Abstract
Active surveillance (AS) is the primary strategy for managing patients with low or favorable-intermediate risk prostate cancer (PCa). Identifying patients who may benefit from AS relies on unpleasant prostate biopsies, which entail the risk of bleeding and infection. In the current study, we aimed to develop a radiomics model based on prostate magnetic resonance images to identify AS candidates non-invasively. A total of 956 PCa patients with complete biopsy reports from six hospitals were included in the current multicenter retrospective study. The National Comprehensive Cancer Network (NCCN) guidelines were used as reference standards to determine the AS candidacy. To discriminate between AS and non-AS candidates, five radiomics models (i.e., eXtreme Gradient Boosting (XGBoost) AS classifier (XGB-AS), logistic regression (LR) AS classifier, random forest (RF) AS classifier, adaptive boosting (AdaBoost) AS classifier, and decision tree (DT) AS classifier) were developed and externally validated using a three-fold cross-center validation based on five classifiers: XGBoost, LR, RF, AdaBoost, and DT. Area under the receiver operating characteristic curve (AUC), accuracy (ACC), sensitivity (SEN), and specificity (SPE) were calculated to evaluate the performance of these models. XGB-AS exhibited an average of AUC of 0.803, ACC of 0.693, SEN of 0.668, and SPE of 0.841, showing a better comprehensive performance than those of the other included radiomic models. Additionally, the XGB-AS model also presented a promising performance for identifying AS candidates from the intermediate-risk cases and the ambiguous cases with diagnostic discordance between the NCCN guidelines and the Prostate Imaging-Reporting and Data System assessment. These results suggest that the XGB-AS model has the potential to help identify patients who are suitable for AS and allow non-invasive monitoring of patients on AS, thereby reducing the number of annual biopsies and the associated risks of bleeding and infection.
Similar content being viewed by others
Introduction
Early detection and treatment can effectively reduce prostate cancer (PCa) mortality [1]. However, for some patients diagnosed early, PCa may not pose an immediate threat to health throughout their lifetime. Thus, immediate treatment may not benefit these patients but may result in side effects (i.e., sexual dysfunction, urinary dysfunction, and fatigue) that diminish the quality of life [2, 3].
Active surveillance (AS) refers to regular monitoring of PCa progression, during which curative treatment is administered once PCa evolves into a high-risk tumor [4]. The primary aim of AS is to delay or avoid unnecessary treatment and its corresponding undesirable effects [5]. Therefore, AS has become the primary strategy for managing patients with low- or favorable intermediate-risk (FIR) PCa [6]. According to AS protocols [7, 8], an annual biopsy is required to determine whether patients on AS require reclassification to a higher-risk category. However, repeated biopsies increase pain and the risk of infection [9, 10] and may complicate the execution of radical prostatectomy (RP) [11].
Magnetic resonance imaging (MRI) is a non-invasive imaging method that can provide high spatial resolution and overall morphological characterization of tumors [12, 13]. In particular, the standardized assessment method, known as the Prostate Imaging-Reporting and Data System v.2 (PI-RADSv2), has been reported to be crucial in identifying suitable AS candidates [14, 15]. However, the PI-RADSv2 assessment relies on a semi-quantitative interpretation of MRI images and greatly depends on the radiologist’s experience, resulting in substantial variability in the assessment results among different radiologists [15,16,17]. Additionally, the visual assessment by radiologists may overlook some of the non-visible information from the tumors.
Gaur [18] suggested the use of radiomics in AS for PCa. Radiomics methods can extract high-throughput features, even those not visible to the naked eye from medical images that may reflect tumor phenotypes [19,20,21] and output a quantitative score indicating the risk probability of the tumor [22]. Recent studies have discovered that radiomics methods could predict the progression of AS in patients [23, 24]. For instance, Algohary et al. [23] developed a radiomic model to identify clinically significant PCa in patients undergoing AS. Sushentsev et al. [24] developed a radiomic model to predict the histopathological progression of PCa in patients undergoing AS. However, none of these studies identified suitable AS candidates due to limited sample sizes and the absence of independent external validation [23, 24]. Therefore, the current study aimed to develop and externally validate a radiomics model using a multicenter dataset to non-invasively discriminate patients with PCa who qualify for AS from those who should undergo definitive treatments, such as RP.
