Abstract
Background
The second-generation metaphyseal cone was useful in managing bone defects in revision knee arthroplasty. However, due to the anatomical constraints in Asian osteometry, the authors utilized a novel free-hand burring technique instead of cannulated reaming for bone preparation. We reported the short-term outcomes of our surgical techniques specific to Asian osteometry.
Methods
We conducted a case series by consecutively recruiting 13 female and 12 male patients (involving 25 knees), with a mean age of 71 years (range, 54–88 years). The patients underwent revision total knee arthroplasty during the period from April 2017 to June 2022. Twenty-three tibial cones and 4 femoral cones using free-hand burring technique were implanted. The mean follow-up duration was 51 months (range 18–80 months). Due to the relatively small bone size and meta-diaphyseal center mismatch in the Asian knees, the free-hand burring technique instead of the cannulated reaming technique was adopted in preparing for cone implantation. The clinical outcomes were knee ranges of motion, the Knee Society Knee scores (KSS), end-of-stem pain, infection, and the need for revision surgery. The radiological outcomes included osteointegration, fracture, and loosening.
Results
Mean knee range of motion improved from 83 degrees (range 0°–120°) preoperatively to 106 degrees (range 60°–125°) postoperatively (P < 0.001). Mean KSS improved significantly from 29 (range 0–70) to 69 (range 5–100) (P < 0.001). All cones were osteointegrated. One case had transient end-of-stem pain, two developed intraoperative minor femoral fractures and one suffered from recurrent infection that did not require cone revision. Cone revision-free survivorship was 100%. There was no aseptic loosening.
Conclusions
The second-generation cone implanted with free-hand burring bone preparation yielded promising short-term outcomes in Asian knees.
Similar content being viewed by others

Background
The demand for revision total knee arthroplasty (TKA) is on the rise with the aging population [1]. Management of bone loss in revision cases can be challenging. The Anderson Orthopaedic Research Institute (AORI) classification system is commonly adopted to classify bone defects [2]. Metaphyseal cone is useful in filling in the bone defect and improving metaphyseal fixation of the prosthesis, in compliance with the concept of zonal fixation [3].
The first-generation cone, despite the reported satisfactory outcomes, was associated with surgical difficulties in bony preparation by free-hand burring, which posed technical challenges and potential inaccuracy in conforming to the bone defect and osteometry. The recent advent of the second-generation cone is manufactured by three-dimensional printing according to a computed tomography-based anatomical database of a diverse population. It is made up of porous titanium to fit the geometry of the native tibia and femur. Bone preparation is streamlined into a cannulated-reaming system with precise sizing and morphology. It is relatively user-friendly and provides standardized bone preparation for implantation. From a biomechanical perspective, the new titanium cone has been verified to be non-inferior or even slightly superior to tantalum in withstanding physiological loading, with equal or fewer micromotions upon cyclical loading [4].
Only a limited number of European studies have been published to show encouraging short-term outcomes of second-generation titanium cone in revision TKA [5,6,7,8,9,10]. To the authors’ best knowledge, such data on the Asian population are still lacking. Therefore, we aimed to study the clinical and radiological outcomes of second-generation titanium cones in our Asian locality.
Methods
We reviewed 25 patients (13 females and 12 males, with 25 knees involved), who underwent revision total knee arthroplasty in our center during the period from April 2017 to June 2022. Our study was approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster, with the reference number UW 20-253. Informed consents were obtained from the patients, including consent for publication of the images in Figs. 1 and 4. Inclusion criteria were revision TKA using tibial and/or femoral second-generation titanium metaphyseal cones (Triathlon Tritanium Cone, TS Revision Knee System, Stryker, Mahwah, NJ, USA), implantation of which was prepared by free-hand burring techniques due to the anatomical constraints of the knees that precluded the use of cannulated reamer. Follow-up intervals were postoperative 2 weeks, 6 weeks, 3 months, 6 months then a year. The minimum follow-up duration lasted for 18 months, and the mean follow-up duration was 51 months (range 18–80 months).
Demographic data including age, gender, indication, and AORI classification were noted. Clinical outcomes recorded at the latest follow-up included knee range of motion, end-of-stem pain, Knee Society Knee Scores (KSS), infection, and any need for revision surgery. Osteointegration was assessed on serial postoperative radiographs, which were also scrutinized for any complications, including fracture, radiolucency, and aseptic loosening.
