mostly a southern phenomenon, with no or few reports in the country's northern regions. Notably, research in the north only found polymorphism RO33 in the presence of other alleles [15], whereas reports from the south found a mix of monomorphic and polymorphic RO33 in single and complex infections [25].
Numerous studies on the genetic diversity of P. falciparum have been reported from the Southwest and North Central zones of Nigeria. By considering varying population patterns, malaria prevalence, time periods, and the choice of a variety of genetic markers, the authors hope to better understand the underlying genetic diversity in these regions. Idakwo et al. [30] included subjects between the ages of 2 and above who had symptoms similar to simple malaria. In another study, 80 samples from two nearby communities (Idah and Ibaji communities) along the Niger River were randomly selected for the genotyping of Merozoite surface protein 1 and 2 polymorphisms. Two MSP-2 (FC27 and 3D7) and all three MSP-1 reported families (K1, MAD20, and RO33) were found among the isolates in these samples, highlighting the high level of diversity of the field isolates (Table 1). According to Kolawole et al. [31], a different study from North Central was carried out between the months of October and November 2012. About 200 people with malaria symptoms were enrolled in this trial. However, parasite genomic DNA was only extracted from 50 samples. For MSP-1, three allelic types were identified: KI, MAD20, and RO33. A total of 39 (81%) of the blood samples contained MSP-1. MSP-2 was detected in 31 (64.58%) of the blood samples, with both FC27 and 3D7 allelic types being present. Using MSP 1 and 2 molecular markers, Usman-Yamman et al. [15] investigated the genetic diversity among newborns between the ages of 6 months and 17 years. MSP 1's dominant allele was MAD 20, while MSP 2's dominant allele was FC-27. According to Oyedeji et al. [24], 93 children from 43 different families and households participated in the study in Lafia. Although the majority of the houses had two or three infected children, each home had at least one child who had a P. falciparum infection that was verified by microscopy. Males made up 59.1% (55/93) of the 93 youngsters enrolled, while females made up 40.9% (38/93). They were between the ages of 9 months and 12 years old. All of the study's young participants' isolates had their msp-2 gene alleles genotyped. According to the distribution of msp 2 alleles among the 93 children from the 43 houses examined, P. falciparum isolates exhibit significant genetic variety, which is demonstrated by the inter- and intra-allelic diversity. In total, 215 MSP-2 were recorded. The FC27 allele type was shown to be much more prevalent than the 3D7 allele type when compared to the 3D7 allele type (Table 1). Dikwa et al. [19] also looked at the genetic diversity of P. falciparum in the North Central city of Kaduna. In this investigation, P. falciparum was detected in 42 samples, including 12 asymptomatic and 30 sick people. However, the polymorphic msp1, msp2, and glutamate-rich protein genes were found in 19 out of 42 of the P. falciparum isolates. The MAD20 and KI alleles from the symptomatic group were found in the msp1 gene. However, just a single 1MAD20 (20.0%) allele was found in isolates from asymptomatic people. Both groups have 3D7 and FC27 found in the msp 2 gene.
The study by Ojurongbe et al. [42] investigated the diversity of Merozoite surface protein -2. The sample size was in symptomatic children aged 0 to 11 years with uncomplicated malaria, there were 101 isolates, of which 60 were male and 41 were female. In this study, children in the age groups of > 4 and 8 recorded the largest number of genotypes (MOI = 1.8), followed closely by children between the ages of 0 and 4 years (MOI = 1.6), suggesting that genetic diversity and infection multiplicity appear to be age-dependent (Table 1). The smallest MOI, 1.3, was found in the oldest group. The genetic diversity in the urban districts of Lagos was examined for a period of 2 months in the study by Oyebola et al. [36]. To determine the variety of the surface proteins on merozoites 1 and 2, only 105 of the original 536 patients enrolled for the study from the two study locations (Lekki and Ikorodu) were found to be P. falciparum positive. The original sample size for the study was 536 individuals (260 men and 276 women). However, from the two study sites, only 100 positive samples were picked at random. Both study sites had the same prevalence of msp-1 polyclonal infections and both appeared to exhibit different patterns of msp-2 polyclonally. Oboh et al. [34] studied pregnant women between the ages of 17 and 42 years old for genetic variation of Merozoite surface protein-1 and 2. To provide a better idea of the genetic variation within the group, the pregnant group was compared to a non-pregnant group. 414 of the 425 pregnant women who were selected for the study had malaria, according to the results. Only 24 (or 5.8%) of the 414 samples taken from pregnant women tested positive for P. falciparum, and the 24 positive non-pregnant samples were also tested for MSP-1 and MSP-2. Fewer individuals in both groups were exposed to MSP-1 and MSP-2 isolates, which exhibited minor infection rates in both (1.05 and 1.15 for pregnant and non-pregnant individuals, respectively) (1.07 and 1.25). In comparison to isolates from pregnant women, the multiplicity of MSP-1 and MSP-2 infection was somewhat higher (1.15 and 1.25, respectively) in isolates from non-pregnant women (1.05 and 1.07, respectively).