Methods
Patients and MRI techniques
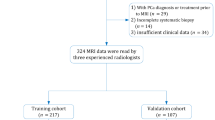
The local Institutional Ethics Review Board approved the study and waived the requirement for written informed consent owing to its retrospective nature. This study adhered to the 1964 Declaration of Helsinki and its subsequent guidelines. Overall, 1,735 consecutive patients who underwent prostate biopsy at six hospitals between January 2018 and June 2021 were enrolled. Based on the inclusion and exclusion criteria (Fig. 1), 956 patients (166, 167, 97, 100, 316, and 110 from hospitals 1 (H1), 2 (H2), 3 (H3), 4 (H4), 5 (H5), and 6 (H6), respectively) were included in the study.
Overview of patients based on the inclusion and exclusion criteria and allocation of patients in the training and external validation cohorts. cT stage: clinical tumor stage; DCE: Dynamic contrast-enhanced; DWI: Diffusion-weighted imaging; mpMRI: Multiparametric magnetic resonance imaging; PSA: Prostate-specific antigen; T2WI: T2-weighted imaging
All patients underwent 3.0-T MRI using an abdominal phased-array coil before prostate biopsy (Supplementary Table S1).
Biopsy analysis, PI-RADS assessment, and lesion annotation
The biopsy results for H1, H2, H4, H5, and H6 were obtained using transrectal ultrasound (TRUS)-guided systemic biopsy and MRI-guided targeted biopsy, and those for H3 were obtained using TRUS-guided saturation biopsy. At each hospital, a junior pathologist analyzed the samples, and the results were verified by a senior pathologist. Disagreements were resolved through discussions between the readers.
According to PI-RADSv2.1 [15], eight junior radiologists (JR1–8) and three experienced radiologists (ER1–3) with over 3 and 18 years of experience, respectively, participated in image interpretation. After the PI-RADS assessment, the same junior radiologist delineated the prostate lesions from the T2-weighted (T2W) images. The delineated lesion was referred to as the region of interest (ROI). The PI-RADS assessment and lesion annotation details are described in Supplementary Sect. 1.
Reference standard
According to the National Comprehensive Cancer Network (NCCN) guidelines [8], patients with PCa undergoing AS meet one of the following criteria: (1) PSA level < 10 ng/mL, cT2b–cT2c, Gleason grade group (GGG) 1, and < 50% positive biopsy cores, or (2) PSA level < 10 ng/mL, cT1–cT2a, GGG 2, and < 50% positive biopsy cores, or (3) PSA level 10–20 ng/mL, cT1–cT2a, GGG 1, and < 50% positive biopsy cores, or (4) PSA level < 10 ng/mL, cT1–cT2a, GGG 1, and < 50% positive biopsy cores. Additionally, the patients with GGG ≥ 3 and ≤ 2 were classified as having clinically significant PCa (csPCa) and non-csPCa, respectively [25].
Development and validation of the radiomics model
Figure 2 illustrates the workflow pipeline of constructing a radiomics models (e.g., eXtreme Gradient Boosting (XGBoost)). Considering the easy acquisition and abundant texture information, T2W images were used to construct the radiomics model [26, 27]. First, images were preprocessed (Supplementary Sect. 2). Next, for each participant, 1,595 radiomics features were extracted from the ROI of the original T2W and the derived images (Supplementary Sect. 3). Then, after feature selection, the radiomics features that were most correlated with the classification were selected from the 1,595 radiomics features (Supplementary Sect. 4). Additionally, XGBoost, logistic regression (LR), random forest (RF), adaptive boosting (AdaBoost), and decision tree (DT) classifiers were used to develop classification models based on the selected radiomic features to identify AS candidates. These radiomics models were referred to as XGBoost AS classifier (XGB-AS), LR AS classifier (LR-AS), RF AS classifier (RF-AS), AdaBoost AS classifier (AdaB-AS), and DT AS classifier (DT-AS), respectively.
AS candidate classification radiomics model workflow pipeline. a MR images were exported through the post-processing workstation. For the lesions on T2W images, the ROI were manually annotated slice by slice; (b) The radiomics features, including shape, texture, histogram, and filter-based features, were extracted; (c) Using a t-test, highly differentiated features were selected to distinguish AS from non-AS candidates. Then, LASSO with a five-fold cross-validation was implemented for further feature selection; (d) Using the features selected by LASSO, a radiomics model was constructed based on the traditional machine learning model (e.g., the XGBoost classifier). Two subgroup analyses were performed to further evaluate this radiomics model’s performance, including distinguishing AS from the ambiguous case group and the immediate-risk group. IR PCa: Immediate-risk prostate cancer; LASSO: Least absolute shrinkage and selection operator; MR: Magnetic resonance
A three-fold cross-center validation was conducted for each model (i.e., LR-AS, RF-AS, AdaB-AS, DT-AS, XGB-AS), with four hospitals used as a training cohort (TC) and the remaining two hospitals used as an external validation cohort (EVC) for each fold of cross-validation, ensuring that the models were multi-center trained and multi-center tested. The details in the data splitting for each fold of the three-fold cross-center were summarized in Supplementary Table S2. Specifically, for the first fold (Fold 1), patients from H1-4 (n = 530) and those from H5-6 (n = 426) were divided into TC and EVC; for the second fold (Fold 2), patients from H1, 2, 5, and 6 (n = 759) and those from H3-4 (n = 197) were divided into TC and EVC; for the third fold (Fold 3), patients from H3-6 (n = 623) and those of H1-2 (n = 333) were divided into TC and EVC.
