Abstract
Introduction
Post-COVID-19 Syndrome (PCS) includes neurological manifestations, especially fatigue and cognitive deficits. Immune dysregulation, autoimmunity, endothelial dysfunction, viral persistence, and viral reactivation are discussed as potential pathophysiological mechanisms. The post-corona-virus immune treatment (PoCoVIT) trial is a phase 2a randomized, controlled, double-blind trial designed to evaluate the effect of methylprednisolone versus placebo on cognitive impairment in PCS. This trial is designed based on the hypothesised autoimmunological pathogenesis and positive aberrations, employing a series of off-label applications.
Methods
Recruitment criteria include a diagnosis of PCS, a minimum age of 18 years and self-reported cognitive deficits at screening. A total of 418 participants will be randomly assigned to either verum or placebo intervention in the first phase of the trial. The trial will consist of a first trial phase intervention with methylprednisolone versus placebo for six weeks, followed by a six-week treatment interruption period. Subsequently, an open second phase will offer methylprednisolone to all participants for six weeks. Outpatient follow-up visits will take place two weeks after each trial medication cessation. The third and final follow-up, at week 52, will be conducted through a telephone interview. The primary outcome measures an intra-patient change of 15 or more points in the memory satisfaction subscale of the Multifactorial Memory Questionnaire (MMQ) from baseline to follow-up 1 (week 8). Key secondary outcomes include long-term intra-patient changes in memory satisfaction from baseline to follow-up 2 (week 20), changes in other MMQ subscales (follow-up 1 and 2), and changes in neuropsychological and cognitive scores, along with assessments through questionnaires focusing on quality of life, fatigue, and mood over the same periods. Exploratory outcomes involve molecular biomarkers variations in serum and cerebrospinal fluid, as well as structural and functional brain magnetic resonance imaging (MRI) parameters changes related to cognition.
Perspective
This trial aims to contribute novel evidence for treating patients with PCS, with a primary focus on those manifesting cognitive deficits. By doing so, it may enhance comprehension of the underlying pathophysiological mechanisms, thereby facilitating biomarker research to advance our understanding and treatment of patients with PCS.
Similar content being viewed by others
Introduction
In late 2019, a new strain of the coronavirus-family, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged. It spread rapidly around the world and precipitated the Coronavirus Disease 2019 (COVID-19) pandemic, thereby significantly impacting global public health [13]. Consequently, many patients continue to experience protracted symptoms, commonly referred to as ‘long-COVID’ or post-COVID-19 syndrome (PCS), a condition that poses a substantial burden to society. PCS exhibits an overall estimated prevalence ranged from 7.5 to 41% in non-hospitalized adults and 37.6% in hospitalized adults [18]. The manifestation of PCS is more common among younger and female patients [3, 6]. PCS is defined by the WHO as a persistent condition, lasting at least three months after infection with broad spectrum of symptoms which may affect all organ systems and impairing daily activity [22]. Cardinal neurological symptoms include fatigue and cognitive deficits [5], which impose a significant impact on quality of life [22]. Patients report a range of cognitive deficits such as concentration difficulties, word-finding difficulties, memory lapses, attention problems and “brain fog”. Systematic neuropsychological assessments reveal deficits in processing speed, executive function, phonemic fluency, category fluency, and memory encoding [2].
Pathophysiological mechanisms underlying the development of PCS and persistent neurological manifestations following SARS-CoV-2 infection revolve around ongoing viral persistence and direct viral invasion, reactivation of latent herpesviridae, endothelial/microcirculatory dysfunction, neuroinflammation, and autoimmunological processes [9, 15, 16, 21]. These potential pathomechanisms involve the overactivation of the immune system, characterized by hyperinflammation and cytokine release. A notable contributor is the post-viral induction of autoimmunity, a well-established mechanism observed in other diseases [16, 21], alongside molecular mimicry, where anti-pathogen antibodies cross-react with host proteins [19].
