Abstract
Background and aims
Gestational diabetes mellitus is well-defined as glucose intolerance first documented during pregnancy. In this study, we examined the possible associations between I/D polymorphism of the angiotensin-converting enzyme gene, the M235T variant of angiotensinogen gene, and the rs7950226 polymorphism of the ARNT-like protein-1 (BMAL1) gene and the risk for diabetes in Egyptian pregnant women.
Subjects and methods
This study recruited 160 gestational diabetes cases and 165 controls. Genomic DNA was derived from peripheral blood leukocytes and ACE gene (I/D) genotyping was performed using the method of polymerase chain reaction and the polymerase chain reaction-based restriction fragment length polymorphism was used for identifying the M235T variant of AGT gene and the rs7950226 polymorphism of the BMAL1.
Results
The II, ID, and DD genotypes of the ACE gene have significant differences in cases compared to controls (P = 0.000 and X2 = 81.77). The M235T polymorphism of the AGT gene was increased with gestational diabetes risk. Furthermore, the AA genotype of the BMAL1 rs7950226 gene was significantly related to the gestational diabetes risk (P = 0.000 and X2 = 52.82). Furthermore, the allele frequencies of the three variants have significant variances between cases and control.
Conclusion
This study suggested significant associations between ACE (DD), AGT (TT), and BMAL1 rs7950226 (AA) gene polymorphisms with gestational diabetes susceptibility and there was a possibility to identify that II + MM + GG as protective haplotypes and DD + TT + AA as risk haplotypes for gestational diabetes.
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) is considered an important adverse side effect in pregnancy, in which women no known to have diabetes develop hyperglycemia during pregnancy [1]. In most cases, chronic insulin resistance and pancreatic β-cell dysfunction result from impaired glucose tolerance and hyperglycemia. GDM risk factors include advanced maternal age, overweight and obesity, and diabetic family history [2]. GDM pathophysiological changes are similar to those in type 2 diabetes mellitus (T2DM) [2]. Accordingly, an interaction between GDM and T2DM is recognized, in which multiple genetic polymorphisms previously reported as risk factors for T2DM are found to increase GDM risk. Those gene polymorphisms are involved in glucose metabolism, insulin secretion, and resistance. Women who suffered from GDM before are at increased risk by seven folds to have T2DM postpartum compared with those who did not have GDM [3].
In normal pregnancy, cardiovascular system changes observed are due to appropriate adaptation to the renin–angiotensin system (RAS) [4]. Angiotensinogen (AGT) is converted to angiotensin I by renin and consequently to angiotensin II, which is more potent, by angiotensin-converting enzyme (ACE). ACE inactivates bradykinin, which has a major effect on the inflammatory process [5]. Moreover, the ACE gene is an important gene and T2DM is one of its abnormalities [6]. Other complications of ACE gene abnormality are end-stage renal disease [7], diabetic nephropathy [8], and gestational diabetes [9, 10]. ACE polymorphism strongly influences ACE activity, as about of total phenotypic plasma variant, 47% of them account for I/D (Insertion/Deletion) allele polymorphism of ACE. There is two times higher ACE activity in subjects with DD (Deletion/Deletion) allele than those with an II (Insertion/Insertion) allele [11]. Angiotensinogen is one of the most important components of the RAS, a single base pair substitution of thymine (T) with cytosine (C) leading to methionine with threonine substitution at position 235 is the gene mutation of M235T angiotensinogen [10]. AGT polymorphism was previously studied in the etiology of T2DM [12].
Recently, a relationship between circadian clock function and the T2DM development has been displayed. BMAL1 is a key component of the mammalian molecular clock. In humans, genetic variants in the ARNT like protein-1 (BMAL1) gene have been recognized to be related to T2DM susceptibility [13]. Despite previous studies, insufficient understood of the genetic history and the predisposition of GDM and given the fact that GDM shares many features with T2DM, so we studied the relationship of ACE (I/D), AGT (M235T), and the ARNT-like 1 (BMAL1, G/A) genetic variations or contributed haplotypes with the possibility of GDM development, in Egyptian pregnant women.