In each fold of the three-fold cross-center validation, the models were developed using open-source packages in Python (v.3.7), including Scikit-learn and xgboost (v.1.6.2). The hyperparameters for these models were optimized using GridSearch CV. GridSearchCV is a package within the Scikit-learn library that consists of two main elements: grid search, which is used to enumerate the hyperparameters and search for the optimal ones, and cross-validation (five-fold cross-validation for the current study), which is used to assess the model’s performance across different subsets of TC.
Owing to the imbalance between the number of AS and non-AS cases, the classification threshold was determined by the threshold-moving method [28], namely, \(\frac{{n}_{AS}}{{n}_{AS}+{n}_{non-AS}}\), where \({n}_{AS}\) and \({n}_{non-AS}\) refer to the number of AS and non-AS cases in TC of the corresponding fold of the three-fold cross-center validation, respectively (Supplementary Table S2). Thus, if the output score of the radiomics model for a case exceeded the threshold, the case was classified into the AS group; otherwise, it was classified into the non-AS group. In agreement with clinical practice, the non-AS group (requiring immediate treatment) was designated as positive cases, and the AS group was designated as negative cases.
The means of area under the receiver operating characteristic curve (AUC), accuracy (ACC), sensitivity (SEN), and specificity (SPE) for the included radiomics models (i.e., XGB-AS, LR-AS, RF-AS, AdaB-AS, and DT-AS) across the three-fold cross-validation were calculated. AUC reflected the overall performance of the classification model without dependence on the threshold, and therefore, it was used to compare the performance of the models (i.e., XGB-AS, LR-AS, RF-AS, AdaB-AS, and DT-AS) for identifying AS candidates.
Subgroup analysis
Two subgroup analyses were conducted in EVC, using ACC to evaluate the performance of the model, as described below.
-
(1)
Identifying AS candidates with discordance in their assessment results between the PI-RADS [15] and NCCN guidelines [8]: In clinical practice, patients with PI-RADS < 3 are not considered for biopsy due to the relatively low risk of csPCa, whereas those with PI-RADS ≥ 3 necessitate biopsy confirmation due to the relatively high risk of csPCa [15, 29, 30]. However, taking the EVC of Fold 1 as an example, 36 patients among those with PI-RADS < 3 did not qualify for AS, according to the NCCN guidelines [8]. In contrast, 42 patients among those with PI-RADS ≥ 3 (i.e., 34 patients with PI-RADS > 3 and eight patients with PI-RADS = 3) were considered suitable for AS according to the NCCN guidelines [8]. Thus, for these 78 ambiguous cases, we evaluated whether XGB-AS could aid in identifying AS candidates and therefore, reducing the unnecessary biopsies.
-
(2)
Identifying AS candidates from the intermediate-risk group: According to the NCCN guidelines [8], patients with PCa classified as intermediate-risk included those with FIR and unfavorable intermediate-risk (UFIR) (Supplementary Sect. 5). AS was considered as a treatment option for FIR patients but not for UFIR patients [8]. However, differentiating between patients with FIR and those with UFIR based on MRI images is difficult. Therefore, we investigated whether the best-performing model could identify AS candidates in the intermediate-risk group. Also taking the EVC of Fold 1 as an example, 85 patients classified as intermediate-risk (FIR, n = 37; UFIR, n = 48) were selected for this subgroup analysis.
Statistical analyses
To assess the intergroup differences in the proportion of AS candidates between TC and EVC in the three-fold cross-center validation, the χ2 test was performed. Moreover, P < 0.05 indicated statistical significance. The AUC with 95%CIs was used to evaluate performance, and DeLong’s test was used to examine the difference in AUC between the radiomics model and PI-RADS assessment. RStudio (v.4.0.3), Statistical Package for Social Sciences (v.26.0 IBM, Armonk, NY, USA), and Python (v.3.7) were used for statistical analyses.