Amodu et al. [41] reported the genetic diversity of P. falciparum in children by classifying the severity of malaria (asymptomatic, uncomplicated, and severe malaria), and the marker used for the study is MSP-1. The study's sample consisted of 223 children, of which 95 (43%) were girls and 128 (57%) were boys. In accordance with WHO guidelines, 101 cases of acute, uncomplicated malaria, 69 cases of severe malaria anemia, and 53 cases of asymptomatic malaria were identified. According to the msp 1 alleles (MAD 20, K1, and RO33) analysis, there is a substantial difference between the three groups. More alleles were found in the asymptomatic group than in the other two groups, by a factor of three.
Limited studies on GLURP and microsatellite markers
Glutamate rich protein (GLURP)
Glutamate-rich protein (GLURP) is an antigen of P. falciparum. It is present in all stages of the malaria parasite [48] and has been reported to induce clinical immunity. The glurp gene comprises basically three key regions; conserved or region, a centra repeat fragment (R1 region), and C- terminal immune dominant repeat region (R2 fragments). The R2 fragment is polymorphic and possesses two B- cell epitopes [28]. Urbanization may play a major role in a lower number of glurp genes obtained in an urban center in southwest Nigeria, these low GLURP values may be indicative of high transmission density. Another key factor may be changed in parasite genome occurring at a faster pace in rural areas than urban areas [28]. The GLURP exhibits a high level of gene conservation, making it an excellent candidate for a vaccine [49]. Extensive diversity was reported in the parasite populations in the four zones in Ogun state, South-Western Nigeria, obtained by the glurp gene, msp 1, and msp 2. Multiclonality is also observed in these zones. Multiclonality of infections has been shown to be recurrent in most malaria-endemic [50].
According to a study by Funwei et al. [28], the glurp gene's RII region showed 12 different allelic fragment sizes, of which 11 were identified in rural regions and six in cities, and showed a considerable amount of variation in the parasite population. In contrast to the urban area, the rural area had a lower frequency of glurp alleles. This could indicate that the transmission intensity was higher there and that significant changes to the parasite's genome happened there more swiftly than in the urban area.
The impact of ACT was reported by Nguetse et al. [58] between the years 2004 (group A) and 2015 (group B). Despite the use of new intervention measures, the MOI climbed somewhat in 2015 but not dramatically (MOI 2004: 1.23 against MOI 2015: 1.47), indicating that there has not been any appreciable decrease in malaria transmission rates throughout this time period. In a location with a high malaria endemicity, a substantial number of glurp alleles (11 in Group B and 12 in Group A) is anticipated. The size of the parasite population undoubtedly supports their presence [59]. Among the parasite population studied by Ikegbunam et al. [57], the glurp genes were observed to occur highest in pregnant women when compared to other adults notably compared to the MOI. This observation may be attributed to the fact that the pregnant group is usually asymptomatic of the malaria parasite [57].
Microsatellite marker
Microsatellite markers are used to evaluate population genetic structure. These markers are thought to be mostly a result of demographic events rather than selection acting on these populations. Microsatellite loci have been suggested to be excellent alternatives to msp-1, msp-2, and glurp due to their abundance, putative neutrality, and higher levels of polymorphisms [51]. MSP-1 and MSP-2 present some limitations, viz.; these markers are often under intense immune pressure and population structure and transmission patterns observed by using these methods may appear masked or distorted [52,53,54]. In previous studies that employed the use of microsatellite analyses, it was observed that parasites from areas of low malaria transmission (< 1% infection) have less genetic diversity but more population structure and greater linkage disequilibrium [55]. Comparison of a given population to that of microsatellites is thus a way to detect selection. Indices of genetic diversity and differentiation such as multiplicity of infection (MOI), and expected heterozygosity are important predictive markers of the intensity of transmission [56]. Ajogbasile et al. [16] reported that the estimated expected heterozygosity values were high, ranging from 0.776 to 0.842 in all nine States observed by microsatellite analysis. This is comparable to cases that have been recorded in other malaria-endemic nations [60–62]. This emphasizes the study's prior finding of substantial parasite genetic diversity and nationwide parasite transmission. (Table 3 and 4).
