Abstract
Background
Endovascular thrombectomy (EVT) is highly effective in acute stroke patients with intracranial large vessel occlusion (LVO), however, presence of concomitant cervical occlusion of the internal carotid artery (ICA) may limit the endovascular access. This study describes feasibility and efficacy of a surgical carotid access (cutdown) to perform interdisciplinary recanalization therapy including carotid endarterectomy (CEA) followed by EVT for recanalization of intracranial LVO in stroke patients with tandem occlusions.
Methods
We identified stroke patients with tandem occlusions who underwent a combined surgical-endovascular approach over a 5-year period. Surgical cutdown was provided by a cardiovascular surgery team at the angio-suite followed by EVT performed by the neuroradiological team. Demographics, stroke characteristics, treatments including antithrombotic management, procedure times, and clinical follow-up were assessed.
Results
Four patients with acute stroke because of tandem occlusions received CEA followed by EVT (two patients after frustrating femoral catheterization, two as first-line approach). Successful recanalization (TICI ≥ 2b) via endovascular thrombectomy was achieved in all patients at a median of 28 min after successful surgical CEA. Intraprocedural complication was observed in one case (25%; i.e. ICA dissection).
Conclusions
This small study provides evidence that a combined interdisciplinary approach of CEA followed by EVT in the angio-suite in acute stroke patients with tandem occlusions is a feasible procedure in patients otherwise not accessible to endovascular recanalizing therapy and, therefore, high likelihood of developing large hemispheric infarction. Prospective data are warranted to identify patients who benefit from this combined approach as first-line therapy.
Similar content being viewed by others
Background
Tandem occlusions of the internal carotid artery (ICA) and middle cerebral artery (MCA) represents a devastating subtype of acute ischemic stroke (AIS) associated with high morbidity and mortality [14]. Acute treatment of these patients reflects a complex and tricky endeavor and is mainly based on endovascular attempts to recanalize ICA followed by MCA [5]. While endovascular thrombectomy (EVT), with or without the addition of intravenous thrombolysis (IVT), is highly effective in AIS patients with intracranial large vessel occlusion (LVO) [6], its power in the aforementioned extreme scenarios involving both intracranial and extracranial vessels is less extensively studied [4]. Given that severe stenosis or occlusion of the cervical ICA limits endovascular access to intracranial LVO, recanalization of long-distance ICA occlusions, including rescue stenting, is required as a first line treatment [2]. However, this attempt, if accomplished at all, is often time-consuming and can lead to delays in intracranial EVT, both of which associated with poor patients’ clinical course [19]. Moreover, peri- and post-procedural clinical management is potentially harmful in light of a necessary intensified antithrombotic management, often including dual antiplatelet therapy and tirofiban [7].
To address this clinical dilemma, an alternative approach of a hybrid rendezvous intervention using surgical carotid endarterectomy (CEA) followed by EVT in these settings has been proposed recently [15, 16]. Yet, these reports rather focused on surgical and technical aspects than reporting clinical neurological data and stressing the potential implications for acute stroke management. Thus, uncertainty remains whether or not this approach is clinically valuable and feasible in daily routine [15, 16]. We here report a case series of acute stroke patients with ICA and MCA tandem occlusions who underwent—on an individual basis and as rescue intervention—combined revascularization of ICA and MCA by CEA followed by EVT within the angiography suite.
Methods
All patients with combined CEA and EVT interventions within the angio-suite were identified from our Giessen stroke registry (GIST; ClinicalTrials.gov Identifier: NCT05295862) which includes all stroke patients treated at the University Hospital Giessen, Germany, over a 5 year-period. Demographics (age, sex), clinical and stroke characteristics (NIHSS, mode and time-point of recanalizing therapies), initial imaging parameters (site of LVO, ASPECT score) and functional outcomes (i.e. modified Rankin scale [mRS]) at discharge and 90 days were extracted from this institutional database. Further, we recorded the time-points of each procedural step in these patients, reviewed medical records and follow-up imaging for antiplatelet treatment regimes, occurrence of complications and final infarct size estimation using ASPECT scores.
Descriptive analyses were performed using SPSS 28.0 (www.ibm.com), presenting absolute numbers (percentages) and median (range) for relevant data in the overall cohort. Individual parameters for each case are reported separately.
Results
Four acute stroke patients with tandem occlusions were treated with the combined interdisciplinary approach including surgical CEA and EVT between 03/2019 and 01/2023 (age range 69-86y; one female patient; see Table 1). Prior cardiovascular comorbidities were frequently present including arterial hypertension, diabetes, chronic kidney disease, coronary heart disease and previous strokes (Table 1). Previous stroke failure known severe ICA-stenosis in 3 of 4 patients (75%). All patients were severely affected (NIHSS 15–21) by AIS due to concomitant occlusion of cervical ICA and ipsilateral MCA at M1-level. Two out of four patients had left-hemispheric stroke, median ASPECT score on initial imaging was 7 (range 6–10).