Based on previous findings, we propose that SARS-CoV-2 triggers an immune response resulting in a dysregulated autoimmune system involving both cellular and humoral components. Preliminary studies of our research group have shown an association of neuronal antibodies present in both serum and cerebrospinal fluid (CSF) and pathological montreal cognitive assessment (MoCA) results in patients with cognitive deficits [9, 16, 21]. Reactive autoantibodies in the central nervous system (CNS), detected in both serum and CSF during SARS-CoV-2 infection, have been consistently observed in a significant proportion of patients [7, 10, 12, 17]. While the role of biomarkers as indicators for CNS damage or involvement in pathophysiological processes remains challenging, they represent potential targets for immunosuppressive treatment. The rationale behind an autoimmune genesis hypothesis suggests that methylprednisolone could be a viable treatment approach. This well-established anti-inflammatory glucocorticoid has proven efficacy in treating various diseases suspected to have an autoimmune aetiology, characterized by inflammatory changes or immune overactivity. Examples include multiple sclerosis, chronic inflammatory demyelinating polyradiculoneuropathy, and steroid-responsive autoantibody related encephalitis [14]. While some of these diseases can be cured completely with corticosteroids, others require repeated pulse therapy. There are several controlled trials that employ corticosteroids, particularly methylprednisolone, at similar doses for autoimmune neurological diseases [8, 24]. The use of glucocorticoids has been explored in acute SARS-CoV-2 infections associated with an excessive inflammatory response [1, 11]. Methylprednisolone holds promise in disrupting various immunological triggers, presenting a well-known, generally well-tolerated, cost-effective, and widely available therapeutic option [14]. Our data indicates that off-label administration of methylprednisolone resulted in subjective improvements and enhanced performance on neuropsychological tests in a high proportion of PCS patients with CSF autoantibodies (data in preparation). This underscores the potential efficacy of the chosen treatment approach within this specific patient cohort. To date, no randomized, placebo-controlled trials have examined the effects of methylprednisolone in patients with PCS primarily characterized by cognitive deficits.
Methods
Objective of the trial
The post-corona-virus immune treatment (PoCoVIT) trial aims to examine the effect of methylprednisolone versus placebo in patients with cognitive deficits in PCS syndrome in a randomized controlled double-blind trial. Additionally, the trial includes exploratory research to identify potential biomarkers, given the frequent occurrence of CNS reactive autoantibodies in the serum and CSF of patients with PCS, particularly those with neurological symptoms such as cognitive deficits. The PoCoVIT trial may enhance our understanding of treatment strategies, thereby improving patient care. Simultaneously, it contributes to biomarker research advancing our understanding of the disease’s pathomechanisms. The objective is not only to demonstrate improvements in clinically relevant and qualitative patient-oriented measures from baseline to week 8 but also to establish correlations between these measures and objective antibody-related mechanistic indicators derived from baseline CSF, neuroimaging, and biomarkers. The second treatment phase, wherein all patients receive methylprednisolone will provide further insights into whether repetitive corticosteroid pulse therapy proves beneficial in symptom control among patients with PCS.
Trial description and design
The PoCoVIT trial is a prospective, single centre trial (OECD category 2) employing a randomized, double blind, placebo-controlled, 2-arm parallel-group design. Patients with predominantly cognitive deficits are enrolled. Figure 1 provides an overview of the main trial procedures. Methylprednisolone serves as the active treatment (verum), and our hypothesis centres on achieving clinically significant improvement following its administration. The primary endpoint is the intra-patient change in Multifactorial Memory Questionnaire (MMQ) subdomain memory satisfaction by ≥ 15 points from baseline to week 8 [25].
Eleven trial visits, detailed in Table 1, including screening, are planned for each patient. The total trial duration for each participant is one year, including two treatment phases, each consisting of 4 weeks of treatment followed by 2 weeks of tapering.