All revision TKA were performed by a single senior chief surgeon. The standard medial parapatellar approach was adopted in all cases. Implants were removed with maximal bone stock preservation. The bone defect was classified intraoperatively following implant removal, using the AORI classification (Fig. 1a). Class IIA and IIB defects were considered indicated for cone augmentation. No bone graft was used as cone was considered adequate in achieving metaphyseal structural support to allow initial mechanical stability for early weight-bearing. The tibia cut surface was assessed first to decide whether recut was needed, followed by the femoral side. Flexion and extension gap balancing were measured with the adjustable spacer block to help determine the appropriate insert thickness and joint line. Femoral rotation was determined with reference to gap balancing method. The joint line was restored, with femoral component distalization and augment in some cases.
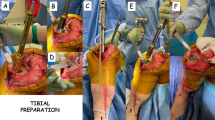
In preparing for cone implantation, cannulated reaming according to the second-generation cone manual was considered contraindicated in the included cases due to the anatomical mismatch between the metaphyseal center and diaphyseal center in those Asian knees. The reamer was guided directly onto the anterior tibial cortex in some cases (Fig. 1b). Instead, the free-hand burring technique was adopted for bone preparation in all cases, similar to the preparation for the first-generation cone (Fig. 1c). Steps of our surgical techniques were detailed as follows. An appropriately sized cone was chosen based on the bone defect and bone size. The proximal contour of the cone was marked on the proximal metaphyseal bone surface, followed by the depth and distal contour, according to the size of the cone. Using a 5-mm tip high-speed burr, the proximal bone surface was prepared in a centrifugal manner to match the marking. The bone was burred gradually from proximal to distal in order to match the contour of the cone (Fig. 1c). It was important to achieve press-fit by gradually increasing the burring surface radially outwards until the stability was tested satisfactory as indicated by the leg being lifted using a cone holder holding onto the implanted cone (Fig. 1d–e). The cone was considered stable if the leg could be lifted off the table with the cone holder without loosening the cone. If stability was inadequate, repeated burring and upsizing of the cone would be performed until adequate press-fit is achieved.
Triathlon revision knee system was implanted in conjunction with the cones in all cases (Fig. 2). Subsequently, mediolateral laxities were tested following trial implant insertion. Varus-valgus constrained implants with cemented stems were utilized in cases with significant residual mediolateral laxity, with their reported excellent mid-term survivorship [10]. Cone was then impacted to achieve press-fit, with satisfactory intraoperative axial and rotational stability. Stemmed knee prostheses were then cemented to the inner surface of the implanted cone, using antibiotics-loaded cement, ensuring joint line restoration. There was no need for offset stem in our case series. We used relatively small short stems to be cemented onto the implanted cones, allowing for adjustment to accommodate any meta-diaphyseal center mismatch.
Postoperatively, all patients were allowed to engage in immediate weight-bearing (full weight-bearing except for two cases with femoral fractures which were allowed protected weight-bearing for six weeks then full weight-bearing). All patients followed a standardized multidisciplinary rehabilitation protocol.
Results
A total of 27 cones were used in 25 knees of 25 patients (13 females and 12 males) receiving revision knee arthroplasty. The indications for revision knee arthroplasty were periprosthetic joint infection (13 out of 25), aseptic loosening (9 out of 25). The indications of the other 3 cases included postoperative knee stiffness, insert dislocation and PE wear. The mean age was 71 (range 54–88). Among the 27 cones, 23 were tibial and 4 were femoral. Two patients received simultaneous femoral and tibial cones. Of the 23 tibial cones, 18 were symmetrical and 5 were asymmetrical. Regarding the cone sizes, among tibial cones, 9 were size A (the smallest), 7 were size B, 4 were size C, 2 were size D and 1 was size E. All the femoral cones (Table 1) were size 1 & 2 (the smallest).
In all cases, the stem was cemented to the inner surface of the cone, with antibiotics-loaded cement. Cemented metaphyseal-engaging stems were utilized in all except one case requiring tibial tubercle osteotomy, in which a hybrid fixation with cemented metaphyseal and cementless diaphyseal-engaging stem was used. The tibial stem length used was 100 mm in 21 out of 25 cases, and 150 mm in the 4 remaining cases. Stem diameter was 12 mm in 15 cases, 10 mm in 6 cases, and 9 mm in 4 cases.
Mean knee range of motion improved from 83 degrees (range 0°–120°) preoperatively to 106 degrees (range 60°–125°) postoperatively (P < 0.001). Mean KSS improved significantly from 29 (range 0–70) to 69 (range 5–100) (P < 0.001). There was only one transient mild end-of-stem pain in a case with a 150 mm long cemented tibial stem, which resolved upon follow-up. Osteointegration was observed in all knees (Fig. 3).