Conclusion
It is conceivable that the observed differences in the most common msp genes between studies are due to immune selection pressure in various study locations, as the immune system can influence parasite antigen selection. The patterns of variability seen in different parts of the country suggest that different treatment techniques may be required to combat malaria in different zones. To strengthen eradication efforts, more research on the impact of diverse allelic distributions on treatment response is needed. This is an area that has received sparse attention in Nigerian studies but may have a substantial impact on the development of novel therapeutic options.
Limitations
A major limitation of this review is the paucity of research publications on the subject. No data on msp1 or msp2 allelic diversity was found in the North-East, South-East, and South-South zones, while data for the North-West were derived from few publications. Future research examining the parasite diversity in these areas will help in drawing a more holistic picture of the genetic diversity of P. falciparum in Nigeria. There is also a need to conduct these studies periodically in the same regions in order to understand shifts in genetic diversity over time or seasons. This may even reveal the reasons for the discrepant results from the same region. Another limitation of the review was the prevalent use of agarose gel electrophoresis for PCR detection. While agarose gel electrophoresis is effective, more novel techniques, involving capillary electrophoresis and genome-wide studies, may identify genetic peculiarities in malaria-infected populations more accurately.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
World malaria report (2021) Geneva: World health organization; License: CC BY-NC-SA 3.0 IGO
White NJ, Pukrittayakamee S, Hien TT, Faiz MA, Mokuolu OA et al (2014) Malaria. Lancet 383(9918):723–735
Abukari Z, Okonu R, Nyarko SB, Lo AC, Dieng CC et al (2019) The diversity, multiplicity of infection, and population structure of P. falciparum parasites circulating in asymptomatic carriers living in high and low malaria transmission settings of Ghana. Genes 10(6):434
Conway DJ, Roper C, Oduola AMJ, Arnot DE, Kremsner PG et al (1999) High recombination rate in natural populations of Plasmodium falciparum. PNAS USA 96:4506–4511
Kolakovich KA, Ssengoba A, Wojcik K, Tsuboi T, Al-Yaman F et al (1996) Plasmodium vivax: favored gene frequencies of the merozoite surface protein-1 and the multiplicity of infection in a malaria endemic region. Exp Parasitol 83(1):11–19
Woehlbier U, Epp C, Hackett F, Blackman MJ, Bujard H (2010) Antibodies against multiple merozoite surface antigens of the human malaria parasite Plasmodium falciparum inhibit parasite maturation and red blood cell invasion. Malar J 18(9):77
Deitsch KW, Chitnis CE (2012) Molecular basis of severe malaria. PNAS-USA109 (26): 10130–10131.