Subject and method
Study subjects
This case–control study was performed at the antenatal care clinic of the Medical Research Center of Excellence (MRCE), Reproductive Health and Family Planning Department, National Research Centre, Egypt. The study involved 325 midtrimester pregnant women: 160 women with GDM and 165 normal pregnant women with normal glucose levels. Selection, screening, and management of diabetes were done according to the criteria of the NICE guidelines [14].
Exclusion criteria were pregnancy with type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), hyper- or hypo-thyroidism, Cushing syndrome, cardiovascular disease, or cancer from the study.
All participants have signed written informed consent and the study had approval from the Ethical Committee of Medical Research at the National Research Centre (NRC).
Sample collection and DNA extraction
Fasting venous blood samples (5 ml) were collected into ethylenediaminetetraacetic acid (EDTA) tubes when conducting routine medical procedures via hospitalization during 24–28 weeks of gestation.
Clinical data and biochemical measurements
Clinical data and biochemical measurements of all subjects were obtained. For each subject we recorded age, weight, height, gestational duration, blood pressure, and family history of T2DM patients. Body mass index (BMI) was calculated as body weight (kg) divided by height square (m2).
The fasting plasma glucose (FPG) and glycosylated hemoglobin A1c (HbA1c) levels were measured using Stanbio Laboratory, USA. Serum human insulin levels were determined by enzyme-linked immunosorbent assays (ELISA) using kits from Immunospec. Corporation (USA) manufacturers’ instructions. Homeostatic Model assessment of insulin resistance (HOMA-IR) was calculated according to the formula: fasting insulin (μ U/L) x fasting glucose (mg/L)/22.5, using fasting values [15].
Isolation of genomic DNA
Genomic DNA was extracted from leukocytes of whole blood by QIA amplification extraction kit, QIAamp® DNA Blood Mini Kit Cat. No. 51104 according to the manufacturer's instructions; the isolated DNA was quantified via until use.
Genotyping of ACE (I/D) gene polymorphism
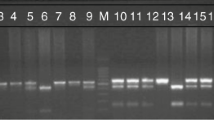
The ACE gene I/D polymorphism was identified using polymerase chain reaction (PCR) and suggested primer by [16]. The template DNA (0.5 μL) was amplified by following primers: forward 5-CTGGAGACCACTCCCATCCTTTCT-3 and reverse 5-GATGTCGCCATCACATTCGTCAGAT-3. The PCR amplifications were initial denaturation for 5 min at 95 °C; then 35 cycles of denaturation for 30 s at 94 °C, 30 s at 50 °C and extension for 1 min at 72 °C followed by a final extension cycle of 72 °C for 7 min (T-Gradient Thermal Cycler, Biometra, Germany. PCR products (190 bp for the deletion or 490 bp with insertion) were distinguished by electrophoresis on 3% agarose gel containing Fast green. An ultraviolet transilluminator was used to detect 490 bp and 190 bp fragments.
Genotyping of AGT (M235T) gene polymorphism
The AGT (M235T) gene polymorphisms were genotyped using a polymerase chain reaction/restriction fragment length polymorphism (PCR–RFLP) [17] via amplification with a forward primer 5-GATGCGCACAAGGTCCTG-3 and a reverse primer 5- CAGGGTGCTGTCCACACTGGCTCGC-3. The PCR conditions were 35 cycles of 1 min at 94 °C, 1 min at 61 °C, and 1 min at 72 °C, followed by a final extension at 72 °C for 7 min (T -Gradient Thermal Cycler, Biometra, Germany), and the products were digested by the restriction enzyme SfaNI (New England Biolabs); then, the restriction products was isolated on a 3% agarose gel. The appeared fragments of 266-bp and 303 bp were detected by ultraviolet transilluminator.
Genotyping of ARNT-like protein-1 (BMAL1) gene polymorphism
The rs7950226 polymorphism of the BMAL1 gene was investigated by using the PCR–RFLP method through amplifications with the forward primer 5-CATGCTGTGCTTGAATACTCCT-3 and the reverse primer 5- CTATGAAACCAAGGCTGAAACA-3 [13]. The 310-bp PCR product was digested by RsaI (New England Biolabs, Ipswich, MA) into two DNA fragments of 151 and 159 bp. The DNA fragments were isolated on a 3.5% agarose gel and detected by an ultraviolet.
transilluminator.
