Abstract
Purpose
The aim of this study was to investigate whether the degree of patellar cartilage loss confirmed during index surgery affects the clinical and radiologic outcomes of total knee arthroplasty (TKA) performed without patellar resurfacing.
Methods
We prospectively divided 2012 patients with a minimum follow-up of 12 months into two groups according to intraoperatively graded cartilage lesions graded using the International Cartilage Repair Society (ICRS) system: group 1, grades 0‒2 (n = 110); group 2, grades 3‒4 (n = 102). Relevant locations, such as medial, lateral, or both facets of the patella, were also assessed. Clinical outcomes were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index, Feller’s patella score, and Kujala anterior knee pain score. Radiographic outcomes included patellar tilt angle and lateral patellar shift on Merchant’s view.
Results
Clinical and radiographic outcomes were not significantly different between the two groups. No patient underwent secondary patellar resurfacing. Although the lateral facet was significantly more involved, there were no significant differences in outcomes.
Conclusions
The degree of intraoperatively identified patellar cartilage loss did not affect the short-term outcomes following primary TKA without patellar resurfacing.
Level of evidence II: Prospective comparative study.
Similar content being viewed by others
Introduction
Patellar resurfacing has been performed in approximately 35% of international joint registries during primary total knee arthroplasty (TKA) [1]. However, the management of the patella remains controversial. Although some surgeons have advocated for patellar resurfacing in terms of decreased postoperative anterior knee pain and risk of progressive patellar cartilage loss [2], many studies have reported that this procedure does not necessarily show superior outcomes [3,4,5]. Moreover, there is a lack of evidence that patellar cartilage loss identified during TKA causes anterior knee pain or decreased function [6]. Some studies have reported that there were no differences in outcomes between patients who underwent or did not undergo patellar resurfacing, regardless of the degree of patellar cartilage loss [7,8,9]. The authors of one study reported satisfactory radiologic outcomes with patellar retention in patients with grade 4 advanced osteoarthritis (OA) in the patellofemoral joint [10].
In addition, the reporting of adverse events associated with patellar resurfacing, including periprosthetic fracture, aseptic loosening, and infection, have recently led many surgeons to advocate patellar retention [6, 7, 10].
Although some retrospective studies have reported favorable outcomes of patellar retention during primary TKA [6, 7], there is a paucity of literature on the prospective outcomes of this procedure. Therefore, the purpose of this prospective study was to investigate whether the degree of patellar cartilage loss confirmed during index surgery affects the short-term clinical and radiologic outcomes of TKA performed without patellar resurfacing. Moreover, we sought to assess the differences in outcomes according to the involved facet of the patella. To this end, we asked two questions: (1) Does the degree of patellar cartilage loss identified during surgery affect the outcomes after primary TKA without patellar resurfacing? (2) Do the outcomes differ depending on the location of the involved facet of the patella? We hypothesized that patellar cartilage loss has no effect on the short-term follow-up outcomes in primary TKA. We also hypothesized that there would be no difference in outcomes depending on the location of the facet involved.
Methods
Patient demographic characteristics
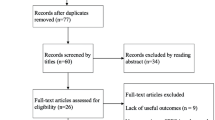
All patients participating in this study were asked for informed consent prior to enrollment. This prospective cohort study was approved by the Institutional Review Board of our hospital before patient data were retrieved (YUMC 2019-06-062-001). From July 2019 to April 2020, 221 knees which underwent consecutive primary TKA without patellar resurfacing were screened. We enrolled patients who were prospectively eligible for clinical and radiographic assessments with a minimum follow-up of 12 months after the index surgery. Patients with inflammatory arthritis (e.g., rheumatoid arthritis), previous surgery around the knee (e.g., arthroscopy, open reduction and internal fixation due to patellar fracture), and post-traumatic OA were excluded. Of the nine knees excluded, three were lost to follow-up, two had rheumatoid arthritis, two underwent arthroscopic surgery, one underwent surgery for patellar fracture, and one had post-traumatic OA. Among those patients who met the inclusion criteria, patients were classified according to the intraoperatively confirmed patella cartilage loss based on the International Cartilage Repair Society (ICRS) grading system [11]. Finally, to meet the minimum number of patients required for each group through the sample size calculation, we enrolled 212 knees in the study (Fig. 1).
