Abstract
Objective
To evaluate the effect of medial posterior tibial slope (PTS) on mid-term postoperative range of motion (ROM) and functional improvement of the knee after medial unicompartmental knee arthroplasty (UKA).
Methods
Medical records of 113 patients who had undergone 124 medial UKAs between April 2009 through April 2014 were reviewed retrospectively. The mean follow-up lasted 7.6 years (range, 6.2–11.2 years). Collected were demographic data, including gender, age, height, weight of the patients. Anteroposterior (AP) and lateral knee radiographs of the operated knees were available in all patients. The knee function was evaluated during office follow-up or hospital stay. Meanwhile, postoperative PTS, ROM, maximal knee flexion and Hospital for Special Surgery (HSS) knee score (pre−/postoperative) of the operated side were measured and assessed. According to the size of the PTS, patients were divided into 3 groups: group 1 (<4°), group 2 (4° ~ 7°) and group 3 (>7°). The association between PTS and the knee function was investigated.
Results
In our cohort, the average PTS was 2.7° ± 0.6° in group 1, 5.6° ± 0.9° in group 2 and 8.7° ± 1.2° in group 3. Pairwise comparisons showed significant differences among them (p < 0.01). The average maximal flexion range of postoperative knees in each group was 112.4° ± 5.6°, 116.4° ± 7.2°, and 117.5° ± 6.1°, respectively, with significant difference found between group 1 and group 2 (p < 0.05), and between group 1 and group 3 (p < 0.05). However, the gender, age, and body mass index (BMI) did not differ between three groups and there was no significant difference between groups in terms of pre−/postoperative HSS scores or postoperative knee ROM.
Conclusion
A mid-term follow-up showed that an appropriate PTS (4° ~ 7°) can help improve the postoperative flexion of knee. On the other hand, too small a PTS could lead to limited postoperative knee flexion. Therefore, the PTS less than 4° should be avoided during medial UKA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
UKA has been increasingly used in clinical practice over the last decade [1]. For the treatment of end-stage medial compartment disease of the knee, it has the advantage of minimal invasiveness, less bleeding, less soft tissue injury, fast recovery and bone-stock conservation [2, 3]. It has become a popular alternative to total knee arthroplasty (TKA), with great patient satisfaction and favorable functional outcomes, especially in younger patients [4]. In recent years, medical centers that performed a large number of UKAs reported that the 10-year prosthesis survival rate after UKA stood somewhere between 94% and 98% [5,6,7], which is close or even equal to the post-TKA rate. Despite the success, complications in UKA were reported, and complications, such as prosthesis loosening and lining wear, which are associated with mal-alignment after UKA, accounted for over 50% of the reasons for UKA revision [8].
It is more technically demanding to align and seat UKA prostheses appropriately given small operation space associated with minimally invasive procedures. Although Berger et al. [5] followed up 62 patients and found a 92% postoperative satisfaction, postoperative radiographic examination still revealed progressive loss of joint space. The statistics of the Australian Orthopaedic Association National Joint Replacement Registry [9] showed that the cumulative percentage of 5-years UKA revision was as high as 15%. The revision of UKA is associated with multiple factors, including prosthesis design, surgeon experience, patient selection, polyethylene quality, and intraoperative alignment and fixation [10,11,12,13]. Among them, the accurate positioning of the implant is a critical factor for implant longevity. A broad range of up to 20° for the PTS has been recommended by many researchers and manufacturers [14], and the PTS may directly affect implant stability, postoperative joint mobility, and the wear rate of the prosthesis. Takayama et al. [15] showed that, compared with knee flexion, an increased PTS led to a tight component gap at knee extension. Therefore, they suggested that when tibial sagittal osteotomy is performed, anatomical PTS should be individualized. However, no unified standard is available for the optimal PTS, as the role of PTS is not fully understood and remains controversial.
In this study, we retrospectively investigated the effect of PTS on the knee function in the medium term after medial UKA, with an attempt to find a surgical strategy for the tibial plateau osteotomy in the medial UKA.
