Abstract
Background
RHOBTB2 gene is associated with developmental and epileptic encephalopathy-64(DEE-64), which is characterized by epilepsy, developmental delay, microcephaly, unspecific facial dysmorphism, and paroxysmal movement disorders. Most previous studies showed that the phenotypes of RHOBTB2 gene include developmental and epileptic encephalopathy(DEE) and DEE with paroxysmal movement disorders. Only one study showed that patient with RHOBTB2 variant had paroxysmal movement disorders with no epilepsy.
Case presentations
Two cases with RHOBTB2 variants are presented here: Case one was diagnosed as DEE, he had recurrent afebrile focal status epilepticus and paroxysmal extrapyramidal symptoms in infancy. Interictal electroencephalogram (EEG) showed focal discharges. Brain magnetic resonance imaging (MRI) showed cortical dysplasia. Epilepsy of case one was refractory. Nevertheless, case two only showed paroxysmal movement disorders alone in adolescence. Video EEG showed focal discharges during an interictal dystonic episode and he brain MRI was normal.
Conclusion
The phenotypes of RHOBTB2 gene include DEE, paroxysmal movement disorders, and DEE with paroxysmal movement disorders. RHOBTB2 can be one of the pathogenic genes of paroxysmal movement disorders.
Similar content being viewed by others
Background
Rho-related BTB domain-containing protein 2(RHOBTB2; MIM: 607,352) is an atypical Rho GTPase, which is mapped to chromosome 8p21.2 and contains 9 exons. RHOBTB2 is composed of a GTPase domain, a proline-rich region, a tandem of two BTB domains, and a conserved C-terminal region, and it is highly expressed in neuronal tissues [1]. Wilkins et al. [2] found that RHOBTB2 is bound to the ubiquitin ligase scaffold protein CUL3, recruits target proteins for degradation and mediates auto-ubiquitination. Straub et al. [3] identified 5 RHOBTB2 variants in 10 patients with developmental and epileptic encephalopathy-64 (DEE64; MIM: 618,004), all of the variants affected BTB domains. They showed varied clinical manifestations, including epilepsy, developmental delay, hemiparesis, paroxysmal movement disorders and microcephaly.
To date, most studies showed that patients with RHOBTB2 variants had DEE and some of them had paroxysmal movement disorders. Only one patient with RHOBTB2 variants had paroxysmal movement disorders with no epilepsy in the literature [4]. Here, we described two cases with novel RHOBTB2 variants in detail and summarized other reported cases to further explore the RHOBTB2 gene-associated phenotypic spectrum.
Case presentation
Case one
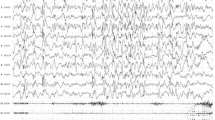
A one-year-old boy with a negative family history of neurological disorders was born at 38 weeks of gestational age by successful virginal delivery. He had delayed developmental milestones with head control at 11 months and limited interaction. He could not sit alone at the age of 1 year and 2 months. His seizure onset age was 55 days after birth, he experienced recurrent afebrile focal status epilepticus (SE), manifested insistent strabismus, unilateral limb twitching with impaired consciousness, and the focal SE lasted from 30 min to 2 h. Paroxysmal extrapyramidal symptoms were observed recurrently, including gaze upward, nystagmus, and dystonic posturing in one arm lasting a few minutes to 30 min with a frequency of 3 to 5 times per day. Video electroencephalogram (EEG) showed normal background. Interictal EEG showed central and parietal slow and sharp waves, and ictal EEG monitored focal SE originating from the right hemisphere. Brain magnetic resonance imaging (MRI) was taken at the age of 10 months, and it showed a widening of frontotemporal subarachnoid space and cortical dysplasia (Fig. 1). The hereditary metabolic screening was normal. A heterozygous de novo missense RHOBTB2 variant (NM_001160036.1, c.103G > A, p. Glu35Lys) was identified using trio-based whole-exome sequencing (WES) (Fig. 2a-c). This novel variant was absent from the control population in the Genome Aggregation Database (gnomAD) and was classified as likely pathogenic according to the American College of Medical Genetics and Genomics (ACMG) guidelines. He was diagnosed as DEE with paroxysmal movement disorder. He was treated with multiple antiepileptic drugs, including valproic acid, topiramate, oxcarbazepine, levetiracetam, clonazepam and lacosamide. At the last follow-up, he still had focal SE and extrapyramidal symptoms at 1 year 2 months.