Statistical methods
All statistical analyses were achieved using SPSS 20.0. The statistical power and sample size were calculated by PASS 11. Variables were compared by ANOVA test and by the X2 test for categorical data between studied groups. Compared differences between allele frequencies and genotype distributions in patients with and without GDM were statistically processed using the Hardy–Weinberg equilibrium tests and the chi-square test (X2) or the Fisher’s exact test. The association between the genetic polymorphisms and some risk factors among GDM and controls were assessed using univariate analysis.
Results
Table 1 shows the genotype distribution of ACE, AGT (M235T), and ARNT (BMAL1) genes in cases and control group. The results revealed that there were significant change in the ACE (I/D), AGT M235T, and ARNT (G/A) gene polymorphisms among GDM women when compared to the controls, and the frequency of DD, TT, and AA genotypes was significantly higher in GDM (X2 = 81.77; P = 0.000, X2 = 109.83; P = 0.000 and X2 = 52.82; P = 0.000), respectively, when compared to controls.
The relationship between different genotypes of the ACE (I/D), AGT (M/T), and ARNT (G/A) and risk factors between GDM and controls are presented in Tables 2, 3, and 4, respectively. There are significant associations between the above-mentioned genes and some risk factors such as BMI, glucose, HBA1c, insulin, and HOMA-IR (as an index of diabetes) with a P value of 0.000. The risk of different variables of GDM depending on the genotypes of the above-mentioned genes is indicated in Table 5.
Gene–gene interactions
The results of gene–gene interactions using the stratification method and haplotype analysis are shown in Table 6. Haplotype analysis indicated the remarkably significant evidence of association with single-nucleotide polymorphism (SNP) combination ACE (DD), AGT (TT), and ARNT (AA) with GDM patients due to the decreased risk of the wild genotypes of ACE (II), AGT (MM), and ARNT (GG) in pregnant women with GDM (0%) as compared to controls (100%) with a P value of 0.001, OR 2.4, and 95% CI 1.229–4.688.
Discussion
Gestational diabetes mellitus (GDM) is supposed to have multifactorial causes; one of them may result from gene variations with the influence of some individual effects. GDM is supposed to have multifactorial causes; one of them may result from gene variations with the influence of some individual effects. For prediction, prevention, and management of GDM, genetic risk scores were implemented. These scores were derived from several genes and their single-nucleotide polymorphisms (functional polymorphisms) or haplotypes [18].
This study was conducted on pregnant Egyptian women with GDM; we have investigated the probable associations of ACE (I/D), AGT (M235T), and ARNT-like protein-1 (G/A) genetic variations with the risk of GDM. Though the actual mechanism of GDM development through gestation is still unknown, it could be recognized by increasing insulin resistance caused by maternal adiposity superimposed by the effect of insulin-desensitizing placental products as prolactin, estrogen, and human placental lactogen [19].
In an insertion/deletion (I/D) polymorphism of ACE gene with intron 16, 287-base pair Alu repetitive sequence is a common occurring variant [20]. This result indicated that the DD genotype and D allele of ACE was significantly associated with an increased risk of GDM.
Our results are in agreement with the present study by Dmitrenko et al. [21] who suggested a significant association between the DD homozygous type of ACE gene and GDM women with preeclampsia in the general inheritance model. This is, also, reported with a positive association in women of Brno and Indian population [22]. In the same line, a study by Khan et al. [19] in an Asian Indian population of pregnant women revealed the relationship between polymorphism of ACE (ID + DD) and the risk for GDM development. Alternatively, the frequency of DD genotype showed no significant difference among GDM patients in a Saudi population, and D allele frequency had a nonsignificant statistical difference between GDM and controls [23]. Moreover, Dostalova et al.[22] had one study in which polymorphism of ACE gene had no significant relation with GDM. ACE catalyzes the cleavage of the decapeptide angiotensin I to the octapeptide angiotensin II, which improves the vasoconstriction activity of the angiotensin [24]. ACE has a significant effect on the angiotensin II production not only in the circulating blood, but also on the synthesis and interaction of renin–angiotensin system (RAS) components, including in the beta cells of the Langerhans islets and the placenta [25]. Local RAS in the pancreas and the placenta are supposed to be involved in physiological and pathophysiological processes in pregnancy [26].