Materials and methods
Patients
We retrospectively analyzed the records of 113 patients with medial unicompartmental knee osteoarthritis who had undergone medial UKA between April 2009 and April 2014. There were 38 males (involving 43 knees) and 75 females (involving 81 knees), with an average age of 68.3 years (range, 48 to 86 years). Mean postoperative follow-up lasted 7.6 years (range, 6.2–11.2 years). The inclusion criteria [16] for this case series study included: (1) patients who were definitely diagnosed with medial unicompartmental knee osteoarthritis, (2) preoperative ROM > 90°, (3) joint flexion contracture < 15° and (4) varus deformity < 15°. The exclusion criterion was the past history of having undergone knee surgeries. The anteromedial osteoarthritis of knee with normally functional anterior cruciate ligament is considered to be best indicated for UKA [6]. It is worth noting that patellofemoral joint osteoarthritis was not a contraindication for UKA in this study [17]. Careful and reasonable patient selection was the key to the efficacy of the surgery.
Follow-up
The patients were followed up for HHS scores, and AP and lateral radiographic results (DICOM format) of the knee. In the physical examination, we employed a protractor to measure ROM and maximal flexion range of the knees (Fig. 1).
Surgical technique
All surgical procedures were performed by a senior surgeon (HC) using the same prosthetic implant (Bioment, Oxford III, USA) by using the same minimally invasive procedure, including the tibial plateau osteotomy. Following the operation manual of Biomet Oxford phase III, the prosthesis was aimed for a 7° of PTS.
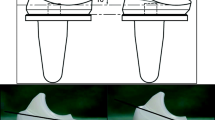
Radiological analysis
Postoperative lateral radiographs of the knee were obtained in DICOM format, and the PTS was measured by using the UniSight software and the measuring tool that goes with the package. The long axis of the proximal tibia, which was most commonly used in clinical practice and is believed to be the normal anatomical axis of the tibia [18], was taken as the reference axis. PTS was defined by the angle between the line perpendicular to the reference axis and the line parallel to the prosthesis platform (Fig. 2). Radiological parameters were independently measured by two authors (CZJ and CKZ) and checked by a senior doctor (HC) to ensure that PTS error was less than 1°. In terms of the angle of PTS measured, patients were divided into 3 groups: a <4° group (group 1), a 4° ~ 7° group (group 2), a >7° group (group 3).
The measurement method on standardized knee radiographs in the lateral view. TPAA, the tibial proximal anatomical axis. Tibial posterior slope (PTS) was defined by the angle between the posterior inclination line of the medial tibial plateau and a line perpendicular to the TPAA, which is defined by α-angle
Statistical analysis
All statistical analyses were conducted by using SPSS version 19.0. Categorical variables were compared by using the Chi-square test. Continuous variables were presented as mean ± standard deviation (SD) and the ANOVA was applied to analyze statistical differences of the related data. The t-test and Student-Newman-Keuls test were used to evaluate the significance of differences between independent samples. p values in this study were two-sided and considered statistically significant when they were less than 0.05.
Results
Of 124 knees included in the study, 19 knees (15.3%) were in group 1, 45 knees (36.3%) in group 2, and 60 knees (48.4%) in group 3. The average PTS of all knees was 6.6° ± 2.4°, ranging from 1.7° to 13°, with P75-P25 = 8.4°-5.0° (Fig. 3). And there were not significant differences among the three groups in gender, age, and BMI (Table 1).
In our cohort, apart from aforementioned patients, 6 patients died and lost to follow-up, and 15 lost contact. No known complications of the UKA took place at the time of death in these patients. During the follow-up period, the insert replacement was performed on one patient due to the impingement of residuary cement and 4 patients received revision surgery with TKA. Of these patients, the PTS was 3.4°, 9.9°, 8.8°, 12.9° and 3.9°, respectively (Table 3). The remaining patients received no subsequent surgery or were not re-admitted due to UKA.