Two intraoperative fractures occurred at anterior femoral cortices during femoral cone impaction and were treated with cerclage wires and protected weight-bearing. Subsequently, the fractures healed with cone osteointegration. One case required revision with debridement, antibiotics, and insert exchange with the cone retained, to treat the recurrent periprosthetic infection at 1.5 years after the two-stage revision with a tibial cone. No aseptic loosening was noted. Cone revision-free survivorship was 100%. There was one mortality unrelated to orthopaedic conditions at postoperative one year.
Discussion
The most important outcome of this study was that promising mid-term outcomes could be achieved by using free-hand burring technique to implant second-generation metaphyseal cone, despite the anatomical differences in Asian osteometry which limited the designated cannulated reaming bone preparation.
Several options are available for managing bone defects in revision total knee arthroplasty. For AORI Class I, i.e., contained defects, cement and screws are commonly adopted. With AORI Class IIA/B and III, there is a metaphyseal deficiency that hinders cement interdigitation. The classical technique of bone grafting, be it cancellous or structural allograft, bears its intrinsic risks of non-union, infection, and resorption [12]. Metallic augmentation in the forms of metaphyseal cone and sleeve is gaining popularity in recent years.
These two types of metal implants are based on different mechanisms. Each type of implant has its pros and cons. The sleeve is designed for use in conjunction with a revision prosthesis to improve axial rotational stability in metaphyseal bone defects. It requires sequential broaching to achieve press-fit. It is designed to be implanted with the prosthesis in one piece, and, hence, would not allow for independent adjustment of the sleeve and stem [13, 14]. On the other hand, cone allows independent metaphyseal fixation followed by cementation of the prosthesis inside the implanted cone to allow for more flexible joint line restoration and rotational adjustment [15, 16]. In particular, in our case series, we managed to use short small cemented stems within the cones for the flexibility to adjust for meta-diaphyseal center mismatch, hence not requiring the use of offset stem in all our cases. Both titanium sleeve and tantalum cone have been widely proven effective and durable in the current literature, with low rates of aseptic loosening [17,18,19].
First-generation tantalum cones have yielded excellent mid-term outcomes, with low rates of loosening and revision in multiple studies [15, 16, 20, 21]. However, the first-generation cones require free-hand burring for preparation, which is considered technically demanding and prone to inaccuracy. Furthermore, its applicability could be limited by the morphology and size of bone, due to a lack of precision in bone preparation and sizing. On the contrary, second-generation titanium metaphyseal cone is designed based on a CT anatomy database, using 3D printing technology [4]. It achieves technical efficiency by its designated cannulated reaming preparation, with improved accuracy in sizing and press-fit. These are technically advantageous to the surgeon as it allows streamlined preparation and accurate press-fit, which are lacking in the first-generation cone. The advancement of the second-generation cone has the theoretical potential to sharpen the biomechanical advantage of the previous generation while reducing the technical difficulty. However, only short-term results have been reported in the scarce literature (Table 2) [5,6,7,8,9,10]. Cemented stems were used in the vast majority of our cases as they allowed minor adjustments of implant position, potentially reduced end-of-stem pain, and minimized the risk of fracture as compared to cementless long stems, with no differences in loosening rate [11, 22].
Tetreault et al. reported one of the largest case series of 139 patients with 202 second-generation cones, yielding an excellent 2-year survivorship with 100% survivorship free of revision for aseptic loosening and 98% survivorship without cone revision [7]. Similarly, Chalmers et al. also reported, in their large series of 163 patients, an excellent 2-year survivorship without cone revision of 96%, and a survivorship free of revision for aseptic loosening of 100% [9]. Monárrez et al. reported a 96% overall cone revision-free survivorship in their 62 patients over a mean follow-up period of 2 years. [10] These studies verified the applicability of cannulated reaming preparation of cone in Caucasian patients with excellent short-term outcomes.
Our study was the first to report the implications of Asian osteometry on the surgical techniques for preparing for the second-generation titanium metaphyseal cone. First, the relatively small-sized tibial and femoral canals would accommodate only the smallest one to two sizes of implants for the majority of our cases. It could potentially predispose the bone to fracture during cone preparation and impaction as a result of bone-implant size mismatch. Furthermore, it is compounded by femoral and tibial bowing. Tang et al. and Yau et al. have respectively proven tibial and femoral bowing in both sagittal and coronal planes in Asian knees [23, 24]. Tang et al. found significant sagittal plane femoral bowing in the distal third of the femora in their radiographic study of 100 lower limbs of Chinese patients [23]. Yau et al., in their radiographic study of 92 Chinese lower limbs, reported significant coronal plane bowing, defined as more than 2 degrees, in 62% of the femurs, and 32% of the tibias [24]. These were considered risk factors for mal-alignment and fractures, hence necessitating long films for preoperative planning.