Surgical techniques
All surgeries were performed by a senior surgeon using the same technique, namely, the modified gap-balancing technique which can balance the extension gap before the flexion gap using the posterior-stabilized gradually reducing radius femoral implant (Attune™; Depuy Synthes, Warsaw, IN, USA) [12, 13]. A medial parapatellar arthrotomy with a midline incision was performed. Femur sizing was performed using an anterior reference system in all cases. The rotation of the tibial component was set by considering several reference points, including the medial one-third of the tibial tuberosity, anterior tibial cortex, and floating technique. All prostheses were used with cement. Antioxidant polyethylene inserts were used in all cases.
No resurfacing of the patella occurred during surgery, regardless of the degree of patellar arthritic change and the original thickness of the patella. Patelloplasty was performed, which included the removal of marginal osteophytes, flattening of denuded facets, and circumferential denervation using electrocautery. Intraoperative patellar tracking was checked throughout the knee motion with the no thumb technique [14, 15].
A single closed suction drain was inserted after surgery and removed 24 h later. The perioperative pain control protocol was identical for all patients, including multimodal drug regimen, postoperative patient-controlled analgesia, and intraoperative periarticular injection. Active dangling exercise was initiated on the day of surgery, and partial weight-bearing was allowed on the first postoperative day. Full weight-bearing was permitted 3 weeks after surgery.
Intraoperatively confirmed cartilage loss of patella and grouping
The degree of cartilage loss of the patella was independently assessed by two orthopedic knee specialists during surgery using the ICRS grading system [11]. An assistant who was not involved in the operation recorded the assessment of each surgeon. If there was a disagreement between the two experts, the third orthopedic knee specialist made the final decision on the grading. We performed baseline surveys for the prospective collection of data with two concurrent cohorts of patients who were assigned to either group 1 (normal to mild cartilage loss; ICRS grades 0‒2; n = 110) or group 2 (moderate to severe cartilage loss, ICRS grades 3‒4, n = 102) (Fig. 2). For subgroup analysis, relevant locations, such as medial, lateral, or both facets of the patella, were assessed.
Outcome measures
Clinical and radiographic outcomes of each patient were assessed before surgery, at 6 weeks after surgery, and at 3, 6, and 12 months after surgery. Clinical outcomes were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score [16], Feller’s patella score [17], and the Kujala Anterior Knee Pain (AKP) score [18]. Reoperation related to secondary patellar resurfacing was also evaluated.
Radiographic outcomes included the patellar tilt angle and lateral patellar shift on Merchant’s view radiograph [19,20,21]. Lateral patellar tilt was defined as the angle between the line crossing the widest portion of the patella and the line passing through the anterior surfaces of both condyles. Lateral patellar shift was defined as the distance between the anterior-most point of the lateral femoral condyle and a line from the lateral edge of the patella perpendicular to the line that passed through the anterior surface of both condyles.
Statistical analysis
A power analysis (G* power software, version 3.1.7) was performed to calculate the number of patients needed in each group to identify the significant differences in clinical outcomes [power of 90%, α error of 0.05, and standard deviation (SD) of 10]. Eighty-five patients per group were required to identify significant differences. Ultimately, 102 patients were assigned to each group taking into account an estimated loss to follow-up of approximately 20%.
Statistical evaluation was performed using IBM SPSS software version 23 (IBM Corp., Armonk, NY, USA), and continuous data were expressed as the mean ± SD. All dependent variables were tested for normality of distribution and equality of variances using the Kolmogorov–Smirnov test and analyzed using parametric or non-parametric tests based on normality. An independent samples t-test (parametric) and Mann–Whitney U-test (non-parametric) were performed to assess the differences in clinical and radiographic variables between the two groups. Fisher’s exact test was used to compare the ratios between the groups. For subgroup analysis, the Kruskal–Wallis test was used to assess the differences among the three groups. Statistical significance was set at p < 0.05.
Reliabilities for the degree of cartilage loss were analyzed using intraclass correlation coefficients, and reliabilities were classified as little, if any (correlation coefficient ≤ 0.25), low (0.26–0.49), moderate (0.50–0.69), high (0.70–0.89), or very high (≥ 0.90) [22].