Case two
The boy was born at 38 weeks with a good start at birth from non-consanguineous parents. He grew normally and performed well at school before he developed paroxysmal movement disorders at the age of 13 years. At the age of 1 year 5 months, an episode of febrile seizure was noted for one time, when he developed fever up to 101.3°F, he performed gaze upward and limb tremor with impaired consciousness for more than ten seconds. Since then, there were no epileptic seizures. From the age of 13 years 6 months, episodes of paroxysmal movement disorders began to occur. Unilateral limb dyskinesia manifested with left limb dystonic posturing and left feet internal rotation. He could walk with an abnormal gait and had a clear consciousness. The episodes usually lasted from half-hour to several hours and recurred several times per day. His language expression was unclear for a few hours after paroxysmal dystonia. Video EEG showed right frontal spike-slow waves and poly-spike slow waves during an interictal dystonic episode. The brain MRI and metabolic screening were normal. Trio-WES was taken at the age of 13 years 9 months and showed a de novo RHOBTB2 variant (NM_001160036.1, c.346C > T, p. Arg94Cys) (Fig. 2d-f). This novel variation was classified as likely pathogenic according to ACMG. At first, he was treated with oxcarbazepine, but there was no effect. Then the drug was replaced by levodopa and benserazide hydrochloride, however, the patient did not respond to the treatment either.
Review of patients with RHOBTB2 variants
We searched in Pubmed with "RHOBTB2" as the keyword. The genotype and phenotype of 19 patients reported in the literature with RHOBTB2 variants were summarized in Table 1. The phenotypes of RHOBTB2 variants of 21 patients in previous literature and this study were showed in Fig. 3.
There were seven de novo missense RHOBTB2 variants identified in 19 patients, among whom eight patients shared the same variant p. Arg483His, five patients shared the same variant p. Arg511Gln and two patients shared the same variant p. Arg511Trp. Of the 19 patients, 13 patients were female and 6 patients were male. Eighteen patients were diagnosed with DEE, the median age of seizure onset was 3.5 months. Various seizure types were observed in 18 patients, including focal seizure in 7 patients, tonic seizure in 3 patients, generalized tonic–clonic seizure (GTCS) in 2 patients, myoclonic seizure in 1 patient and epileptic spasms in 1 patient. There were a total of 12 patients who experienced SE, three of them experienced febrile SE and two of them had the characteristics of focal seizures. All 18 patients had developmental delay. Meanwhile, other clinical manifestations had been observed in some patients. Thirteen of 18 patients had paroxysmal movement disorders, including dystonia, athetoid movement, dyskinesia and choreatic movement. Fourteen of 18 patients had microcephaly. Nine patients had hypotonia. Four patients had hemiplegia. Atypical facial dysmorphism was described in 9 patients, including low nasal bridge, epicanthal folds, micrognathia, deep-set eyes and long philtrum. Six patients had EEG details, five patients showed interictal focal epileptic discharges and one patient showed normal EEG. Among all patients who underwent brain MRI examination, 7 patients showed cortical atrophy, 3 patients had thin corpus callosum, 1 patient had corpus callosum hypoplasia, and 1 patient showed delayed myelination. All 7 patients with brain atrophy had a history of SE.
One patient reported previously had paroxysmal movement disorders without a typical epileptic seizure. This patient had complex hyperkinetic movements at 6 months of age, followed by generalized choreodystonia and dystonia at 3 years old. She had developmental milestones delay, microcephaly and facial dysmorphism. Her video EEG and brain MRI were both normal.
Patients with RHOBTB2 variants who had epilepsy were treated with multiple antiepileptic drugs. Two patients had responded to levetiracetam and one patient to phenobarbital. Seizures of one patient were controlled by carbamazepine after 4 years old. Other epilepsy patients showed drug refractory. Meanwhile, one patient with paroxysmal movement disorders had responded to carbamazepine.
Discussion
In 2018, Straub et al. [3] first reported that heterozygous variants in RHOBTB2 are associated with DEE-64. Since then, there were total 19 cases reported associated with RHOBTB2 and additional clinical details are shown in Table 1 [3,4,5,6,7,8]. Eighteen patients with RHOBTB2 variants had characterized of DEE, among them, 13 patients showed paroxysmal movement disorders, including dystonia, dyskinesia, athetosis and choreatic features. Only one patient with RHOBTB2 variant reported previously had paroxysmal movement disorders without epilepsy [4]. Previous studies showed that patients with RHOBTB2 variants could manifested microcephaly, stereotyped movement, and unspecific facial dysmorphism including low nasal bridge, epicanthal folds, micrognathia, deep-set eyes, and long philtrum. In this study, we reported two patients with novel RHOBTB2 variants. One patient showed epilepsy in early infancy, he had developmental milestones delay, microcephaly and paroxysmal extrapyramidal symptoms, while the other patient only showed paroxysmal movement disorders in adolescence.