Patients receive trial information and undergo screening before enrolment. At baseline 1 (B1), participants are scanned using cerebral MRI. At baseline 2 and prior to randomization (B2/R), patients complete a neurological and neuropsychological assessment. Blood and optional CSF samples are collected and assessed potential occurrence of autoantibodies. Selected patients, with or without autoantibodies, may be enrolled, following informed consent, in the biomarker and diagnostic platform receiving additional blood analyses and imaging. The biomarker and diagnostic platforms within our centre serve as databases for the identification of diagnostic and prognostic markers associated with PCS, using both imaging data and blood/CSF samples. After randomization, treatment phase 1 unfolds over six weeks, during which patients are randomly assigned to either verum (methylprednisolone) or placebo treatment. Follow-up 1 occurs two weeks post the cessation of trial medication of treatment phase 1. After a four-week treatment break, the second treatment phase begins with all patients receiving methylprednisolone for an additional six weeks. Follow-up 2 occurs two weeks post the cessation of treatment phase 2. Follow-up 3, scheduled 52 weeks after randomization, comprises a telephone interview and patient-completed questionnaires.
During both treatment phases, each participant undergoes safety and monitoring assessments involving blood tests and ultrasound examination for exclusion of deep vein thrombosis of the lower extremity. Detailed documentation of demographic data, medical history, and clinical assessments is conducted during the trial visits (for details refer to Table 1).
Eligibility criteria
Patients with PCS and cognitive deficits will be recruited from the specialised outpatient clinic of the Department of Neurology at Charité. Inclusion and exclusion criteria for the trial population are comprehensively outlined in Table 2. Informed consent from all participants is mandatory and will be documented after the screening visit, ensuring at least a 24-h period before baseline 1.
Arms and intervention
Participants will be stratified based on age (> 50 years or ≤ 50 years), sex and cognitive screening assessment results, as determined by the MoCA at baseline 2 (> 26/30 or ≤ 26/30 points). Randomization will occur in a 1:1 ratio, assigning participants to either the verum or placebo group. The total intervention duration per participant is 20 weeks. The initial six weeks constitute a double-blind intervention with a starting dose of body weight-adjusted methylprednisolone or matching placebo. In the verum group, participants receive oral methylprednisolone at a dose of approximately 1 mg/kg body weight, taken once daily for four weeks followed by a two-week tapering phase. Conversely, in the control group participants receive a matching placebo orally once daily for six weeks, adhering to a comparable titration schedule to maintain blinding. Following the initial six-week blinded intervention, a drug-free period of six weeks ensues. This is followed by a second, unblinded treatment phase lasting the same duration with an equivalent tapering scheme. During this phase, all participants receive methylprednisolone Three follow-up visits (week 8, week 20, and week 52) are scheduled in addition to the six safety visits.
Outcome measures
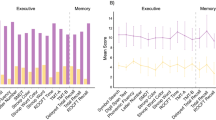
The primary outcome measure is the intra-patient change in the MMQ sub-domain memory satisfaction, demonstrating an increase of ≥ 15 points from baseline to week 8 [25]. Key secondary and safety outcome measures include: (a) Intra-patient change in MMQ sub-domain memory satisfaction from baseline to week 20 and week 52, along with changes from week 8 to week 20, and from week 20 to week 52 (b). Mean difference in MMQ sub-domain memory performance and memory strategy from baseline to week 8, (c) Intra-patient change in neuropsychological and cognitive scores and quality of life measures from baseline to week 8 and week 20, and from week 8 to week 20 (d). Exploratory biomarker-related outcomes encompass the occurrence and change in molecular biomarkers in serum and CSF as well as structural or functional alterations in imaging of cortical and subcortical regions and fibre tracts implicated in neurocognitive processes.
The assessment of investigational medicinal product side effects is conducted through adverse event, serious adverse event, and suspected or unexpected serious adverse reaction reports. Detailed objective measures and outcomes are shown in Table 3.
Sample size calculation and statistical analysis
For the PoCoVIT trial, we aim to detect an improvement in the MMQ sub-domain memory satisfaction. We consider a change of additional 15 points a clinically relevant improvement. Based on our previous data, we anticipate this improvement in 15% of the verum group and 5% of the placebo group. To achieve 90% power at a significance level of α = 0.05, we require 188 patients in each group. This calculation uses a two-sample test for proportions (z-test with arcsine transformation) in the stats package of the R statistical computing environment (version 4.0.2). Assuming a dropout rate of 10%, our recruitment target is 209 patients per group, ensuring that 188 participants remain after dropout. We, therefore, plan to screen 700 patients to enrol the necessary 418, stratified by sex, age, and MoCA score.