Results
The average age at surgery was 71.6 (range 60.0‒85.0) years, and the average follow-up period was 16.2 (range 12.0‒21.0) months. There were no significant differences in the demographic variables between the groups (Table 1).
Patellar cartilage loss was the highest in patellas assessed with ICRS grade 3 (28.8%) (Table 2). At 12 months after surgery, clinical outcomes, including WOMAC, Feller’s patella score, and Kujala AKP score, were not significantly different between the two groups (Fig. 3). After the index surgery, no significant difference was observed in radiographic outcomes, and there was no significant change during follow-up (Table 3). During the study period, no patient complained of anterior knee pain (AKP), and none of the patients underwent secondary patellar resurfacing. Although subgroup analyses were significantly more lateral among the relevant facets, they did not show significant differences in clinical outcomes (Fig. 4). Intraoperative agreement of the cartilage status showed very high intra- and inter-observer reliabilities (Table 4).
Clinical outcomes before surgery, at 6 weeks after surgery, and at 3, 6, and 12 months following TKA without patellar resurfacing. No statistically significant differences were observed between the two groups according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, Feller’s patella score, and the Kujala Anterior Knee Pain (AKP) score. Preop Preoperative
Discussion
The most notable finding of this study was that patients who underwent primary TKA without patellar resurfacing did not show significant differences in clinical and radiographic outcomes up to 2 years after surgery, regardless of the degree of patellar cartilage loss.
To the best of our knowledge, there is as yet no consensus on the optimal management of the patella during primary TKA. Some authors have advocated for a resurfacing procedure for patellas with an almost denuded cartilage [23, 24], while others have reported that patellar resurfacing fails to guarantee better outcomes even with deterioration of patellar cartilage [7, 8, 10]. In this study, we did not perform resurfacing even in those patellas with almost denuded cartilage. This decision was primarily due to the surgeon’s choice based on our hypothesis in this study.
Several adverse events associated with patellar resurfacing have been reported, including patellar fracture, osteonecrosis, extensor mechanism malalignment, and loosening or wear of the patellar component [25,26,27]. Moreover, some studies have reported that it was very difficult to restore patellar thickness and adequate patellar tracking [28]. Inappropriate patellar thickness may also affect patellofemoral overstuffing [29, 30], and a resultant thickness of < 12 mm after resection has an inherent risk of periprosthetic fracture [31,32,33].
Furthermore, with the exception of clinical and radiographic outcomes, our results showed that no patients complained of AKP or underwent additional secondary patella surfacing during an average follow-up period of 16.2 months. Some studies have reported an increased incidence of AKP after primary TKA in the absence of resurfacing [34, 35] and suggested secondary resurfacing as a rescue procedure [36, 37]. However, since AKP has multifactorial characteristics, it has been reported that the effect of secondary resurfacing is only 40‒50% relief of the symptoms [36]. The possibility of developing patella cartilage loss after primary TKA may also be a concern [38]. However, to the best of our knowledge, there is a paucity of literature on the subject of patella cartilage loss that develops several years after TKA; even if patella cartilage loss is progressive, it is difficult to conclude that such deterioration is associated with inferior clinical outcomes or worsening of AKP.
Despite the informative results of this study, the study does have a number of limitations that need to be considered. First, the relatively short follow-up period may be a major concern. Significant differences may have been missed because mid- to long-term outcomes were not assessed. However, some studies have reported that gradual cartilage loss of the patella was not necessarily observed after primary TKA in a time-dependent fashion [3, 7]. Furthermore, since several factors, including the femoral component, patellar height, and joint line, can influence deterioration of the patella cartilage, the time factor cannot be considered on its own. Second, since this study was not a comparative study with the group that had undergone patellar resurfacing, it is difficult to guarantee that non-resurfacing shows better results than resurfacing. Therefore, a comparative, randomized, prospective study is required to confirm that patellar retention can also provide favorable results regardless of the cartilage status of the patella. Third, other types of femoral components, such as cruciate retaining or single radius, were not considered. As reported, the trochlear geometry of the femoral component may vary with each design, and some are incompatible with the native patella [39, 40]. Therefore, the results may differ in patients treated with other types of femoral components. However, in this study, a single senior surgeon performed the surgery using the same implant with a patella-friendly design and gradual radius to minimize bias between patients. Finally, a female predominance was observed in this study. Thus, the same outcomes may not apply to populations with different sex ratios. However, OA is known to be more common in Asian women [41]. In particular, South Korean women have a five- to sevenfold higher rate of knee arthroplasty [42].