Beeson JG, Drew DR, Boyle MJ, Feng G, Fowkes FJ et al (2016) Merozoite surface proteins in red blood cell invasion, immunity, and vaccines against malaria. FEMS Microbiol Rev 40(3):343–372
Peyerl-Hoffmann G, Jelinek T, Kilian A, Kabagambe G, Metzger WG et al (2001) Genetic diversity of Plasmodium falciparum and its relationship to parasite density in an area with different malaria endemicities in west Uganda. Trop Med Int Health 6:607–613
Holder AA, Blackman MJ, Burghaus PA, Chappel JA, Ling IT et al (1992) Malaria merozoite surface protein (MSP1)-structure processing and function. Mem Inst Oswaldo Cruz 87(3):37
John CC, Park GS, Sam-Agudu N, Opoka RO, Boivin MJ (2008) Elevated serum levels of IL-1ra in children with Plasmodium falciparum is associated with increased severity of disease. Cytokine 41:204–208
Gilson PR, Nebl T, Vukcevic D, Moritz RL, Sargeant T et al (2006) Identification and stoichiometry of Glycosylphosphatidylinositol-anchored membrane protein of the human malaria parasite Plasmodium falciparum. Mol Cell Proteom 5(7):1286–1299
Kiwanuka GN (2009) Genetic diversity in Plasmodium falciparum merozoite surface protein 1and 2 coding genes and its limitation in malaria epidemiology: a review of published studies from 1997–2007. J Vector Borne Dis 46(1):1–12
Mohammed H, Hassen K, Assefa A, Mekete K, Tadesse G (2019) Genetic diversity of Plasmodium falciparum isolates from patients with uncomplicated and severe malaria based on msp-1 and msp-2 genes in Gublak. Northwest Ethiopia Malar J 18:413
Usman-Yamman H, Omalu CJ, Abubakar A, Abolarinwa SO, Eke SS et al (2021) Genetic diversity of Plasmodium falciparum isolates in Minna, North Central Nigeria inferred by PCR genotyping of Merozoite surface protein 1 and 2. Infect Genet Evol 96:105143
Ajogbasile FV, Kayode AT, Oluniyi PE, Akano KO, Uwanibe JN et al (2021) Genetic diversity and population structure of Plasmodium falciparum in Nigeria: insights from microsatellite loci analysis. Malar J 20:236
Ashley EA, Pyae PA, Woodrow CJ (2018) Malaria. Lancet 391(10130):1608–1621
Oyedeji SI, Awobode HO, Kun J (2013) Limited genetic diversity and low multiplicity of Plasmodium falciparum infections in children with severe malaria in Lafia. North-central Nigeria J Exp Clin Med 5(4):143–147
Dikwa KB, Yahaya UA, Suleiman MDB, AB, (2020) Diversity of Plasmodium falciparum isolated from symptomatic and asymptomatic individuals in parts of kaduna metropolis. Kaduna state Am J Microbiol Res 8(3):83–92
Mayengue PL, Ndounga M, Malonga FV, Bitemo M, Ntoumi F (2011) Genetic polymorphism of merozoite surface protein-1 and merozoite surface protein-2 in Plasmodium falciparum isolates from Brazzaville. Republic of Congo Malar J 10:276
Mwingira F, Nkwengulila G, Schoepflin S, Sumari D, Beck HP et al (2011) Plasmodium falciparum msp1, msp2, and glurp allele frequency and diversity in sub-Saharan Africa. Malar J 10:79
Soe TN, Wu Y, Tun MW, Xu X, Hu Y et al (2017) Genetic diversity of Plasmodium falciparum populations in southeast and western Myanmar. Parasite Vectors 10:322
Oyedeji SI, Awobode HO, Anumudu C, Kun J (2013) Genetic diversity of Plasmodium falciparum isolates from naturally infected children in north-central Nigeria using the merozoite surface protein-2 as molecular marker. Asian Pac J Trop Med 6(8):589–594
Oyedeji SI, Bassi PU, Oyedeji SA, Ojurongbe O, Awobode HO (2020) Genetic diversity and complexity of Plasmodium falciparum infections in the microenvironment among siblings of the same household in North-central Nigeria. Malar J 19:338
Amodu OK, Olaniyan SA, Omotade OO (2015) Changes in Plasmodium falciparum population dynamics in two populations at different time periods in Ibadan, Southwest Nigeria. Afr J Biomed Res 18:17–22
Abiodun IB, Oluwadun A, Ayoola AO, Olusola IS (2016) Plasmodium falciparum Merozoite surface protein-1 polymorphism among asymptomatic sickle cell anaemia patients in Nigeria. Acta Med Iran 54(1):45
Chang HH, Childs LM, Buckee CO (2016) Variation in infection length and super-infection enhance selection efficiency in the human malaria parasite. Sci Rep 6:26370
Funwei RA, Thomas BN, Falade CO, Ojurongbe O (2018) Extensive diversity in allelic frequency of Plasmodium falciparum merozoite surface proteins and glutamate-rich protein in rural and urban settings of southwestern Nigeria. Malar J. https://doi.org/10.1186/s12936-017-2149-5
Miles A, Iqbal Z, Vauterin P, Pearson R, Campino S et al (2016) Indels, structural variation, and recombination drive genomic diversity in Plasmodium falciparum. Genome Res 26:1288–1299
Idakwo J, Idowu, ET, Oyebola KM, Otubanjo OA (2018) Low levels of Plasmodium falciparum genetic diversity in two Nigerian communities bordering the Niger River. Pan Afri J life Sci https://doi.org/10.36108/pajols/8102/10(0130).