AGT gene encodes the precursor of all peptides of angiotensin. This gene is located on chromosome 1 (lq42-43) and has been considered as hypertension gene [27] and preeclampsia [28, 29]. To our knowledge, this study is the first one that evaluates the influence of this common SNP on GDM in Egyptian women. Our findings showed significant associations between the TT genotype and T allele of AGT and the risk of GDM. A study done by Ludwi et al. [30] suggested that T allele of AGT M235T polymorphism as an independent risk factor for CAD, while Gurkan et al. [31] findings did not support the idea that persons with T allele of AGT 235 gene will have high levels of AGT and so will yield more Ang. II, which lead to destruction of the tissue, as this genetic variant was more frequent in healthy subjects. Furthermore, we observed a significant correlation between the recessive model of AGT (MM + MT/ TT) with BMI, hypertension, and HOMA-IR. An earlier Japanese study was in agreement with our results, in which M235T reported a positive association with visceral obesity in obese women and T2DM morbid obese patients [32, 33]. M235T, also, has been investigated and showed a positive relation with T2DM in the Tunisian population [34]. Association between AGT rs699 and hypertension induced by pregnancy was investigated by another meta-analysis in the Chinese population. This meta-analysis found that the dominant genetic model (MT + TT) and the recessive genetic model (MT + MM) have significant associations [35]. Angiotensin II acts as a final hormone affecting the renin–angiotensin system. Its reactive production baseline can be increased by variants of angiotensinogen as M235T. Autoregulatory mechanisms could be provoked by continuous over-stimulation which leads to increase vascular tone and vascular hypertrophy. The sensitivity to angiotensin II then increased and the plasma levels of most angiotensinogen systems are reduced [36].
Strong evidence for the ARNT-like protein-I (BMALI) gene role has been provided in T2DM pathogenesis [37,38,39]. Given the genetic and pathophysiological feature's similarities between T2DM and GDM, in this study, we investigated the informative variants of the relationship between the BMAL1 gene and GDM in Egyptian women. GDM susceptibility knowledge is still limited, concerning genes or epigenetic alterations induced by glucose which occur during gestation, despite the wide spread of active research using genomic technologies [40]. This study provides evidence that the clock gene variants of the ARNT like the protein-1 (BMAL1) gene may be a predisposing factor to GDM in the Egyptian population. There was a positive association between the mutant genotype AA and A allele and the development of GDM. Circadian clock genes contribute to reproductive processes in mammals. BMAL1 plays an essential role in female reproduction [41].
Our findings were consistent with the previous studies conducted by Pappa et al.[13] who indicated for the first time that the rs7950226 (G > A) of the BMAL1 gene can be associated with increased GDM susceptibility. To our knowledge, these polymorphisms were found to be associated with T2DM in current studies by Kelly et al. [38], further increasing the list of sharing genetic parameters and common variants between GDM and T2DM. Also, the results are in agreement with Woon et al. [42] who reported T2DM patients independently, and found that the same polymorphisms in rs7950226 (G > A) were highly associated with T2DM susceptibility. However, our findings differ from Kelly et al. [38], who displayed that the haplotype of rs7950226A/rs11022775T of the BMAL1 gene has a positive association with T2DM.
The circadian clock distribution differences in gene polymorphism frequencies between populations worldwide were recently highlighted, giving us a powerful genetic component associated with the environment, not as a result of natural selection [43]. Specifically, the significant role of the clock genes, mainly BMAL1 in circadian self-keeping oscillations involved in glucose metabolism, growth, and pancreatic islets insulin signaling, has been recently underscored. These delayed phase oscillations when applied on mutant mice by conditional β-cell knockout lead to hyperinsulinemia and diabetes [37]. An early stage of dysfunction of β-cell may be reflected as a temporal derangement of the secretion of insulin. This also augments the clock (s) function of dynamic relation links in different tissues and increases the impact of disruption leading to T2DM [13].