Since a single primary outcome is selected, no multiplicity adjustment is required. Analyses of secondary outcomes will be exploratory. For the primary outcome, a binary logistic regression model will be used, focusing on improvement in outcome variables and treatment group as main effects, adjusting for stratification variables. Odds ratios will be reported with 95% confidence intervals, and an alpha of 0.05 has been set for significance. Complete case analysis will be conducted. Where missing values exceed 5%, sensitivity analysis will be performed using multiple imputation chain equations [4].
Secondary outcomes will be initially analysed descriptively and modelled using appropriate techniques such as ANCOVA and logistic models, depending on the outcome distributions. The treatment variable will be included as the main factor adjusting for stratification variables similar to the primary analysis model. Treatment effects will be calculated with two-sided 95% confidence intervals, and outcomes will be analysed in complete cases analyses. Safety, subgroup and interim analyses will be conducted. Statistical analyses will be performed using SAS release 9.2 or higher (SAS Institute Inc., Cary, North Carolina, USA) and R (www.r-project.org) version 4.1.2 or higher.
Contacts
The PoCoVIT trial is conducted within the Nationale Klinische Studiengruppe (NKSG), a clinical trial and translational research platform for the development of treatment in PCS and ME/CFS, funded by the German Ministry of Education and Research (BMBF) [20].
Perspective
This trial is based on the hypothesis that an immune system overactivation triggers sustained hyperinflammation and autoantibody production in PCS. Autoantibodies, including those against neurotransmitter receptors, have been identified in several cohorts of patients with PCS [9, 10]. The identification and specification of relative frequencies are still limited due to the broad spectrum of antibodies. Notably, autoantibodies against G protein-coupled receptors (GPCRs), particularly ß2- and a1-adrenoreceptors, angiotensin II-, muscarinic M2-, MAS-, nociception–, and ETA-receptors, have been found in sera from PCS patients with neurological and/or cardiac symptoms [26]. These autoantibodies correlated with symptom severity (e.g., fatigue, vasomotor and cognitive symptoms) in patients with post-acute sequelae of COVID-19 with chronic fatigue syndrome (PACS-CFS) [23]. Our findings indicate that autoantibodies targeting brain epitopes are common in patients with PCS and strongly associated with pathological cognitive screening test, especially when detected in CSF [9, 10]. However, due to the recent nature of this research, the epitopes and nature of these autoantibodies have not yet been fully characterized.
Evidence regarding the effect of immunosuppressive therapeutics is urgently needed. To date there are no proven therapeutic options to treat patients with PCS, which imposes a significant burden on individuals, society, and the economy. Methylprednisolone, chosen as the active treatment in this trial, is a cost-effective pharmaceutical with demonstrated clinical effectiveness in various immune-mediated diseases. Adverse effects are well described, and safety visits are scheduled accordingly in the PoCoVIT trial. An additional major aim of PoCoVIT is to enhance our understanding of the pathophysiological mechanisms underlying the disease paving the way for potential therapeutic approaches. In PCS, the imperative for adequately powered randomized placebo-controlled trials is evident, seeking to replace controversial experimental therapeutic approaches with evidence-based decision making in the future.