The postoperative HHS scores averaged 91.7 at the last follow-up, being virtually 40 higher than preoperative HSS scores, indicating that the clinical effect was excellent. Furthermore, the average PTS was 2.7° ± 0.6° in group 1, 5.6° ± 0.9° in group 2 and 8.7° ± 1.2° in group 3, respectively. Correspondingly, preoperative HSS score in each group was 48.79 ± 6.02, 52.40 ± 6.77, and 50.93 ± 7.02, respectively. And postoperative HSS score was 92.68 ± 3.23, 91.87 ± 4.15, and 91.67 ± 5.54 in groups 1, 2 3, respectively. Significant improvement was achieved after UKA (p < 0.01). However, there were no significant differences among the three groups in pre- and postoperative HSS scores. Similarly, as shown in Table 2, there was no significant difference in the ROM of both pre- and postoperative knee joints among the three groups (all p > 0.05). We are led to draw the conclusion that the PTS exerts little effect on the postoperative functional recovery after the medial UKA within a certain range.
Our main finding was that the value of postoperative maximal knee flexion was significantly lower in group 1 than in group 2 and group 3 (p = 0.013). It was 116.44° ± 7.20° in group 2 and 117.50° ± 6.14° in group 3 respectively, whereas it was 112.37° ± 5.62° in group 1, with the difference in flexion being almost 5° (Fig. 4). This finding indicated that the PTS has an impact on the maximal knee flexion after medial UKA. In performing tibial sagittal osteotomy during a medial UKA, too small a PTS slope (< 4°) may impair postoperative knee flexion.
Discussion
Multiple studies examined the impact of PTS on the knee joint from different perspectives. Kang et al. [19] explored biomechanical effects of PTS on UKA using finite element analysis, and found that the PTS influenced the contact stress on the polyethylene insert and articular cartilage after UKA. Hashemi et al. [20] used MRI to assess PTS and Nunley et al. [21] employed CT scans to evaluate the PTS in patients who are indicated for UKA. Of note, both of them noted a significant difference between the medial and lateral compartments in tibial slopes. Medial compartment diseases tend to be associated with increased anterior wear and a decreased PTS slope, while lateral compartment diseases commonly bear connection with posterior wear and an increased PTS. Although the role of the PTS has been discussed in the current literature on UKA, its role and recommended angle remain elusive [15].
Excellent lower limb alignment and precise implant positioning are essential to the attainment of favorable results of UKA. Therefore, researchers have tried different measuring methods to find the optimal PTS. For example, Hashemi et al. [20] used the long axis of the proximal tibia as the reference axis to blindly measure the PTS of 20 cases. The PTS of male adults was − 3° ~ 10°, while the PTS of female adults was 0 ° ~ 10 °. They found a larger PTS in females (5.9 °) than in males (3.7 °). On the other hand, Zhang et al. [22] applied different reference axes to evaluate the PTS of 80 healthy adults in southern China on three-dimensional reconstruction of CT. The medial tibial posterior slope was 11.5° with the proximal tibia long axis, 8.4° with the anterior tibial cortical axis and 6.3° with the posterior tibial cortical axis. The results of the three axes varied but were correlated with each other significantly. In this study, according to the original design objective and the operation manual, the prosthesis (Oxford phase III, Biomet) was aimed for a 7° of PTS, a radiological standard. Although the surgeon strictly followed the steps as instructed, the PTS measured after medial UKA was 6.6° ± 2.4°, not a constant angle of 7° (Fig. 2). Various factors can impact on PTS measurements. First and foremost, when an extracorporeal tibial medullary locator is used, anatomical variations may lead to disparate positioning, which can eventually cause discrepancy in tibial plateau osteotomy. Secondly, patients with medial compartment osteoarthritis may well have subchondral osteosclerosis of the tibial plateau, which can result in swing saw blade deviating upward and a smaller PTS in osteotomy. Or, in order to avoid deviation, the surgeon may slightly press the swing saw downwards, which leads to excessive osteotomy of the tibial plateau. Last but not least, due to the use of minimally invasive incision in UKA, poor vision in the posterior part of the knee joint may cause excessive bone cement to remain, which elevates the posterior part of the tibial prosthesis and leads to a smaller PTS. What is more, factors such as varus deformity, valgus deformity and flexion contracture, need to be considered during the operation to avoid excessive correction of the lower limb alignment and excessive stress in the contralateral compartment.