Kolawole OM, Mokuolu OA, Olukosi YA, Oloyede TO (2016) Population genomics diversity of Plasmodium falciparum in malaria patients attending Okelele health centre, Okelele, Ilorin, Kwara State. Nigeria Afr Health Sci 16(3):704
Happi CT, Gbotosho GO, Sowumi A, Falade CO, Akinboye DO et al (2004) Molecular analysis of Plasmodium falciparum recrudescent malaria infections in children treated with chloroquine in Nigeria. Am J Trop Med 70(1):20–26
Ngoundou-Landji J, Nwuba RI, Anumudu CI, Odaibo AB, Maya WD et al (2010) Fine specificity of anti-MSP119 antibodies and multiplicity of Plasmodium falciparum Merozoite Surface Protein 1 types in individuals in Nigeria with sub-microscopic infection. Malaria J 9:287
Oboh MA, Idowu ET, Oyebola MK, Olukosi YA, Otubanjo OA et al (2017) Genetic diversity of Plasmodium falciparum among pregnant women in South-west Nigeria. Niger J Parasitol 38(1):104
Olasehinde Gl, Yah CS, Singh R, Ojurongbe OO, Ajayi AA, et al (2012). Genetic diversity of Plasmodium falciparum field isolates from southwestern Nigeria. Afr Health Sci 12(3):355–361
Oyebola MK, Idowu ET, Olukosi YA, Iwalokun BA, Agomo CA et al (2014) Genetic diversity and complexity of Plasmodium falciparum infections in Lagos. Nigeria Asian Pac J Trop Biomed 4(1):87–91
Sondo P, Derra K, Rouamba T, Diallo SN, Taconet P et al (2020) Determinants of Plasmodium falciparum multiplicity of infection and genetic diversity in Burkina Faso. Parasites Vectors 13:427
Tusting LS, Bousema T, Smith DL, Drakeley C (2014) Measuring changes in Plasmodium falciparum transmission: precision, accuracy, and costs of metrics. Adv Parasitol 84:151–208
Lum JK, Kaneko A, Taleo G, Amos M, Reiff DM (2007) Genetic diversity and gene flow of humans, Plasmodium falciparum, and Anopheles farauti of Vanuatu: inferred malaria dispersal implications for malaria control. Acta Tropical 103:102–107
Ajibaye O, Osuntoki AA, Ebuehi AO, Iwalokun EA, Balogun EO et al (2017) Pro- inflammatory cytokine response and genetic diversity in merozoite surface protein 2 of Plasmodium falciparum isolate from Nigeria. Adv Biomed Res 6:142
Amodu OK, Adeyemo OO, Ayoola OO, Gbadegesin AE, Orimadegun AK et al (2005) Genetic diversity of msp-1 locus and symptomatic malaria in southwest Nigeria. Acta Trop 95(3):226–232
Ojurongbe O, Fagbenro-Beyioku AF, Adeyeba OA, Kun JF (2011) Allelic diversity of merozoite surface protein 2 genes of P. falciparum among children in osogbo Nigeria. West Indian Med J 60(10):19
Ibara-Okabande R, Koukouikila-Koussounda F, Ndounga M, Vouvoungui J, Malonga V et al (2012) Reduction of multiplicity of infections but no change in msp2 genetic diversity in Plasmodium falciparum isolates from Congolese children after introduction of artemisinin combination therapy. Malar J 11:410
Chen I, Clarke SE, Gosling R, Hamainza B, Killeen G et al (2016) “Asymptomatic” malaria: a chronic and debilitating infection that should be treated. PLoS Med 13(1):e1001942
Ofosu-Okyere A, Mackinnon MJ, Sowa MPK, Koram KA, Nkrumah F et al (2001) Novel Plasmodium falciparum clones and rising clone multiplicities are associated with the increase in malaria morbidity in Ghanaian children during the transition into the high transmission season. Parasitol 12:113–123
Okungbowa MAO (2016) Prevalence and distribution of malaria and msp genes in Benin metropolis Edo state, Nigeria. UNIBEN J Sci Technol 4(1):1–10
Longdet IY, Kutshik RJ, Yakubu B, Ngutur PG (2019) Frequency of the FC 27 allelic family of merozoite surface protein 2 gene signifies highly virulent strain of Plasmodium falciparum in Jos. Nigeria Int J Life Sci Res 7(2):105–110