Availability of data and materials
The original contributions presented in the trial are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Abbreviations
- B1:
-
Baseline 1
- B2/R:
-
Baseline 2 and randomization
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- COVID-19:
-
Coronavirus disease 2019
- GPCRs:
-
G protein-coupled receptors
- MRI:
-
Magnetic resonance imaging
- MoCA:
-
Montreal cognitive assessment
- MMQ:
-
Multifactorial Memory Questionnaire
- PoCoVIT:
-
Post-corona-virus immune treatment
- PCS:
-
Post-COVID 19 Syndrome
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
References
Angus, D. C., Derde, L., Al-Beidh, F., Annane, D., Arabi, Y., Beane, A., van Bentum-Puijk, W., Berry, L., Bhimani, Z., Bonten, M., Bradbury, C., Brunkhorst, F., Buxton, M., Buzgau, A., Cheng, A. C., de Jong, M., Detry, M., Estcourt, L., Fitzgerald, M., & Summers, C. (2020). Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: The REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA, 324(13), 1317–1329. https://doi.org/10.1001/jama.2020.17022
Becker, J. H., Lin, J. J., Doernberg, M., Stone, K., Navis, A., Festa, J. R., & Wisnivesky, J. P. (2021). Assessment of cognitive function in patients after COVID-19 infection. JAMA Network Open, 4(10), e2130645. https://doi.org/10.1001/jamanetworkopen.2021.30645
Boesl, F., Audebert, H., Endres, M., Pruss, H., & Franke, C. (2021). A neurological outpatient clinic for patients with post-COVID-19 syndrome - A report on the clinical presentations of the first 100 patients. Frontiers in Neurology, 12, 738405. https://doi.org/10.3389/fneur.2021.738405
Buuren, S., & Groothuis-Oudshoorn, C. (2011). MICE: multivariate imputation by chained equations in R. Journal of Statistical Software. https://doi.org/10.18637/jss.v045.i03
Ceban, F., Ling, S., Lui, L. M. W., Lee, Y., Gill, H., Teopiz, K. M., Rodrigues, N. B., Subramaniapillai, M., Di Vincenzo, J. D., Cao, B., Lin, K., Mansur, R. B., Ho, R. C., Rosenblat, J. D., Miskowiak, K. W., Vinberg, M., Maletic, V., & McIntyre, R. S. (2022). Fatigue and cognitive impairment in post-COVID-19 syndrome: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 101, 93–135. https://doi.org/10.1016/j.bbi.2021.12.020
Chen, C., Haupert, S. R., Zimmermann, L., Shi, X., Fritsche, L. G., & Mukherjee, B. (2022). Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. Journal of Infectious Diseases, 226(9), 1593–1607. https://doi.org/10.1093/infdis/jiac136
Delamarre, L., Gollion, C., Grouteau, G., Rousset, D., Jimena, G., Roustan, J., Gaussiat, F., Aldige, E., Gaffard, C., Duplantier, J., Martin, C., Fourcade, O., Bost, C., Fortenfant, F., Delobel, P., Martin-Blondel, G., Pariente, J., Bonneville, F., Geeraerts, T., & Neuro, I. C. U. R. G. (2020). COVID-19-associated acute necrotising encephalopathy successfully treated with steroids and polyvalent immunoglobulin with unusual IgG targeting the cerebral fibre network. Journal of Neurology, Neurosurgery and Psychiatry, 91(9), 1004–1006. https://doi.org/10.1136/jnnp-2020-323678
Flanagan, E. P., McKeon, A., Lennon, V. A., Boeve, B. F., Trenerry, M. R., Tan, K. M., Drubach, D. A., Josephs, K. A., Britton, J. W., Mandrekar, J. N., Lowe, V., Parisi, J. E., & Pittock, S. J. (2010). Autoimmune dementia: Clinical course and predictors of immunotherapy response. Mayo Clinic Proceedings, 85(10), 881–897. https://doi.org/10.4065/mcp.2010.0326