All four patients underwent combined interventional treatment under general anesthesia (Table 2). The indication for the combined treatment was made on an individual basis and consented among neurologists, neuroradiologists and cardiovascular surgeons.
Unsuccessful endovascular approach and rescue crossover to rendezvous approach
Patients 1 and 2 presented with right-sided ICA occlusions; patient 1 received IVT within established time window, whereas patient 2 presented as wake-up stroke not eligible for IVT. Multimodal imaging confirmed indication for EVT (Fig. 1), groin puncture was performed 63 (patient 1) min, 75 (patient 2) min respectively, after imaging (Table 2). The endovascular approach proved unsuccessful to probe ICA why after 39 min, and 62 min respectively, a crossover to a combined treatment approach was decided (Fig. 2, Table 2). Vascular surgeons took over in the angio-suite and surgical cutdown was performed 23 min, 31 min respectively, later. CEA procedure including implantation of a 6F sheath into the ICA lasted for 61 min, 91 min respectively. Subsequently, the endovascular team performed EVT using a SOFIA aspiration catheter via the implanted sheath (Fig. 2, Table 2). After successful thrombectomy, cervical wound closure was performed by the vascular surgeon. Overall length of procedure was 3:46 h (T0–T5), and 4:47 h respectively (Fig. 2, Table 2).
Initial imaging of patient 1. Non-contrast CT images (A–C) and CT-perfusion imaging including time to peak (TTP; D–F) and cerebral blood volume maps (CBV; G–I) on admission are provided. On initial imaging, minimal early ischemic changes were present (A–C), contrary to the large mismatch (TTP/CBV) detected by perfusion imaging (D–I)
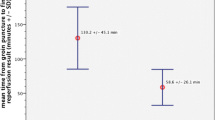
Step-by step illustration of the rendezvous approach. Illustration of the surgical and endovascular hybrid thrombectomy in patient 1. The blue timeline represents procedures performed by the neuroradiological team (NR), while the red one represents those performed by the vascular surgery team (VS). T0–T1: Initially, endovascular access was achieved by puncture of the femoral artery by NR. In the angiography, the internal carotid artery (ICA) did not show contrast enhancement (left) and several attempts to pass-through failed (right) prompting the involvement of the VS team after 0:39 h. T1–T2: The delay until takeover by VS lasted 0:23 h. T2–T3: Within 1:02 h, VS established the surgical access, performed a carotid endarterectomy of the ICA (left), and implanted a carotid sheath (right). T3–T4: NR took over again (left). Middle cerebral artery occlusion at the M1-level was still present (middle) and was recanalized by endovascular thrombectomy via the surgically implanted sheath (right; duration 0:21 h). T4–T5: After thrombectomy, the carotid sheath was removed and the wound was closed by VS (1:22 h). T0–T5: The entire procedure, from initial groin puncture to wound closure, lasted 3:46 h
Direct rendezvous approach without endovascular attempt to recanalize ICA
Following up to both crossover patients reported above, two further patients with similar imaging patterns (patients 3 and 4, Tables 1, 2) received direct surgical cutdown 75 min (patient 3) and 58 min (patient 4) after imaging, respectively, skipping the initial endovascular approach of patients 1 and 2 attempting to recanalize ICA. In essence, indication for this direct combined approach was made as individual decisions in light of in-hospital strokes. Upon qualifying diagnostic imaging both interventional teams consented to perform the direct combined approach. Time saving of this direct rendezvous approach as compared to patients 1 and 2 was > 60 min.
Clinical course and outcomes
Efficacy and safety parameters are presented in Table 3. Successful recanalization (TICI ≥ 2b) was achieved in all patients. Only one relevant intraprocedural complication was reported, i.e. periprocedural dissection of the ICA requiring additional stenting (patient 3). Follow-up imaging 24 h after intervention revealed no significant increase of brain infarction compared to initial imaging (ASPECTS median 7.5; Fig. 3). Clinical course however was serious, with one patient developing multi organ failure leading to DNR/DNT orders and comfort care decisions. 90 day follow up of the other three patients revealed a mRS score of 4 in one patient, whereas the other two patients died after refusing life support including artificial respiration.
Radiological outcome in follow-up imaging. NCCT indicates non-contrast cranial CT. One day post intervention, only a small infarct demarcation was observed in the right insula (A) without any bleeding complication. Nine days post intervention, hemorrhagic transformation within the infarcted region became evident (B)
Discussion
This small study established feasibility and safety of a combined rendezvous approach within the angio-suite for surgical CEA to recanalize ICA, followed by EVT for revascularization of MCA in acute stroke patients. Several aspects emerge from the data.