Results
Patient characteristics
Overall, 956 patients with PCa who underwent 3.0-T MRI at six hospitals were included. The clinical characteristics, demographic information, and distribution of AS and non-AS candidates for included patients are summarized in Table 1. According to the NCCN guidelines [8], for Fold 1, 17.2% of patients (91/530) in TC and 12.9% of patients (55/426) in EVC met the AS criteria; for Fold 2, 15.9% of patients (121/759) in TC and 12.7% of patients (25/197) in EVC met the AS criteria; for Fold 3, 12.8% of patients (80/623) in TC and 19.8% of patients (66/333) in EVC met the AS criteria (Supplementary Table S2).
Model validation and comparison
Table 2 summarizes the means of the AUC, ACC, SEN, and SPE of the included radiomics models (i.e., LR-AS, RF-AS, AdaB-AS, DT-AS, and XGB-AS) for identifying AS candidates across three-fold cross-center validation. As indicated in Table 2, XGB-AS has the highest AUC (0.803) and ACC (0.693). Compared to XGB-AS, DT-AS and AdaB-AS show higher SEN (0.752 vs 0.668) and SPE (0.865 vs 0.841), respectively. However, DT-AS and AdaB-AS presented much lower SPE (0.539 vs 0.841) and SEN (0.491 vs 0.668) when compared to XGB-AS, respectively. These results indicate that XGB-AS exhibits better comprehensive performance in identifying AS candidates than the other models.
For the convenience of description, the XGB-AS models trained and tested in Folds 1, 2, and 3 are referred to as XGB-AS-1, XGB-AS-2, and XGB-AS-3, respectively, whose AUC, ACC, SEN and SPE were summarized in Table 3. As indicated in Table 3, the AUC of XGB-AS-2 is slightly higher than that of XGB-AS-1, which is much higher than that of XGB-AS-3. The detailed optimal hyperparameters of XGB-AS-1, XGB-AS-2, and XGB-AS-3 were summarized in Supplementary Table S3. Additionally, as indicated in Table 3, there is no significant difference in the proportion of AS candidates between TC and EVC for Fold 1 (P = 0.069) or Fold 2 (P = 0.259) of the three-fold cross-center validation. In contrast, such difference is significant for Fold 3 of the three-fold cross-center validation (P = 0.0043), which may be one of the reasons for the decrease in the performance of XGB-AS-3. Thus, to minimize the bias resulting from the patients splitting during the three-fold cross-center validation, the model with the median performance according to AUC (i.e., XGB-AS-1) was selected as the most clinically applicable model, which was used for the subgroup analyses in the corresponding EVC to further validate its clinical performance.
In clinical practice, the PI-RADS assessment is often used to determine whether a biopsy is needed to confirm the presence of csPCa [15]. This can reduce the incidence of unnecessary biopsies by improving the csPCa detection rate [25]. Similarly, XGB-AS-1 was developed to non-invasively identify AS candidates, thereby reducing the need for unnecessary biopsies. Therefore, to reduce unnecessary biopsies, we compared XGB-AS-1 with PI-RADS assessment. In the EVC, XGB-AS-1 yielded an AUC of 0.851 (95%CI: 0.807–0.894) for identifying AS candidates, which was significantly larger than that of the PI-RADS assessment (0.697, 95%CI: 0.643–0.751; P < 0.001; Fig. 3). The ACC, SEN, and SPE of XGB-AS-1 were 0.779 (332/426), 0.771 (286/371), and 0.836 (46/55) in the EVC, respectively. In the PI-RADS assessment, when a threshold of PI-RADS ≥ 3 was employed for detecting csPCa, the ACC, SEN, and SPE in the EVC were reported as 0.735 (313/426), 0.910 (293/322), and 0.192 (20/104), respectively [29, 30].
Subgroup analysis
As revealed by the first subgroup analysis (Fig. 4a), among 78 ambiguous cases characterized by the discordance between the PI-RADS assessment and NCCN guidelines, 78.6% (33/42) of the AS candidates with PI-RADS ≥ 3 and 55.6% (20/36) of the non-AS candidates with PI-RADS < 3 were accurately identified (Fig. 4b). Therefore, XGB-AS-1 had an ACC of 67.9% (53/78) in discriminating the ambiguous cases.