As for the assumed GDM pathophysiological mechanisms that involve the clock genes, also regarding common features between both types of diabetes (T2DM and GDM) such as decreased insulin secretion and β-cell dysfunction, and increased insulin resistance during gestation, it is believable that the associated decrease in clock genes allele variants especially BMAL1 gene, as it was documented in this study, may increase the risk of GDM and glucose intolerance [39]. Besides, decreased susceptibility of the GDM alleles makes complementary β-cell mass increase [39, 40, 44]. The related deficiency of the allele variants of the clock genes and particularly of the BMAL1 gene, as recognized in our study, might further result in the increased risk of glucose intolerance and GDM.
Conclusion
Our results proposed that the ACE (I/D), AGT (M235T), and BMAL1 rs7950226 (G/A) gene polymorphisms might have an important role in GDM development in Egyptian pregnant women. In this study, it was possible to identify that II + MM + GG were the protective haplotypes for GDM while DD + TT + AA were the risk haplotypes for GDM. In the future, it could allow using this genetic marker as the principle in assessing the individual prediction of GDM development, which will assist to take efficient protective efforts for timely improvement in the pregnancy outcome.
Limitation
The limitation of this research study included the lack of evaluation of the ACE, AGT, and ARNT like protein-1 (BMAL1) levels and uses the only one SNP for each one. Studies with larger sample sizes are necessary to investigate the associations between gene polymorphisms and GDM in Egyptian populations.
Availability of data and material
The datasets supporting the results are included within the article. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available because of privacy or ethical restrictions.
Abbreviations
- ACE:
-
Angiotensin converting enzyme
- AGT (M235T):
-
Angiotensinogen
- BMAL1:
-
ARNT-like protein-1
- BMI:
-
Body mass index
- ELISA:
-
Enzyme-linked immunosorbent assays
- GDM:
-
Gestational diabetes mellitus
- HBA1c:
-
Glycated Hemoglobin
- HOMA-IR:
-
Homeostatic Model Assessment of Insulin Resistance
- OR:
-
Odds ratio
- T2DM:
-
Type 2 diabetes mellitus
- 95% CI:
-
95% Confidence Intervenes
References
American Diabetes Association Classification and Diagnosis of Diabetes (2018) Standards of medical care in diabetes-2018. Diabetes Care 41:S13–S27. https://doi.org/10.2337/dc18-S002
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH (2018) The pathophysiology of gestational diabetes mellitus. Int J Mol Sci 19(3342):1–21
Moon JH, Kwak SH, Jang HC (2017) Prevention of type 2 diabetes mellitus in women with previous gestational diabetes mellitus. Korean J Intern Med 32:26–41
Kusmierska-Urban K, Rytlewski K, Huras H (2015) Associations of ACE I/D and AGT M235T gene polymorphisms with the gestational hypertension and the fetal growth. Obstet Gynecol Int J 2(1):00026. https://doi.org/10.15406/ogij.2015.02.00026
Sparks MA, Crowley SD, Gurley SB, Mirotosu M, Coffman TM (2014) Classical Renin- Angiotensin system in kidney physiology. Compr Physiol 4(3):1201–1228
Al-Harbi EM, Farid EM, Gumaa KA, Singh J (2012) Genotypes and allele frequencies of angiotensin-converting enzyme (ACE) insertion/deletion polymorphism among Bahraini population with type 2 diabetes mellitus and related diseases. Mol Cell Biochem 362(1–2):219–223
Zhou TB, Yu ZY, Chen LS, Zhang LC (2012) Meta-analysis of the relationship between ACE I/D gene polymorphism and end stage renal disease in patients with diabetic nephropathy. Nephrology 17(5):480–487
Rahimi Z (2012) ACE insertion/deletion (I/D) polymorphism and diabetic nephropathy. J Nephropathol 1(3):143–151
Khan IA, Jahan P, Hasan Q, Rao P (2013) Angiotensin-converting enzyme gene insertion/ deletion polymorphism studies in Asian Indian pregnant women biochemically identifies gestational diabetes mellitus. J Renin Angiotensin Aldosterone Syst 15(4):566–571