There is currently no unified standard for tibial plateau osteotomy of the UKA, and the optimal PTS should help surgeons perform the proximal tibia osteotomy properly on the sagittal plane, to optimize limb alignment and implant positioning. Many researchers tried different posterior slopes for the tibial plateau osteotomy. Nunley et al. [21] evaluated CT imaging parameters of 2395 patients who had undergone UKA and suggested that to obtain a better knee motor function, the PTS should be within 5° ~ 7°. The degree of PTS greatly influences the kinematics of the knee and plays an important role in sagittal plane stability and tibial translation with weight bearing [23,24,25]. Weber et al. [8] positioned prostheses under four different tibial slopes (− 4°, 0°, 4°, 8°) to perform a kinematic analysis and found that increasing the tibial slope led to a reduced backside wear. They recommended a tibial slope between 4° and 8° in UKA to reduce wear. Campbell et al. [26] used computer-assisted tomography to perform UKA on 60 patients, whose tibial slopes were at about 7°, and accomplished good postoperative function. Hernigou et al. [27], on the basis of a follow-up of sixteen years (mean time), suggested that the posterior slope of the tibial implant > 7° should be avoided, particularly if the anterior cruciate ligament is absent at the time of implantation. Most importantly, it is generally believed that the anteversion of tibial plateau or a 0° of PTS is undesirable [28, 29], which will not only limit flexion of the knee, but also lead to excessive stress on the tibial prosthesis. It can accelerate the wear of the polyethylene insert and the loosening of the prosthesis. With regard to the re-operation after UKA in our cohort (Table 3), our evidence did not suffice to support a conclusion that PTS is correlated with such failures, and further studies are warranted. However, in this study, we divided the PTS into three groups (< 4°, 4° ~ 7°, and > 7°) and found that too small a PTS (< 4°) led to limited postoperative knee flexion.
This study has several limitations. First, although studies regarding PTS in UKA are scanty, the retrospective study design is still of limited value. This specific field should be prospectively studied. Second, we did not compare the effects of preoperative and postoperative PTS changes on postoperative knee function, because we believed that the measurement of PTS in the cases of medial compartment knee osteoarthritis was not accurate. Third, the power of this study, like all other radiographic studies of TKA, might be impaired by inter- and intra-observer variability of radiographic measurements. Finally, the size of patients was limited due to the retrospective nature of the study, further larger-sized studies are needed.
In conclusion, although the medial UKA has been successful in patients with medial compartment knee osteoarthritis, the PTS-related knee flexion limitation should not be neglected. It remains a pivotal part of joint replacement surgeries to properly deal with the PTS, since PTS plays a significant role in the maintenance of the tension of cruciate ligaments of the knee joint, the normal sliding and rolling of the femoral condyle, and the stability of the prosthesis. In the tibial plateau osteotomy and fixation of the tibial prosthesis, a too small PTS should be avoided. PTS within an appropriate range (4°∼7°) can help achieve the maximal knee flexion after medial UKA.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PTS:
-
posterior tibial slope
- ROM:
-
range of motion
- UKA:
-
medial unicompartmental knee arthroplasty
- HSS:
-
Hospital for Special Surgery
- AP:
-
anteroposterior
- BMI:
-
body mass index
- TKA:
-
total knee arthroplasty
References
Johal S, Nakano N, Baxter M, Hujazi I, Pandit H, Khanduja V. Unicompartmental knee Arthroplasty: the past, current controversies, and future perspectives. J Knee Surg. 2018;31:992–8.
Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91:52–7.
Griffin T, Rowden N, Morgan D, Atkinson R, Woodruff P, Maddern G. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg. 2007;77:214–21.
Kang KT, Park JH, Koh YG, Shin J, Park KK. Biomechanical effects of posterior tibial slope on unicompartmental knee arthroplasty using finite element analysis. Biomed Mater Eng. 2019;30:133–44.
Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006.
Argenson JN, Blanc G, Aubaniac JM, Parratte S. Modern unicompartmental knee arthroplasty with cement: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg Am. 2013;95:905–9.
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee. 2014:S26–32.
Weber P, Schröder C, Schmidutz F, Kraxenberger M, Utzschneider S, Jansson V, Müller PE. Increase of tibial slope reduces backside wear in medial mobile bearing unicompartmental knee arthroplasty. Clin Biomech (Bristol, Avon). 2013;28:904–909.