Franke, C., Boesl, F., Goereci, Y., Gerhard, A., Schweitzer, F., Schroeder, M., Foverskov-Rasmussen, H., Heine, J., Quitschau, A., Kandil, F. I., Schild, A. K., Finke, C., Audebert, H. J., Endres, M., Warnke, C., & Pruss, H. (2023). Association of cerebrospinal fluid brain-binding autoantibodies with cognitive impairment in post-COVID-19 syndrome. Brain, Behavior, and Immunity, 109, 139–143. https://doi.org/10.1016/j.bbi.2023.01.006
Franke, C., Ferse, C., Kreye, J., Reincke, S. M., Sanchez-Sendin, E., Rocco, A., Steinbrenner, M., Angermair, S., Treskatsch, S., Zickler, D., Eckardt, K. U., Dersch, R., Hosp, J., Audebert, H. J., Endres, M., Ploner, J. C., & Pruss, H. (2021). High frequency of cerebrospinal fluid autoantibodies in COVID-19 patients with neurological symptoms. Brain, Behavior, and Immunity, 93, 415–419. https://doi.org/10.1016/j.bbi.2020.12.022
Group, R. C., Horby, P., Lim, W. S., Emberson, J. R., Mafham, M., Bell, J. L., Linsell, L., Staplin, N., Brightling, C., Ustianowski, A., Elmahi, E., Prudon, B., Green, C., Felton, T., Chadwick, D., Rege, K., Fegan, C., Chappell, L. C., Faust, S. N., & Landray, M. J. (2021). Dexamethasone in hospitalized patients with COVID-19. The New England Journal of Medicine, 384(8), 693–704. https://doi.org/10.1056/NEJMoa2021436
Guilmot, A., Maldonado Slootjes, S., Sellimi, A., Bronchain, M., Hanseeuw, B., Belkhir, L., Yombi, J. C., De Greef, J., Pothen, L., Yildiz, H., Duprez, T., Fillee, C., Anantharajah, A., Capes, A., Hantson, P., Jacquerye, P., Raymackers, J. M., London, F., El Sankari, S., & van Pesch, V. (2021). Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. Journal of Neurology, 268(3), 751–757. https://doi.org/10.1007/s00415-020-10108-x
Hu, B., Guo, H., Zhou, P., & Shi, Z. L. (2021). Characteristics of SARS-CoV-2 and COVID-19. Nature Reviews Microbiology, 19(3), 141–154. https://doi.org/10.1038/s41579-020-00459-7
McDaneld, L. M., Fields, J. D., Bourdette, D. N., & Bhardwaj, A. (2010). Immunomodulatory therapies in neurologic critical care. Neurocritical Care, 12(1), 132–143. https://doi.org/10.1007/s12028-009-9274-0
Meinhardt, J., Radke, J., Dittmayer, C., Franz, J., Thomas, C., Mothes, R., Laue, M., Schneider, J., Brunink, S., Greuel, S., Lehmann, M., Hassan, O., Aschman, T., Schumann, E., Chua, R. L., Conrad, C., Eils, R., Stenzel, W., Windgassen, M., & Heppner, F. L. (2021). Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nature Neuroscience, 24(2), 168–175. https://doi.org/10.1038/s41593-020-00758-5
Monje, M., & Iwasaki, A. (2022). The neurobiology of long COVID. Neuron, 110(21), 3484–3496. https://doi.org/10.1016/j.neuron.2022.10.006
Mulder, J., Lindqvist, I., Rasmusson, A. J., Husen, E., Ronnelid, J., Kumlien, E., Rostami, E., Virhammar, J., & Cunningham, J. L. (2021). Indirect immunofluorescence for detecting anti-neuronal autoimmunity in CSF after COVID-19—Possibilities and pitfalls. Brain, Behavior, and Immunity, 94, 473–474. https://doi.org/10.1016/j.bbi.2021.02.013
Nittas, V., Gao, M., West, E. A., Ballouz, T., Menges, D., Wulf Hanson, S., & Puhan, M. A. (2022). Long COVID through a public health lens: An umbrella review. Public Health Reviews, 43, 1604501. https://doi.org/10.3389/phrs.2022.1604501
Nunez-Castilla, J., Stebliankin, V., Baral, P., Balbin, C. A., Sobhan, M., Cickovski, T., Mondal, A. M., Narasimhan, G., Chapagain, P., Mathee, K., & Siltberg-Liberles, J. (2022). Potential autoimmunity resulting from molecular mimicry between SARS-CoV-2 spike and human proteins. Viruses. https://doi.org/10.3390/v14071415
Scheibenbogen, C., Bellmann-Strobl, J. T., Heindrich, C., Wittke, K., Stein, E., Franke, C., Pruss, H., Pressler, H., Machule, M. L., Audebert, H., Finke, C., Zimmermann, H. G., Sawitzki, B., Meisel, C., Toelle, M., Krueger, A., Aschenbrenner, A. C., Schultze, J. L., Beyer, M. D., & Burock, S. (2023). Fighting post-COVID and ME/CFS—Development of curative therapies. Frontiers in Medicine, 10, 1194754. https://doi.org/10.3389/fmed.2023.1194754