Aggarwal P, Agarwa N, Das N, Dala K (2016) Association of polymorphisms in angiotensing converting enzyme gene with gestational diabetes mellitus in Indian women. Int J Appl Basic Med Res 6(1):31–37
Doria A, Patti ME, Kahn CR (2010) The emerging genetic architecture of type 2 diabetes. Cell Metab 16:1152–1156
Qiao Y, Wang M, Pan Y, Zhang X, Fang TF, Chen Y et al (2018) The relationship between ACE/AGT gene polymorphisms and the risk of diabetic retinopathy in Chinese patients with type 2 diabetes. J Renin-Angiotensin- Aldosterone Syst 19(1):1–8. https://doi.org/10.1177/1470320317752955
Pappa KI, Gazouli M, Anastasiou E, Iliodromiti Z, Antsaklis A, Anagnou NP (2013) The major circadian pacemaker ARNT-like protein-1 (BMAL1) is associated with susceptibility to gestational diabetes mellitus. Diabetes Res ClinPract 99(2):151–157
American Diabetes Association Classification and Diagnosis of Diabetes. Standards of Medical 2018.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Rigat B, Hubert C, Corvol P, Soubrier F (1992) PCR detection of the insertion/deletionpolymorphism of the human angiotensin converting enzyme gene (DCP1) (dipeptidyl carboxypeptidase 1). Nucleic Acids Res 20(6):1433. https://doi.org/10.1093/nar/20.6.1433-a
Caulfield M, Lavender P, Farrall M et al (1994) Linkage of the angiotensinogen gene to essential hypertension. N Engl J Med 330:1629–1633
Vrachnis N, Antonakopoulos N, Iliodromiti Z et al (2012) Impact ofmaternal diabetes on epigenetic modifications leading to diseasesin the offspring. Exp Diabetes Res 2012:538474. https://doi.org/10.1155/2012/538474
Khan IA, Movva S, Shaik NA, Chava S, Jahan P, Mukkavali KK et al (2013) Investigation of Calpain 10 (rs2975760) gene polymorphism in Asian Indians with gestational diabetes mellitus. Meta Gene 2:299–306
Chmaisse HN, Jammal M, Fakhoury H, Fakhoury R (2009) study on the association between angiotensin-I converting enzymeI/D dimorphism and type-2 diabetes mellitus. Saudi J Kidney Dis Transpl 20(6):1038–1046
Dmitrenko OP, Karpova NS, Nurbekov MK, Papysheva OV (2020) I/D Polymorphism Gene ACE and Risk of Preeclampsia in Women with Gestational Diabetes Mellitus. Dis Markers 7:1–7. https://doi.org/10.1155/2020/887523018
Dostalova Z, Bienertova-Vasku AJ, Vasku A, Gerychova R, Unzeitig V (2006) Insertion–deletion polymorphism in the gene for angiotensin-converning enzyme (I/D ACE) in pregnant womenwith gestational diabetes. CeskaGynekol 71(5):369–373
Saddick SY (2015) Angiotensin converting enzyme gene polymorphism studies: a case-control study. Saudi J Biol Sci 22:327–331
Vitoratos N, Hassiakos D, Iavazzo C (2012) Molecular mechanism of preeclampsia. J Pregnancy 298343:1–5
Herr D, Bekes I, Wulff C (2013) Local renin-angiotensin system in the reproductive system. Front Endocrinol 4:150. https://doi.org/10.3389/fendo.2013.00150
Spaan JJ, Brown MA (2012) Renin-angiotensin system in pre-eclampsia: everything old is new again. Obstetric Med Med Pregnancy 5(4):147–153
Yagil Y, Yagil C (2004) Candidate genes, association studies and haplotype analysis in the search for the genetic basis of hypertension. J Hypertens 22:1255–1258
Bernard N, Giguère Y (2003) Genetics of preeclampsia: What are the challenges? J Obstet Gynaecol Can 25:578–585
Yang J, Shang J, Zhang S, Li H, Liu H (2013) The role of the renin angiotensin-aldosterone system in preeclampsia: genetic polymorphisms and microRNA. J Mol Endocrinol 50:R53–R66
Ludwig EH, Borecki IB, Ellison RC, Folsom AR, Heiss G, Higgins M et al (1997) Associations between candidate loci angiotensin-converting enzyme and angiotensinogen with coronary heart disease and myocardial infarction: the NHLBI Family Heart Study. Ann Epidemiol 7:3–12