Tandem occlusions affect approximately 10–15% of stroke patients and are specifically challenging [19]. Some advocate avoiding interventional treatments in such cases and relying solely on intravenous thrombolysis, yet successful reperfusion rate is likely to be insufficient in tandem occlusions [14]. A meta-analysis has shown benefits of thrombectomy for this patient subset, yet uncertainty remains regarding optimal technique to achieve access to intracranial LVO [6, 8]. Specifically, in patients with pre-existing high-grade ICA stenosis, initial endovascular approach appears demanding.
As a consequence, as an alternative technical approach to conventional femoral catheterization for endovascular access to the extra- und intracranial vessels, a direct ultrasound-guided carotid puncture has been proposed [10]. However, this technique harbors some shortcomings, risk of dissection, individual anatomical difficulties as well as post-procedural complications in access site closure [13], all of which undermine its common application in acute stroke patients. Another option involves direct surgical access to the ICA, as demonstrated by vascular surgeons 2019 before the corona lock-down. This study demonstrated the feasibility of surgical access without significant procedural complications, even when systemic thrombolysis was administered concurrently [16]. Yet, scope of this publication were technical aspects and feasibility descriptions addressed at the surgical community without having achieved its well-deserved recognition and creditability among acute neurovascular stroke physicians. Therefore, the present study of a combined surgical and endovascular revascularization may now offer clinical and procedural management information to the community of clinical neurologists, highlighting the feasibility and safety of the combined approach for patients otherwise not treatable by a conventional endovascular approach.
Even if individual risk factors of acute stroke patients are known, the success of femoral access-based recanalization of ICA and MCA remains uncertain in each case. Therefore, one must carefully consider the risk of a futile catheterization attempt delaying recanalization versus the risks associated with a more invasive cutdown approach. In our report, initial cutdown would have saved more than 60 min in those patients who crossed-over after unsuccessful endovascular approach. An additional potential benefit of the combined approach is the lack of ICA stenting (anterograde, stenting first or retrograde, thrombectomy first) performed otherwise during the endovascular approach [19]. As stenting requires dual antiplatelet treatment the subsequent risk of intracranial hemorrhage is increased, specifically in larger infarct volumes [7, 9]. The discussion to prefer balloon catheterization (angioplasty) alone followed by thrombectomy, leaving stenting for a second intervention at a later stage [1], is currently not recommended based on all evidence in light of a higher risk of stroke recurrence and progression rate [18]. Hence, the combined approach with initial surgical cutdown opens up a valuable and clinically feasible avenue, allowing direct CEA with subsequent EVT on a timely basis for patients with tandem occlusions.
Overall, patients with tandem occlusions have a poor prognosis why—in light of all aspects discussed above—interpretation of clinical outcomes in patients with tandem occlusions treated by one or the other approach is tricky [3, 18]. One important aspect refers to the fact that there have been no randomized clinical trials primarily focusing on tandem occlusion patients no far; existing evidence mainly was derived from post-hoc analyses of subsets of patients, why the first RCTs have been initiated such as the EASI-TOC (NCT04261478) and the TITAN (NCT03978988) trials. Hence, the outcomes described here, should not be overrated for the following reasons: patients have had most severe comorbidities prone to decompensation during protracted clinical course of treatment eventually resulting in care limitations and do-not treat orders. Moreover, the patients presented here represent a negative selection of patients presumably not having been eligible for recruitment into respective trials [11, 12]. Thus, even smaller series, specifically those which provide proof-of-principle data, appear valuable preceding subsequent trials [17].
Although the combined approach demonstrated recanalization in all patients in this study, it is important to consider limitations. The small number of cases and the lack of a control group preclude definitive conclusions regarding the superiority of this method over conventional endovascular approaches. Additionally, the decision to pursue a direct surgical cutdown should be carefully evaluated on an individual basis, as done here in those patients with in-hospital strokes only, weighing benefits and risks and taking into account individual risk factors, anatomical considerations, and available resources. Implementing such a collaborative framework requires significant organizational effort and a good understanding of each discipline's role in the procedure.