Conclusion
The degree of intraoperatively identified patellar cartilage loss did not affect the short-term outcomes following primary TKA without patellar resurfacing.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available, but they are available from the corresponding author on reasonable request.
References
Fraser JF, Spangehl MJ (2017) International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. J Arthroplasty 32(1):83–86
Patel K, Raut V (2011) Patella in total knee arthroplasty: to resurface or not to—a cohort study of staged bilateral total knee arthroplasty. Int Orthop 35(3):349–353
Burnett RSJ, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL (2009) Patellar resurfacing compared with nonresurfacing in total knee arthroplasty: a concise follow-up of a randomized trial. J Bone Joint Surg Am 91(11):2562–2567
Burnett R, Boone J, McCarthy K, Rosenzweig S, Barrack R (2007) A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res 464:65–72
Grassi A, Compagnoni R, Ferrua P, et al (2018) Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc 26(11):3206–3218
Park HJ, Chang MJ, Kim TW, Chang CB, Kang KS, Kang S-B (2021) Subchondral bone condition and intraoperative grading of cartilage degeneration underneath patella unrelated to the clinical outcome after TKA with unresurfaced patella. J Knee Surg. 2021. https://doi.org/10.1055/s-0041-1723980.
Cho W-J, Bin S-I, Kim J-M, Lee B-S, Sohn D-W, Kwon Y-H (2018) Total knee arthroplasty with patellar retention: the severity of patellofemoral osteoarthritis did not affect the clinical and radiographic outcomes. J Arthroplasty 33(7):2136–2140
Seo SS, Kim CW, Moon SW (2011) A comparison of patella retention versus resurfacing for moderate or severe patellar articular defects in total knee arthroplasty: minimum 5-year follow-up results. Knee Surg Relat Res 23(3):142
van Raaij TM, van der Meij E, de Vries AJ, van Raay JJ (2020) Patellar resurfacing does not improve clinical outcome in patients with symptomatic tricompartmental knee osteoarthritis. An RCT Study of 40 patients receiving primary cruciate retaining total knee arthroplasty. J Knee Surg 34:1503
Eshnazarov K, Seon J-K, Song E-K (2016) Comparison of radiological assessments patellar resurfacing with retention for grade IV osteoarthritis in patellofemoral joint accomplished total knee arthroplasty. Vestn Rentgenol Radiol 97(1):28–32
Mainil-Varlet P, Aigner T, Brittberg M, et al (2003) Histological assessment of cartilage repair: a report by the Histology Endpoint Committee of the International Cartilage Repair Society (ICRS). J Bone Joint Surg Am 85(suppl_2):45–57
Moro-oka T-a, Shiraishi H, Iwamoto Y, Banks SA (2010) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18(3):375–380
Daines BK, Dennis DA (2014) Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 6(1):1
Scott RD (1979) Prosthetic replacement of the patellofemoral joint. Orthop Clin North Am 10(1):129–137
Bindelglass DF, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty: implication for surgical technique. J Arthroplasty 11(5):507–511
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 5(12):1833-1840
Feller JA, Bartlett RJ, Lang DM (1996) Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 78(2):226–228
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9(2):159–163
Heesterbeek P, Beumers M, Jacobs W, Havinga M, Wymenga A (2007) A comparison of reproducibility of measurement techniques for patella position on axial radiographs after total knee arthroplasty. Knee 14(5):411–416
Laurin C, Dussault R, Levesque H (1979) The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res 144:16–26
Bito H, Takeuchi R, Kumagai K, Aratake M, Saito I, Hayashi R et al (2010) Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg Sports Traumatol Arthrosc 18(7):955–960
Munro BH (2005) Statistical methods for health care research. Philadelphia: Lippincott Williams and Wilkins
Roberts DW, Hayes TD, Tate CT, Lesko JP (2015) Selective patellar resurfacing in total knee arthroplasty: a prospective, randomized, double-blind study. J Arthroplasty 30(2):216–222
Rodríguez-Merchán EC, Gómez-Cardero P (2010) The outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res 468(5):1254–1257