The results of subgroup analysis results for XGB-AS-1. Panels (a) and (b) show the confusion matrix and ACC for distinguishing AS from ambiguous cases with discordance in the assessment results between the PI-RADS assessment and NCCN guidelines, respectively. Panels (c) and (d) show the confusion matrix and ACC for distinguishing FIR patients (AS candidates) from intermediate-risk patients, respectively. The True Label and XGB-AS-1 predicted label indicate the ground truth and classification result of the XGB-AS-1 model, respectively, with 1 for non-AS and 0 for AS. The value in each color check indicates the number of cases for the corresponding True Label and XGB-AS-1 predicted label. XGB-AS-1, the most clinically applicable radiomics model developed in this study based on the XGBoost architecture for identifying AS candidates
As revealed by the second subgroup analysis (Fig. 4c), among the 85 intermediate-risk patients, 83.8% (31/37) of AS and 54.2% (26/48) of non-AS candidates were identified from the FIR and UFIR patients, respectively (Fig. 4d). Therefore, the XGB-AS-1 model had an ACC of 67.1% (57/85) for identifying AS candidates in the intermediate-risk group.
Feature analysis
Table 4 summarizes the features selected for the development of XGB-AS-1. As indicated in Table 4, only three categories of features (i.e., one original feature, nine wavelet features, and three local binary pattern in 3D (LBP-3D) features) were selected by the feature selection process to develop XGB-AS-1 (Supplementary Figure S1). Among these features, when comparing the AS group to the non-AS group, four features (including one original feature, two wavelet features, and one LBP-3D feature) had significantly higher values for the AS group, whereas the remaining nine features (consisting of seven wavelet features and two LBP-3D features) demonstrated significantly lower values for the AS group (P < 0.05).
Discussion
In this study, a radiomics model based on MRI was developed and externally validated to discriminate between AS and non-AS candidates. The results indicated that XGB-AS demonstrated promising performance in identifying AS candidates. According to AS protocols [7, 8], patients on AS must periodically undergo repeat biopsies to determine whether they can continue to follow AS. However, frequent biopsies lead to side effects such as bleeding and infection [9, 10], and a particularly difficult implementation of RP [11]. Furthermore, XGB-AS accurately identified an average of 84.1% of AS candidates. If XGB-AS had been utilized previously, patients with PCa could have avoided unnecessary biopsies, the risk of overtreatment, and potentially challenging RP. Thus, XGB-AS can serve as a primary non-invasive categorization tool, assisting in the accurate identification of AS candidates and avoiding the detrimental effects of repeated biopsies.
In terms of identifying patients with PCa who required biopsy confirmation, XGB-AS displayed better performance than the PI-RADS assessment conducted by experienced radiologists. Moreover, disagreement exists regarding whether biopsy confirmation is required between the PI-RADS assessment [15] and NCCN guidelines [8]. The proposed XGB-AS-1 accurately identified 78.6% (33/42) of AS candidates and 55.6% (20/36) of non-AS candidates from ambiguous cases, with discordance in the assessment results between the PI-RADS assessment and the NCCN guidelines (i.e., the reference standard of the current study). Thus, when patients with PCa were assessed using MRI, our model effectively reduced unnecessary biopsies and enhanced detection SEN and SPE. Therefore, our model may be a potential tool to aid radiologists in the risk stratification of PCa based on non-invasive MRI images. According to clinical practice guidelines [8], an invasive biopsy is necessary for risk stratification of patients with FIR and UFIR. However, utilizing XGB-AS-1, 83.8% (31/37) of the FIR patients who were suitable AS candidates and 54.2% (26/48) of the UFIR patients who were non-AS candidates were correctly identified using MRI. Thus, unnecessary biopsies can be avoided in these patients and early detection can be achieved. These results further underscore the capability of the proposed XGB-AS-1 model to discern subtle differences between AS and non-AS candidates, thereby aiding in identifying AS candidates based on MRI.
Overall, 13 radiomics features that exhibited significant differences in feature values between AS and non-AS candidates were included in XGB-AS-1. Among them, the original _shape_ sphericity was greater for AS than for non-AS. This feature measures the similarity between the shapes of a lesion and a sphere. Thus, our findings suggest that lesions in AS candidates exhibit a more regular shape than those in non-AS candidates. Similar to our findings, Wang et al. [31] reported that the original _shape_ sphericity of adrenal lipid-poor adenomas was greater than that of adrenal metastases. This original_ shape_ sphericity was calculated from the original T2W images rather than from their derived images (e.g., wavelet images). Thus, differences in the original_ shape_ sphericity can provide radiologists and urologists with direct visual and semantic information to determine AS. Additionally, the selected features included wavelet and LBP-3D features, consistent with recent radiomics studies that reported a relationship between these features and tumor progression, as observed in Hodgkin lymphoma [32], cervical cancer [33], and meningioma [34]. Unlike original_ shape_ sphericity, these features are quantified from the derived images and, hence, are not visually represented. However, they comprise most of the selected radiomics features and encompass substantial subtle and invisible information capable of quantitatively characterizing the heterogeneity of PCa. Consequently, they play an important role in the identification of AS candidates.