Hang JR, Stanford TE, Graves SE, Davidson DC, de Steiger RN, Miller LN. Outcome of revision of unicompartmental knee replacement. Acta Orthop. 2010;81:95–8.
Stern SH, Becker MW, Insall JN. Unicondylar knee arthroplasty. An evaluation of selection criteria. Clin Orthop Relat Res. 1993:143–8.
Robertsson O, Knutson K, Lewold S, Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001;83:45–9.
Ackroyd CE, Whitehouse SL, Newman JH, Joslin CC. A comparative study of the medial St Georg sled and kinematic total knee arthroplasties. Ten-year survivorship. J Bone Joint Surg Br. 2002;84:667–72.
Aldinger PR, Clarius M, Murray DW, Goodfellow JW, Breusch SJ. Medial unicompartmental knee replacement using the "Oxford Uni" meniscal bearing knee. Orthopade. 2004;33:1277–83.
Weber P, Crispin A, Schmidutz F, Utzschneider S, Pietschmann MF, Jansson V, Müller PE. Improved accuracy in computer-assisted unicondylar knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:2453–61.
Takayama K, Matsumoto T, Muratsu H, Ishida K, Araki D, Matsushita T, Kuroda R, Kurosaka M. The influence of posterior tibial slope changes on joint gap and range of motion in unicompartmental knee arthroplasty. Knee. 2016;23:517–22.
Deschamps G, Chol C. Fixed-bearing unicompartmental knee arthroplasty. Patients' selection and operative technique. Orthop Traumatol Surg Res. 2011;97:648–61.
Song EK, Park JK, Park CH, Kim MC, Agrawal PR, Seon JK. No difference in anterior knee pain after medial unicompartmental knee arthroplasty in patients with or without patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24:208–13.
Genin P, Weill G, Julliard R. The tibial slope. Proposal for a measurement method. J Radiol. 1993;74:27–33.
Kang KT, Park JH, Koh YG, Shin J, Park KK. Biomechanical effects of posterior tibial slope on unicompartmental knee arthroplasty using finite element analysis. Biomed Mater Eng. 2019;30:133–44.
Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Mansouri H, Dabezies E. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90:2724–34.
Nunley RM, Nam D, Johnson SR, Barnes CL. Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplast. 2014;29:1677–80.
Zhang Y, Wang J, Xiao J, Zhao L, Li ZH, Yan G, Shi ZJ. Measurement and comparison of tibial posterior slope angle in different methods based on three-dimensional reconstruction. Knee. 2014;21:694–8.
Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86:506–11.
Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, Müller PE. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19:1643–8.
Haddad B, Konan S, Mannan K, Scott G. Evaluation of the posterior tibial slope on MR images in different population groups using the tibial proximal anatomical axis. Acta Orthop Belg. 2012;78:757–63.
Campbell DG, Johnson LJ, West SC. Multiparameter quantitative computer-assisted tomography assessment of unicompartmental knee arthroplasties. ANZ J Surg. 2006;76:782–7.
Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86:506–11.
Mariani EM, Bourne MH, Jackson RT, Jackson ST, Jones P. Early failure of unicompartmental knee arthroplasty. J Arthroplast. 2007;22:81–4.
Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J. Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res. 2013;99:S219–25.
Acknowledgements
Not applicable.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (No. 81071473).
Author information
Authors and Affiliations
Contributions
Conception and design: Chuan He. Collection and pooling of data: Zhijie Chen, Kaizhe Chen, Yufei Yan. Data analysis and interpretation: Jianmin Feng, Yi Wang, Zhihong Liu and Qingming Yang. Manuscript preparation: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study (reference number: 2020–170) was approved by the Ethics Committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai City, China.
Consent for publication
Not applicable.
Competing interests
Chuan He is a member of the Editorial Board of Arthroplasty. Other authors declare that they have no competing interests in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Z., Chen, K., Yan, Y. et al. Effects of posterior tibial slope on the mid-term results of medial unicompartmental knee arthroplasty. Arthroplasty 3, 11 (2021). https://doi.org/10.1186/s42836-021-00070-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42836-021-00070-y