Moreover, meta-diaphyseal center mismatch was reportedly more prevalent in the Asian population, in which the center of tibia diaphysis is often offset from the metaphyseal center. In a more recent CT cross-sectional study by Tang et al., the center of the tibial plateau and the center of the tibia shaft were defined by locating the centers of the best-fitting rectangle and circle respectively in axial CT images, based on standardized anatomical landmarks. They concluded that in Chinese patients, the tibial shaft center was commonly anterolateral to the tibial plateau center, with the offset being more pronounced in male than female patients [25]. Our experience concurred with the phenomenon of meta-diaphyseal center mismatch found in the Asian population. As depicted in Fig. 4, the diaphyseal intramedullary guiding rod would offset the cannulated reamer at the metaphyseal level, due to the anterolateral eccentric position of the diaphyseal center with reference to the metaphyseal center, thereby predisposing bone to cortical abutment or fracture on reaming. It should be noted that the designated cannulated reaming preparation was utilized in virtually all the reported Caucasian series. Our study was the first to report the free-hand burring technique in preparing for the second-generation cone, with promising mid-term outcomes commensurate with the reamer-prepared cone results in Caucasians. Remarkably, there was no aseptic loosening in our series, with a 100% cone revision-free survivorship. Our findings are valuable and clinically-pertinent, especially for Asian patients given their different osteometry.
Further studies incorporating computed tomography are needed to delineate the exact anatomical differences between Asian and Caucasian knees and to elucidate the local applicability of existing cannulated reaming preparation. This will also shed light on modifications in implants to accommodate Asian osteometry. From the authors’ perspective, it will have impactful potential to expand the applicability of future-generation cones to suit different osteometry and ethnicity, hence translating to improved outcomes.
Our study had the following limitations. First, it was a single-surgeon series which might limit the generalizability of the surgical techniques and results. Second, the anatomical constraints were assessed intraoperatively based on the surgeons’ experience. Ideally, CT-based studies would be valuable in delineating the osteometry, hence dictating which bone preparation technique was of choice. Third, the outcome measurements were on short-term basis only. Longer-term follow-ups are necessary to conclude on the longevity of cone implantation using our surgical techniques.
Conclusions
Second-generation titanium metaphyseal cone implanted with free-hand burring bone preparation yielded promising mid-term clinical and radiological results in our locality. Our study highlights the anatomical constraints in Asian knees which could potentially limit the applicability of cannulated reaming designated for second-generation cone. Caution should be exercised in preparing bone for cone implantation in Asian patients given their relatively small and bowed bone and meta-diaphyseal center mismatch.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- KSS:
-
Knee Society Knee Scores
- TKA:
-
Total Knee Arthroplasty
- AORI:
-
Anderson Orthopaedic Research Institute
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5.
Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–75.
Morgan-Jones R, Oussedik SI, Graichen H, Haddad FS. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015;97-B(2):147-9.
Faizan A, Bhowmik-Stoker M, Alipit V, Kirk AE, Krebs VE, Harwin SF, Meneghini RM. Development and verification of novel porous titanium metaphyseal cones for revision total knee arthroplasty. J Arthroplasty. 2017;32(6):1946–53.
Patel NK, Kim EG, Chughtai M, Khlopas A, Elmallah RD, Harwin SF, Delanois RE, Mont MA. Highly porous metaphyseal cones in revision total knee arthroplasty: a case series. J Knee Surg. 2016;29(8):614–20.
Denehy KM, Abhari S, Krebs VE, Higuera-Rueda CA, Samuel LT, Sultan AA, Mont MA, Malkani AL. Metaphyseal fixation using highly porous cones in revision total knee arthroplasty: minimum two year follow up study. J Arthroplasty. 2019;34(10):2439–43.
Tetreault MW, Perry KI, Pagnano MW, Hanssen AD, Abdel MP. Excellent two-year survivorship of 3D-printed metaphyseal cones in revision total knee arthroplasty. Bone Joint J. 2020;102-B(6_Supple_A):107-115.
Remily EA, Dávila Castrodad IM, Mohamed NS, Wilkie WA, Kelemen MN, Delanois RE. Short-term outcomes of 3D-printed titanium metaphyseal cones in revision total knee arthroplasty. Orthopedics. 2021;44(1):43–7.