This study had three limitations. First, although the proposed model was tested using the EVC, the study was retrospective. Future studies should validate and broaden our findings by using prospective data. Second, multicenter cases were manually segmented, which was time-consuming. An automatic segmentation algorithm would be beneficial for future studies. Third, the performance of XGB-AS-1 in ambiguous and intermediate-risk cases is not excellent; perhaps, a more advanced model (i.e., a deep-learning model) has the potential to stratify them accurately. However, the number of ambiguous and intermediate-risk cases in the current dataset was relatively small, rendering it insufficient to train and validate a deep-learning model. Further studies should develop more advanced models with a large amount of data, owing to the clinical significance of the risk re-stratification of ambiguous and intermediate-risk patients.
Conclusions
In conclusion, the proposed radiomics model demonstrated promising performance in identifying candidates for AS, particularly in the classification of AS and non-AS candidates among the patients with PCa considered intermediate risk and those misclassified by the PI-RADS assessment. These findings suggest that the XGB-AS model has the potential to help identify patients who are suitable for AS and allow non-invasive monitoring of patients with AS, thereby reducing the number of annual biopsies and the associated risks of bleeding and infection.
Availability of data and materials
The clinical data used in this study are not available because they contain personal privacy information of patients unless the institutional approvals are obtained and the agreements of data usage are signed. However, the other materials of this study are available through a reasonable request to the corresponding authors.
Abbreviations
- ACC:
-
Accuracy
- AS:
-
Active surveillance
- AUC:
-
Area under the receiver operating characteristic curve
- csPCa:
-
Clinically significant prostate cancer
- EVC:
-
External validation cohort
- FIR:
-
Favorable intermediate-risk
- GGG:
-
Gleason grade group
- H:
-
Hospital
- LBP-3D:
-
Local binary pattern in 3D
- MRI:
-
Magnetic resonance imaging
- NCCN:
-
National Comprehensive Cancer Network
- PCa:
-
Prostate cancer
- PI-RADS:
-
Prostate Imaging-Reporting and Data System
- PSA:
-
Prostate-specific antigen
- ROI:
-
Region of interest
- RP:
-
Radical prostatectomy
- SEN:
-
Sensitivity
- SPE:
-
Specificity
- T2W:
-
T2-weighted
- TC:
-
Training cohort
- TRUS:
-
Transrectal ultrasound
- UFIR:
-
Unfavorable intermediate-risk
- XGB-AS:
-
The radiomics model based on the eXtreme Gradient Boosting architecture for identifying active surveillance candidates
- XGBoost:
-
EXtreme Gradient Boosting
- DT:
-
Decision tree
- LR:
-
Logistic regression
- RF:
-
Random forest
- AdaBoost:
-
Adaptive boosting
- IQR:
-
Interquartile range
- cT:
-
stage clinical tumor stage
- DCE:
-
Dynamic contrast-enhanced
- DWI:
-
Diffusion-weighted imaging
- mpMRI:
-
Multiparametric magnetic resonance imaging
- IR PCa:
-
Immediate-risk prostate cancer
- LASSO:
-
Least absolute shrinkage and selection operator
- MR:
-
Magnetic resonance
References
Hugosson J, Roobol MJ, Månsson M, Tammela TLJ, Zappa M, Nelen V et al (2019) A 16-yr follow-up of the European randomized study of screening for prostate cancer. Eur Urol 76(1):43–51. https://doi.org/10.1016/j.eururo.2019.02.009
Kishan AU, Collins SP (2021) Quality of life after prostate cancer treatment. Int J Radiat Oncol Biol Phys 110(3):727–730. https://doi.org/10.1016/j.ijrobp.2021.03.017
Carter SM, Rogers W, Heath I, Degeling C, Doust J, Barratt A (2015) The challenge of overdiagnosis begins with its definition. BMJ 350:h869. https://doi.org/10.1136/bmj.h869
Sandhu S, Moore CM, Chiong E, Beltran H, Bristow RG, Williams SG (2021) Prostate cancer. Lancet 398(10305):1075–1090. https://doi.org/10.1016/S0140-6736(21)01652-8
Botejue M, Abbott D, Danella J, Fonshell C, Ginzburg S, Guzzo TJ et al (2019) Active surveillance as initial management of newly diagnosed prostate cancer: data from the PURC. J Urol 201(5):929–936. https://doi.org/10.1016/j.juro.2018.10.018