Chalidis BE, Tsiridis E, Tragas AA, Stavrou Z, Giannoudis PV (2007) Management of periprosthetic patellar fractures: a systematic review of literature. Injury 38(6):714–724
Lindstrand A, Robertsson O, Lewold S, Toksvig-Larsen S (2001) The patella in total knee arthroplasty: resurfacing or nonresurfacing of patella. Knee Surg Sports Traumatol Arthrosc 9(1):S21–S23
Panni AS, Cerciello S, Del Regno C, Felici A, Vasso M (2014) Patellar resurfacing complications in total knee arthroplasty. Int Orthop 38(2):313–317
Pagnano M, Trousdale R (2000) Asymmetric patella resurfacing in total knee arthroplasty. Am J Knee Surg 13(4):228–233
Bracey DN, Brown ML, Beard HR et al (2015) Effects of patellofemoral overstuffing on knee flexion and patellar kinematics following total knee arthroplasty: a cadaveric study. Int Orthop 39(9):1715–1722
Kemp MA, Metcalfe AJ, Sayers A, Wylde V, Eldridge JD, Blom AW (2018) Does overstuffing of the patellofemoral joint in total knee arthroplasty have a significant effect on postoperative outcomes? Knee 25(5):874–881
Ortiguera CJ, Berry DJ (2002) Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am 84(4):532–540
Yoo JD, Kim NK (2015) Periprosthetic fractures following total knee arthroplasty. Knee Surg Relat Res 27(1):1
Parvizi J, Kim K-I, Oliashirazi A, Ong A, Sharkey PF (2006) Periprosthetic patellar fractures. Clin Orthop Relat Res 446:161–166
Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA (2005) Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res 438:191–196
Longo UG, Ciuffreda M, Mannering N, D’Andrea V, Cimmino M, Denaro V (2018) Patellar resurfacing in total knee arthroplasty: systematic review and meta-analysis. J Arthroplasty 33(2):620–632
Toro-Ibarguen AN, Navarro-Arribas R, Pretell-Mazzini J, Prada-Cañizares AC, Jara-Sánchez F (2016) Secondary patellar resurfacing as a rescue procedure for persistent anterior knee pain after primary total knee arthroplasty: do our patients really improve? J Arthroplasty 31(7):1539–1543
Grassi A, Compagnoni R, Ferrua P et al (2018) Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sport Traumatol Arthrosc 26(11):3206–3218
UK Department of Health. NICE Clinical Guideline NG157 (2020) Joint replacement (primary): hip, knee and shoulder. Methods.
Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E (2011) Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am 93(14):1301–1309
Maradit-Kremers H, Haque OJ, Kremers WK, et al (2017) Is selectively not resurfacing the patella an acceptable practice in primary total knee arthroplasty? J Arthroplasty 32(4):1143–1147
Vina ER, Kwoh CK (2018) Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol 30(2):160
Koh IJ, Kim MW, Kim JH, Han SY, In Y (2015) Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in Korea from 2009 to 2013. J Arthroplasty 30(6):939–944
Acknowledgements
Not applicable.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1A6A1A03040177).
Author information
Authors and Affiliations
Contributions
O-JS and GBK: conception and design of the study. O-JS: provision of study materials and/or patients. O-JS: acquisition of data. O-JS and GBK: analysis and interpretation of data. GBK: drafting of the article. O-JS and GBK: final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board. Informed consent was obtained from all patients prior to review.
Consent for publication
This manuscript is original and has not been submitted simultaneously to another journal. All authors participated in the research and agree with the contents of the manuscript. The authors undersigned hereby transfer, assign, and otherwise convey all copyright ownership to Knee Surgery & Related Research, and represent that the journal owns all rights to the material submitted.
Competing interests
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shon, OJ., Kim, G.B. Does the degree of intraoperatively identified cartilage loss affect the outcomes of primary total knee arthroplasty without patella resurfacing? A prospective comparative cohort study. Knee Surg & Relat Res 34, 36 (2022). https://doi.org/10.1186/s43019-022-00161-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-022-00161-3