Seizure onset of patients with RHOBTB2 variants usually occurred during the infantile period. Multiple seizure types were observed, including focal seizure, GTCS, myoclonic seizure, tonic seizure, and epileptic spasms. SE was common in most patients. 65% (13/20) of epilepsy patients with RHOBTB2 variants reported in the literature and in this study experienced SE. Among the 13 patients, three of them were characterized by febrile SE, two of them experienced focal SE, as one patient in our study. All epilepsy patients with RHOBTB2 variants had developmental delays. EEG usually showed interictal focal epileptic discharges. The abnormalities of brain MRI including cortical atrophy, corpus callosum dysplasia, delayed myelination, and hippocampal atrophy were observed. All patients with brain atrophy experienced SE. Four patients with hemiplegia had a history of SE and one of them showed focal SE, indicated that SE can lead to hemiplegia. Brain MRI of some cases showed swollen or reduced focal diffusion in acute encephalopathy and subsequent focal atrophy. A previous study found that edema in acute encephalopathy could lead to different degrees of cerebral cortex atrophy in convalescence, focal SE could lead to hemispheric cerebral lesions in patients with Dravet syndrome, whereas generalized tonic–clonic SE could cause bilateral cerebral lesions [9]. Therefore, brain atrophy in patients with RHOBTB2 variants may be correlated with SE.
In this study, one patient with RHOBTB2 variant only showed paroxysmal movement disorders without afebrile seizures in adolescence. He had normal psychomotor development before episodes of dystonia occurred. Necpál, Ján et al. [4] reported a girl with RHOBTB2 variant who had paroxysmal movement disorders without epilepsy at 3 years old. Her clinical features were characterized by delays in developmental milestones, paroxysmal choreodystonia, microcephaly, and facial dysmorphism including epicanthal folds, wide nasal bridge, and long flat philtrum. These cases suggest that RHOBTB2 variants can cause paroxysmal movement disorders alone.
There were totally seven de novo RHOBTB2 variants in 19 patients reported previously. Eight patients shared the same variant p. Arg483His and five patients shared the same variant p. Arg511Gln (Table 1). All of the variants were located in BTB domains. The BTB domains bind to GTPase domain and to the ubiquitin ligase scaffold CUL3, the interaction mediates auto-ubiquitination and related to proteasomal degradation. Overexpression of RhoBTB in Drosophila showed more severe neurological phenotypes than upon knockdown, which indicated that the neurological symptoms caused by the variant in the BTB domain of RHOBTB2 gene may be due to the decrease of proteasomal degradation, followed by overexpression of RhoBTB [3]. Among the eight patients with the same variant p. Arg483His, five patients had DEE accompanied with paroxysmal movement disorders, two cases had DEE and one patient had paroxysmal movement disorders alone, which indicated that recurrent RHOBTB2 variant can lead to phenotypic variability. Two novel variants of RHOBTB2 in this study were located in the GTPase domain, they were characterized by DEE with paroxysmal movement disorders or paroxysmal movement disorders alone. This study support that RHOBTB2 is one of the pathogenic gene of epilepsy and paroxysmal movement disorders.
In this study, case one with DEE was treated with multiple antiepileptic drugs and showed refractory. In a previous study, some patients with RHOBTB2 variants who had DEE responded to levetiracetam, phenobarbital, and carbamazepine [3]. Paroxysmal movement disorders are usually difficult to treat. Case two in our study was treated by levodopa and benserazide hydrochloride and and oxcarbazepine, but there was no effect. In previous studies, RHOBTB2-associated paroxysmal movement disorders were commonly treated with carbamazepine. Straub et al. [3] reported three patients with epilepsy and paroxysmal movement disorders were treated with carbamazepine, one of them had a partial response for movement disorders. Spagnoli et al. [8] reported that paroxysmal movement disorders in one patient with RHOBTB2 variant completely resolved by carbamazepine.
Genetic etiology of paroxysmal movement disorders has been unveiled readily with the advent of next-generation sequencing (NGS). Pathogenic variant of the PRRT2 gene was identified firstly to be the cause of paroxysmal movement disorders [10]. Further studies confirmed that the phenotypes of the PRRT2 gene include paroxysmal kinesigenic dyskinesia, benign sporadic and familial infantile epilepsy, and the overlapping disorder of paroxysmal kinesigenic dyskinesia with infantile epilepsy [11]. Subsequently, more pathogenic genes related to paroxysmal movement disorders were reported, including SCN8A, DEPDC5, KCNA1, KCNMA1, PNKD and SLC2A1 [12]. SCN8A, DEPDC5, KCNA1 KCNMA1 and SLC2A1 are also epilepsy-related genes as RHOBTB2 in this study, which indicates that paroxysmal movement disorders and epilepsy may have gene pleiotropy or share similar pathogenesis.
Conclusion
Here we reported two patients with novel RHOBTB2 variants who had infantile DEE with paroxysmal movement disorders and adolescent paroxysmal movement disorders only. DEE-associated RHOBTB2 variants are characterized by multiple seizure types, SE, developmental delay, and cortical atrophy. The phenotypes of RHOBTB2 gene include DEE, paroxysmal movement disorders, and the overlapping disorder of DEE with paroxysmal movement disorders. RHOBTB2 can be one of the pathogenic genes of paroxysmal movement disorders.