Tosoian JJ, Carter HB, Lepor A, Loeb S (2016) Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol 13(4):205–215. https://doi.org/10.1038/nrurol.2016.45
Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR et al (2016) Active surveillance for the management of localized prostate cancer (cancer care Ontario guideline): American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 34(18):2182–2190. https://doi.org/10.1200/JCO.2015.65.7759
National Comprehensive Cancer Network (NCCN) clinical practice guidelines in oncology: prostate cancer. version 3.2024. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459. Accessed 10 May 2024
Borghesi M, Ahmed H, Nam R, Schaeffer E, Schiavina R, Taneja S et al (2017) Complications after systematic, random, and image-guided prostate biopsy. Eur Urol 71(3):353–365. https://doi.org/10.1016/j.eururo.2016.08.004
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R et al (2013) Systematic review of complications of prostate biopsy. Eur Urol 64(6):876–892. https://doi.org/10.1016/j.eururo.2013.05.049
Fujita K, Landis P, McNeil BK, Pavlovich CP (2009) Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance. J Urol 182(6):2664–2669. https://doi.org/10.1016/j.juro.2009.08.044
Richenberg J, Løgager V, Panebianco V, Rouviere O, Villeirs G, Schoots IG (2019) The primacy of multiparametric MRI in men with suspected prostate cancer. Eur Radiol 29(12):6940–6952. https://doi.org/10.1007/s00330-019-06360-1
Turkbey B, Mani H, Shah V, Rastinehad AR, Bernardo M, Pohida T et al (2011) Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol 186(5):1818–1824. https://doi.org/10.1016/j.juro.2011.07.013
Park JJ, Park BK (2017) Role of PI-RADSv2 with multiparametric MRI in determining who needs active surveillance or definitive treatment according to PRIAS. J Magn Reson Imaging 45(6):1753–1759. https://doi.org/10.1002/jmri.25534
Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ et al (2019) Prostate imaging reporting and data system version 2.1:2019 update of prostate imaging reporting and data system version 2. Eur Urol 76(3):340–351. https://doi.org/10.1016/j.eururo.2019.02.033
Park KJ, Choi SH, Lee JS, Kim JK, Kim MH (2020) Interreader agreement with prostate imaging reporting and data system version 2 for prostate cancer detection: a systematic review and meta-analysis. J Urol 204:661–670. https://doi.org/10.1097/JU.0000000000001200
Sonn GA, Fan RE, Ghanouni P, Wang NN, Brooks JD, Loening AM et al (2019) Prostate magnetic resonance imaging interpretation varies substantially across radiologists. Eur Urol Focus 5(4):592–599. https://doi.org/10.1016/j.euf.2017.11.010
Gaur S (2023) Commentary: considering radiomics in the setting of prostate cancer active surveillance. Eur Radiol 33(6):3789–3791. https://doi.org/10.1007/s00330-023-09295-0
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, De Jong EEC, Van Timmeren J et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14(12):749–762. https://doi.org/10.1038/nrclinonc.2017.141
Algohary A, Shiradkar R, Pahwa S, Purysko A, Verma S, Moses D et al (2020) Combination of peri-tumoral and intra-tumoral radiomic features on bi-parametric MRI accurately stratifies prostate cancer risk: a multi-site study. Cancers 12(8):2200. https://doi.org/10.3390/cancers12082200
Aerts HJWL, Velazquez ER, Leijenaar RTH, Parmar C, Grossmann P, Carvalho S et al (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5:4006. https://doi.org/10.1038/ncomms5006
Ma S, Xie HH, Wang HH, Han C, Yang JJ, Lin ZY et al (2019) MRI-based radiomics signature for the preoperative prediction of extracapsular extension of prostate cancer. J Magn Reson Imaging 50(6):1914–1925. https://doi.org/10.1002/jmri.26777
Algohary A, Viswanath S, Shiradkar R, Ghose S, Pahwa S, Moses D et al (2018) Radiomic features on MRI enable risk categorization of prostate cancer patients on active surveillance: preliminary findings. J Magn Reson Imaging 48(3):818–828. https://doi.org/10.1002/jmri.25983
Sushentsev N, Rundo L, Blyuss O, Nazarenko T, Suvorov A, Gnanapragasam AJ et al (2022) Comparative performance of MRI-derived PRECISE scores and delta-radiomics models for the prediction of prostate cancer progression in patients on active surveillance. Eur Radiol 32(1):680–689. https://doi.org/10.1007/s00330-021-08151-x