Chalmers BP, Malfer CM, Mayman DJ, Westrich GH, Sculco PK, Bostrom MP, Jerabek SA. Early survivorship of newly designed highly porous metaphyseal tibial cones in revision total knee arthroplasty. Arthroplast Today. 2021;23(8):5–10.
Monárrez R, Bains SS, Chen Z, Sax OC, Salib CG, Mont MA, Delanois RE. Two-year survivorship and outcomes of a three-dimensional printed metaphyseal cone in the setting of revision total knee arthroplasty. J Knee Surg. 2022;35(14):1540–3.
Patel AR, Barlow B, Ranawat AS. Stem length in revision total knee arthroplasty. Curr Rev Musculoskelet Med. 2015;8(4):407–12.
Hilgen V, Citak M, Vettorazzi E, Haasper C, Day K, Amling M, Gehrke T, Gebauer M. 10-year results following impaction bone grafting of major bone defects in 29 rotational and hinged knee revision arthroplasties: a follow-up of a previous report. Acta Orthop. 2013;84(4):387–91.
Chalmers BP, Desy NM, Pagnano MW, Trousdale RT, Taunton MJ. Survivorship of metaphyseal sleeves in revision total knee arthroplasty. J Arthroplasty. 2017;32(5):1565–70.
Watters TS, Martin JR, Levy DL, Yang CC, Kim RH, Dennis DA. Porous-coated metaphyseal sleeves for severe femoral and tibial bone loss in revision TKA. J Arthroplasty. 2017;32(11):3468–73.
Lachiewicz PF, Watters TS. Porous metal metaphyseal cones for severe bone loss: when only metal will do. Bone Joint J. 2014;96-B(11 Supple A):118-21.
Divano S, Cavagnaro L, Zanirato A, Basso M, Felli L, Formica M. Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg. 2018;138(6):851–63.
Kim HJ, Lee OS, Lee SH, Lee YS. Comparative analysis between cone and sleeve in managing severe bone defect during revision total knee arthroplasty: a systematic review and meta-analysis. J Knee Surg. 2018;31(7):677–85.
Zanirato A, Formica M, Cavagnaro L, Divano S, Burastero G, Felli L. Metaphyseal cones and sleeves in revision total knee arthroplasty: Two sides of the same coin? Complications, clinical and radiological results-a systematic review of the literature. Musculoskelet Surg. 2020;104(1):25–35.
Roach RP, Clair AJ, Behery OA, Thakkar SC, Iorio R, Deshmukh AJ. Aseptic loosening of porous metaphyseal sleeves and tantalum cones in revision total knee arthroplasty: a systematic review. J Knee Surg. 2021;34(10):1033–41.
De Martino I, De Santis V, Sculco PK, D’Apolito R, Assini JB, Gasparini G. Tantalum Cones provide durable mid-term fixation in revision TKA. Clin Orthop Relat Res. 2015;473(10):3176–82.
Kamath AF, Lewallen DG, Hanssen AD. Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty: a five to nine-year follow-up. J Bone Joint Surg Am. 2015;97(3):216–23.
Wang C, Pfitzner T, von Roth P, Mayr HO, Sostheim M, Hube R. Fixation of stem in revision of total knee arthroplasty: cemented versus cementless-a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3200–11.
Tang WM, Chiu KY, Kwan MF, Ng TP, Yau WP. Sagittal bowing of the distal femur in Chinese patients who require total knee arthroplasty. J Orthop Res. 2005;23(1):41–5.
Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong). 2007;15(1):32–6.
Tang Q, Zhou Y, Yang D, Xu H, Liu Q. The offset of the tibial shaft from the tibial plateau in Chinese people. J Bone Joint Surg Am. 2010;92(10):1981–7.
Acknowledgements
Publication was made possible in part by support from the HKU Libraries Open Access Author Fund sponsored by the HKU Libraries.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
P.K.C. was the chief surgeon involved in all the reported cases and the corresponding author who supervised the manuscript writing. T.K.C.L. was the major contributor in writing the manuscript. Other authors contributed to the collection and analysis of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster, with the reference number UW 20-253. Informed consents were obtained from all the patients upon recruitment.
Consent for publication
Not applicable.
Competing interests
Kwong Yuen Chiu is a member of the Editorial Board of Arthroplasty and other authors declare that they have no competing interests. All authors were not involved in the journal’s review or decisions related to this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leung, T.K.C., Chan, P.K., Fu, H. et al. Promising short-term outcomes of free-hand burring technique to implant second-generation metaphyseal cone in Asian knees – a case series. Arthroplasty 6, 35 (2024). https://doi.org/10.1186/s42836-024-00254-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42836-024-00254-2