Availability of data and materials
Department of Pediatrics, Peking University First Hospital.
Abbreviations
- ACMG:
-
American College of Medical Genetics and Genomics
- DEE:
-
Developmental and epileptic encephalopathy
- SE:
-
Status epilepticus
- EEG:
-
Electroencephalogram
- MRI:
-
Magnetic resonance imaging
- ILAE:
-
International League Against Epilepsy
- GTCS:
-
Generalized tonic–clonic seizure
- NGS:
-
Next-generation sequencing
References
Ramos S, Khademi F, Somesh BP, Rivero F. Genomic organization and expression profile of the small GTPases of the RhoBTB family in human and mouse. Gene. 2002;298:147–57.
Wilkins A, Ping Q, Carpenter CL. RhoBTB2 is a substrate of the mammalian Cul3 ubiquitin ligase complex. Genes Dev. 2004;18:856–61.
Straub J, Konrad EDH, Grüner J, Toutain A, Bok LA, Bok MT, et al. Missense Variants in RHOBTB2 Cause a Developmental and Epileptic Encephalopathy in Humans, and Altered Levels Cause Neurological Defects in Drosophila. Am J Hum Genet. 2018;102(1):44–57.
Necpál J, Zech M, Valachová A, Sedláček Z, Bendová S, Hančárová M, et al. Severe paroxysmal dyskinesias without epilepsy in a RHOBTB2 mutation carrier. Parkinsonism Relat Disord. 2020;77:87–8.
Belal H, Nakashima M, Matsumoto H, Yokochi K, Taniguchi-Ikeda M, Aoto K, et al. De novo variants in RHOBTB2, an atypical Rho GTPase gene, cause epileptic encephalopathy. Hum Mutat. 2018;39(8):1070–5.
Knijnenburg ACS, Nicolai J, Bok LA, Bay A, Stegmann APA, Sinnema M, et al. Acute encephalopathy after head trauma in a patient with a RHOBTB2 mutation. Neurol Genet. 2020;6(3):e418.
Rochtus A, Olson HE, Smith L, Keith LG, Achkar CI, Taylor A, et al. Genetic diagnoses in epilepsy: The impact of dynamic exome analysis in a pediatric cohort. Epilepsia. 2020;61(2):249–58.
Spagnoli C, Soliani L, Caraffi SG, Baga M, Rizzi S, Salerno GG, et al. Paroxysmal movement disorder with response to carbamazepine in a patient with RHOBTB2 developmental and epileptic encephalopathy. Parkinsonism Relat Disord. 2020;76:54–5.
Tian X, Ye J, Zeng Q, Zhang J, Yang X, Liu A, et al. The clinical outcome and neuroimaging of acute encephalopathy after status epilepticus in Dravet syndrome. Dev Med Child Neurol. 2018;60(6):566–73.
Chen W-J, Lin Y, Xiong Z-Q, Wei W, Ni W, Tan G-H, et al. Exome sequencing identifies truncating mutations in PRRT2 that cause paroxysmal kinesigenic dyskinesia. Nat Genet. 2011;43(12):1252–5.
Döring JH, Saffari A, Bast T, Brockmann K, Ehrhardt L, Fazeli W, et al. The Phenotypic Spectrum of PRRT2-Associated Paroxysmal Neurologic Disorders in Childhood. Biomedicines. 2020;8(11):456.
Delorme C, Giron C, Bendetowicz D, Méneret A, Mariani L-L, Roze E, et al. Current challenges in the pathophysiology, diagnosis, and treatment of paroxysmal movement disorders. Expert Rev Neurother. 2021;21(1):81–97.
Acknowledgements
We thank the patients and their family members participating in this study. We also thank team staff who assisted in the data collection as well as Dr. Xiaodong Wang, Cipher Gene Ltd. for her assistance in manuscript editing.
Funding
This study was supported by Key Research Project of the Ministry of Science and Technology of China (Grant Nos. 2016YFC0904400 and 2016YFC0904401).
Author information
Authors and Affiliations
Contributions
XYN wrote the article under the supervision of YHZ, while YY, MMC, YS, QZT, JZ had collected relevant case information. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Peking University First Hospital(approval number is 2012 [453]). Parental written informed consent was obtained from patients of all study participants.
Consent for publication
Parental written informed consent was obtained from patients of all study participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Niu, X., Sun, Y., Yang, Y. et al. RHOBTB2 gene associated epilepsy and paroxysmal movement disorder: two cases report and literature review. Acta Epileptologica 3, 20 (2021). https://doi.org/10.1186/s42494-021-00056-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42494-021-00056-y