Gürkan A, Emingil G, Saygan BH, Atilla G, Köse T, Baylas H et al (2009) Angiotensin – converting enzyme (ACE), angiotensinogen (AGT), and angiotensin II type 1 receptor (AT1R) gene polymorphisms in generalized aggressive periodontitis. Arch Oral Biol 54(4):337–344. https://doi.org/10.1016/j.archoralbio.2008.12.005
Takakura Y, Yoshida T, Yoshioka K, Umekawa T, Kogure A, Toda H et al (2006) Angiotensinogen gene polymorphism (Met235Thr) influences visceral obesity and insulin resistance in obese Japanese women. Metabolism 55:819–824
Pacholczyk M, Ferenc T, Kowalski J, Adamczyk P, Chojnowski J, Ponikowska I (2015) Angiotensinogen gene M235T and T174M polymorphisms in patients with morbid obesity and type 2 diabetes mellitus. J Diabetes Metab 6(1):1–8. https://doi.org/10.4172/2155-6156.1000479
Mehri M, Koubaa N, Hammamia S, Mahjoub S, Chaaba R, Nakbi A, Zouari B et al (2010) Genotypic interactions of renin-angiotensin system genes with diabetes type 2 in a Tunisian population. Life Sci 87:49–54
Zhu M, Zhang J, Nie S, Yan W (2012) Associations of ACE I/D, AGT M235T gene polymorphisms with pregnancy induced hypertension in Chinese population: a meta-analysis. J Assist Reprod Genet 29:921–932. https://doi.org/10.1007/s10815-012-9800-4
Mutter WP, Karumanchi SA (2008) Molecular mechanisms of preeclampsia. Microvasc Res 75:1–8
Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH et al (2010) Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466:627–631
Kelly MA, Rees SD, Hydrie MZ, Shera AS, Bellary S, O’Hare JP, et al. Circadian gene variants and susceptibility to type 2 diabetes: a pilot study. PLoS ONE 2012; e32670.
Konig M, Shuldiner AR (2012) The genetic interface between gestational diabetes and type 2 diabetes. J Matern Fetal Neonatal Med 25:36–40
Watanabe RM (2012) Inherited destiny? Genetics and gestational diabetes mellitus. Genome Med 3:18
Pan X, Meredith J, Taylor MJ, Cohen E, Hanna N, Mota S (2020) Circadian clock, time-restricted feeding and reproduction. Int J Mol Sci 21:831. https://doi.org/10.3390/ijms21030831
Woon PY, Kaisaki PJ, Braganca J, Bihoreau MT, Levy JC, Farall M et al (2007) Aryl hydrocarbon receptor nuclear translocator-like (BMAL1) is associated with susceptibility to hypertension and type2 diabetes. Proc Nat Acad Sci USA 104:14412–14417
Ciarleglio CM, Ryckman KK, Servick SV, Hida A, Robbins S, Wells N et al (2008) Genetic differences in human circadian clock genes among worldwide populations. J Biol Rhythms 23:330–340
Lee J, Kim MS, Li R, Liu VY, Fu L, Moore DD et al (2011) Loss of Bmal1 leads to uncoupling and impaired glucose stimulated insulin secretion in b-cells. Islets 3:381–388
Acknowledgements
We thank the patients and volunteers who participated in this study
Funding
This work was supported by a grant from the National Research Centre, Egypt (Project Number 11010185).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: Esmat Ashour, Mie Afify, Olfat M. Fawzi. Diagnosis and selection of all participants in the study: Ahmed Okasha. Contributed reagents/materials/analysis tools: Weaam Gouda, Lamiaa Mageed and Esmat Ashour. Weaam Gouda, Lamiaa Mageed, Ahmed Okasha, and Esmat Ashour Contributed to the analysis of the results and the writing of the manuscript. All authors provided critical feedback and helped shape the research, analysis, and approved the final version submitted for the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Human Ethical Committee of the National Research Centre (The patient provided written consent).
Consent for publication
Written informed consent was obtained from all patients and controls.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ashour, E., Gouda, W., Mageed, L. et al. Association of gene polymorphisms of ACE, AGT, and ARNT-like protein 1 with susceptibility to gestational diabetes. Egypt J Med Hum Genet 23, 59 (2022). https://doi.org/10.1186/s43042-022-00273-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00273-1