deStricker K, Vuust J, Jepsen S, Oeuvray C, Theisen M (2000) Conservation and heterogeneity of the glutamate-rich protein (GLURP) among field isolates and laboratory lines of Plasmodium falciparum. Mol Biochem Parasitol 111:123–130
Duru KC, Thomas BN (2014) Genetic diversity and allelic frequency of glutamate-rich protein (GLURP) in Plasmodium falciparum Isolates from Sub-Saharan Africa. Microbiol Insights 7:35–39
Happi TC, Thomas SM, Falade GGO, CO, Akinboye DO, et al (2003) Point mutations in the pfcrt and pfmdr-1 genes of Plasmodium falciparum and clinical response to chloroquine, among malaria patients from Nigeria. Ann Trop Med Parasitol 97:439–451
Mobegi VA, Loua KM, Ahouidi AD, Satoguina J, NwakanmaDC, et al (2012) Population genetic structure of Plasmodium falciparum across a region of diverse endemicity in West Africa. Malar J 11:223
Hughes AL (1992) Positive selection and interallelic recombination at themerozoitesurface antigen-1 (MSA-1) locus of Plasmodium falciparum. Mol Biol Evol 9:381–393
Hughes MK, Hughes AL (1995) Natural selection on Plasmodium surface proteins. Mol Biochem Parasitol 71:99–113
Escalante AA, Lal AA, Ayala FJ (1998) Genetic polymorphism and natural selection in the malaria parasite Plasmodium falciparum. Genetics 149:189–202
Anderson TJ, Haubold B, Williams JT, Estrada-Franco JG, Richardson L et al (2000) Microsatellite markers reveal a spectrum of population structures in the malaria parasite Plasmodium falciparum. Mol Biol Evol 17:1467–1482
Arnot D (1998) Unstable malaria in Sudan: the influence of the dry season. Clone multiplicity of Plasmodium falciparum infections in individuals exposed to variable levels of disease transmission. Trans R Soc Trop Med Hyg 92:580–585
Ikegbunam MN, Anagu LO, Duru C, Nworu CS, Esimone CO (2022) Genetic diversity and allelic frequency of antigenic markers in Plasmodium falciparum isolates from Nnewi district in Nigeria. J Infect Dev Ctries 16(3):557–563
Nguetse CN, Ojo JA, Nchotebah C, Ikegbunam MN, Meyer CG, Thomas BN et al (2018) Genetic diversity of the Plasmodium falciparum glutamate-rich protein R2 region before and twelve years after introduction of artemisinin combination therapies among febrile children in Nigeria. Am J Trop Med Hyg 98(3):667–676
Yuan L, Zhao H, Wu L, Li X, Parker D, Xu S, Zhao Y, Feng G, Wang Y, Yan G, Fan Q, Yang Z, Cui L (2013) Plasmodium falciparum populations from northeastern Myanmar display high levels of genetic diversity at multiple antigenic loci. Acta Trop 125:53–59
Mulenge FM, Hunja CW, Magiri E, Culleton R, Kaneko A, Aman RA (2016) Genetic diversity and population structure of Plasmodium falciparum in Lake Victoria Islands, a region of intense transmission. Am J Trop Med Hyg 95:1077–1085
Conway DJ, Machado RL, Singh B, Dessert P, Mikes ZS, Povoa MM et al (2001) Extreme geographical fixation of variation in the Plasmodium falciparum gamete surface protein gene Pfs48/45 compared with microsatellite loci. Mol Biochem Parasitol 115:145–156
Durand P, Michalakis Y, Cestier S, Oury B, Leclerc MC, Tibayrenc M et al (2003) Significant linkage disequilibrium and high genetic diversity in a population of Plasmodium falciparum from an area (Republic of the Congo) highly endemic for malaria. Am J Trop Med Hyg 68:345–349
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AOO, JAA, and ATA conceived the review. AOO, JAA, AOF, AKO, and ATA were involved in search strategy and drafting. ATA supervised the review and revised and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Opute, A.O., Akinkunmi, J.A., Funsho, A.O. et al. Genetic diversity of Plasmodium falciparum isolates in Nigeria. A review. Egypt J Med Hum Genet 23, 129 (2022). https://doi.org/10.1186/s43042-022-00340-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00340-7