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–822. https://doi.org/10.1016/S0140-6736(16)32401-1
Nketiah G, Elschot M, Kim E, Teruel JR, Scheenen TW, Bathen TF et al (2017) T2-weighted MRI-derived textural features reflect prostate cancer aggressiveness: preliminary results. Eur Radiol 27(7):3050–3059. https://doi.org/10.1007/s00330-016-4663-1
Vignati A, Mazzetti S, Giannini V, Russo F, Bollito E, Porpiglia F et al (2015) Texture features on T2-weighted magnetic resonance imaging: new potential biomarkers for prostate cancer aggressiveness. Phys Med Biol 60(7):2685–2701. https://doi.org/10.1088/0031-9155/60/7/2685
Zhou ZH, Liu XY (2006) Training cost-sensitive neural networks with methods addressing the class imbalance problem. IEEE Trans Knowl Data Eng 18(1):63–77. https://doi.org/10.1109/TKDE.2006.17
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378(19):1767–1777. https://doi.org/10.1056/NEJMoa1801993
Kuhl CK, Bruhn R, Krämer N, Nebelung S, Heidenreich A, Schrading S (2017) Abbreviated biparametric prostate MR imaging in men with elevated prostate-specific antigen. Radiology 285(2):493–505. https://doi.org/10.1148/radiol.2017161937
Wang GZ, Kang B, Cui JJ, Deng Y, Zhao Y, Ji CS et al (2023) Two nomograms based on radiomics models using triphasic CT for differentiation of adrenal lipid-poor benign lesions and metastases in a cancer population: an exploratory study. Eur Radiol 33(3):1873–1883. https://doi.org/10.1007/s00330-022-09182-8
Lue KH, Wu YF, Liu SH, Hsieh TC, Chuang KS, Lin HH et al (2020) Intratumor heterogeneity assessed by 18F-FDG PET/CT predicts treatment response and survival outcomes in patients with Hodgkin lymphoma. Acad Radiol 27(8):e183–e192. https://doi.org/10.1016/j.acra.2019.10.015
Liu B, Sun Z, Xu ZL, Zhao HL, Wen DD, Li YA et al (2022) Predicting disease-free survival with multiparametric MRI-derived radiomic signature in cervical cancer patients underwent CCRT. Front Oncol 11:812993. https://doi.org/10.3389/fonc.2021.812993
Zhang J, Yao K, Liu PP, Liu ZY, Han T, Zhao ZY et al (2020) A radiomics model for preoperative prediction of brain invasion in meningioma non-invasively based on MRI: A multicentre study. EBiomedicine 58:102933. https://doi.org/10.1016/j.ebiom.2020.102933
Acknowledgements
The authors are grateful to the First Affiliated Hospital of Soochow University, Second Affiliated Hospital of Soochow University, Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology, Changshu No. 1 People’s Hospital, Beijing Friendship Hospital Affiliated to Capital Medical University, and People’s Hospital of Taizhou for providing data and help for this study.
Funding
This study has received funding by the Beijing Hospital Authority Clinical Medicine Development special funding support, No. ZLRK202333; the Nature Science Foundation of Beijing, No. Z200027; the National Key Research and Development Program of China, No. 2022YFB3203800; the Innovative Research Group Project of the National Natural Science Foundation of China, Nos. 82071887 and 81671656; the Key-Area Research and Development Program of Guangdong Province, No. 2021B0101420005; and the Beijing hospitals Authority 10 Key Construction Projects Funding, No. Q19051-16.
Author information
Authors and Affiliations
Contributions
LW, JGL, CHH conceived the research idea and developed the study design; JB, JH, ZZJ, SLL, JZ, JKS, LBJ, ZK, and LW collected images, manually delineated tumours and assessed PI-RADS scores; SLL, XHL, ZBC, BYY collected clinical data; YWL, LTZ, and JGL performed data analysis; YWL wrote the first draft of the manuscript and coordinated its subsequent revision; LTZ performed code and data review, and was instrumental in revising the manuscript; JGL and LW critically revised the manuscript for important intellectual content. All authors contributed considerably to the study and have approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Y., Zhao, L., Bao, J. et al. Non-invasively identifying candidates of active surveillance for prostate cancer using magnetic resonance imaging radiomics. Vis. Comput. Ind. Biomed. Art 7, 16 (2024). https://doi.org/10.1186/s42492-024-00167-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42492-024-00167-6