Song, E., Bartley, C. M., Chow, R. D., Ngo, T. T., Jiang, R., Zamecnik, C. R., Dandekar, R., Loudermilk, R. P., Dai, Y., Liu, F., Sunshine, S., Liu, J., Wu, W., Hawes, I. A., Alvarenga, B. D., Huynh, T., McAlpine, L., Rahman, N. T., Geng, B., & Farhadian, S. F. (2021). Divergent and self-reactive immune responses in the CNS of COVID-19 patients with neurological symptoms. Cell Rep Med, 2(5), 100288. https://doi.org/10.1016/j.xcrm.2021.100288
Soriano, J. B., Murthy, S., Marshall, J. C., Relan, P., & Diaz, J. V. (2022). A clinical case definition of post-COVID-19 condition by a Delphi consensus. The Lancet Infectious Diseases, 22(4), e102–e107. https://doi.org/10.1016/S1473-3099(21)00703-9
Sotzny, F., Filgueiras, I. S., Kedor, C., Freitag, H., Wittke, K., Bauer, S., Sepulveda, N., Mathias da Fonseca, D. L., Baiocchi, G. C., Marques, A. H. C., Kim, M., Lange, T., Placa, D. R., Luebber, F., Paulus, F. M., De Vito, R., Jurisica, I., Schulze-Forster, K., Paul, F., & Scheibenbogen, C. (2022). Dysregulated autoantibodies targeting vaso- and immunoregulatory receptors in post COVID syndrome correlate with symptom severity. Frontiers in Immunology, 13, 981532. https://doi.org/10.3389/fimmu.2022.981532
Strupp, M., Zingler, V. C., Arbusow, V., Niklas, D., Maag, K. P., Dieterich, M., Bense, S., Theil, D., Jahn, K., & Brandt, T. (2004). Methylprednisolone, valacyclovir, or the combination for vestibular neuritis. New England Journal of Medicine, 351(4), 354–361. https://doi.org/10.1056/NEJMoa033280
Troyer, A. K., & Rich, J. B. (2002). Psychometric properties of a new metamemory questionnaire for older adults. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57(1), P19-27. https://doi.org/10.1093/geronb/57.1.p19
Wallukat, G., Hohberger, B., Wenzel, K., Furst, J., Schulze-Rothe, S., Wallukat, A., Honicke, A. S., & Muller, J. (2021). Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. Journal of Translational Autoimmunity, 4, 100100. https://doi.org/10.1016/j.jtauto.2021.100100
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. The PoCoVIT trial is funded by the Bundesministerium für Bildung und Forschung (German Ministry of Education and Research), Grant 01EP2201.
Author information
Authors and Affiliations
Contributions
CF and HA developed the concept of the studies. HP gave important input to the trial concept. CF and VR wrote the original draft of the paper. FB, BB, AG, LA, IE, AQ, AP, LB, SB, HP, HA, CS reviewed and edited the paper. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Trial registration: 10.3-2023-504826-21-00-B-00318. EU trial number: 2023-504826-21-00. Date of registration: 31.08.2023. The protocol is registered in http://clinicaltrials.gov and has been approved by the ethical review committee of the BfArM (Bundesinstituts für Arzneimittel und Medizinprodukte).
Consent for publication
Not applicable.
Competing interests
All authors are employed at Charité- Universitätsmedizin Berlin. All authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Franke, C., Raeder, V., Boesl, F. et al. Randomized controlled double-blind trial of methylprednisolone versus placebo in patients with post-COVID-19 syndrome and cognitive deficits: study protocol of the post-corona-virus immune treatment (PoCoVIT) trial. Neurol. Res. Pract. 6, 16 (2024). https://doi.org/10.1186/s42466-024-00311-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42466-024-00311-w