Conclusions
In conclusion, this case series presents a combined treatment approach involving carotid endarterectomy and thrombectomy for acute stroke patients with tandem occlusions. The findings suggest that in cases where conventional endovascular access is not feasible, direct surgical cutdown may offer a viable alternative to achieve successful recanalization. However, due to the limited number of cases and the complex nature of these patients, cautious interpretation is necessary, and further research is required to determine the broader applicability and potential benefits of this approach in the management of tandem occlusions.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- EVT:
-
Endovascular thrombectomy
- IVT:
-
Intravenous thrombolysis
- ICA:
-
Internal carotid artery
- CEA:
-
Carotid endarterectomy
- LVO:
-
Large vessel occlusion
- AIS:
-
Acute ischemic stroke
- NIHSS:
-
National Institute of Health Stroke Scale
- ASPECT:
-
Alberta stroke program early CT score
- TICI:
-
Thrombolysis in cerebral infarction scale
- mRS:
-
Modified Rankin scale
References
Akpinar, C. K., Gurkas, E., & Aytac, E. (2017). Carotid angioplasty-assisted mechanical thrombectomy without urgent stenting may be a better option in acute tandem occlusions. Interventional Neuroradiology, 23(4), 405–411. https://doi.org/10.1177/1591019917701113
Behme, D., Mpotsaris, A., Zeyen, P., Psychogios, M. N., Kowoll, A., Maurer, C. J., Joachimski, F., Liman, J., Wasser, K., Kabbasch, C., Berlis, A., Knauth, M., Liebig, T., & Weber, W. (2015). Emergency stenting of the extracranial internal carotid artery in combination with anterior circulation thrombectomy in acute ischemic stroke: A retrospective multicenter study. AJNR American Journal of Neuroradiology, 36(12), 2340–2345. https://doi.org/10.3174/ajnr.A4459
Catanese, L., Shoamanesh, A., & Poppe, A. Y. (2021). Tandem occlusions: A tale of two treatments. Stroke, 52(10), 3106–3108. https://doi.org/10.1161/STROKEAHA.121.036219
Eker, O. F., Buhlmann, M., Dargazanli, C., Kaesmacher, J., Mourand, I., Gralla, J., Arquizan, C., Fischer, U. M., Gascou, G., Heldner, M., Arnold, M., Costalat, V., & Mordasini, P. (2018). Endovascular treatment of atherosclerotic tandem occlusions in anterior circulation stroke: Technical aspects and complications compared to isolated intracranial occlusions. Frontiers in Neurology, 9, 1046. https://doi.org/10.3389/fneur.2018.01046
Goyal, M., Demchuk, A. M., Menon, B. K., Eesa, M., Rempel, J. L., Thornton, J., Roy, D., Jovin, T. G., Willinsky, R. A., Sapkota, B. L., Dowlatshahi, D., Frei, D. F., Kamal, N. R., Montanera, W. J., Poppe, A. Y., Ryckborst, K. J., Silver, F. L., Shuaib, A., Tampieri, D., … Investigators, E. T. (2015). Randomized assessment of rapid endovascular treatment of ischemic stroke. The New England Journal of Medicine, 372(11), 1019–1030. https://doi.org/10.1056/NEJMoa1414905
Goyal, M., Menon, B. K., van Zwam, W. H., Dippel, D. W., Mitchell, P. J., Demchuk, A. M., Davalos, A., Majoie, C. B., van der Lugt, A., de Miquel, M. A., Donnan, G. A., Roos, Y. B., Bonafe, A., Jahan, R., Diener, H. C., van den Berg, L. A., Levy, E. I., Berkhemer, O. A., Pereira, V. M., … Collaborators, H. (2016). Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet, 387(10029), 1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Heck, D. V., & Brown, M. D. (2015). Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. Journal of NeuroInterventional Surgery, 7(3), 170–175. https://doi.org/10.1136/neurintsurg-2014-011224
Heider, D. M., Simgen, A., Wagenpfeil, G., Dietrich, P., Yilmaz, U., Muhl-Benninghaus, R., Roumia, S., Fassbender, K., Reith, W., & Kettner, M. (2020). Why we fail: Mechanisms and co-factors of unsuccessful thrombectomy in acute ischemic stroke. Neurological Sciences, 41(6), 1547–1555. https://doi.org/10.1007/s10072-020-04244-5
Marsh, E. B., Llinas, R. H., Hillis, A. E., & Gottesman, R. F. (2013). Hemorrhagic transformation in patients with acute ischaemic stroke and an indication for anticoagulation. European Journal of Neurology, 20(6), 962–967. https://doi.org/10.1111/ene.12126
Mokin, M., Snyder, K. V., Levy, E. I., Hopkins, L. N., & Siddiqui, A. H. (2015). Direct carotid artery puncture access for endovascular treatment of acute ischemic stroke: Technical aspects, advantages, and limitations. Journal of NeuroInterventional Surgery, 7(2), 108–113. https://doi.org/10.1136/neurintsurg-2013-011007
Nguyen, T. N., Raymond, J., Nogueira, R. G., Fischer, U., & Siegler, J. E. (2022). The problem of restrictive thrombectomy trial eligibility criteria. Stroke, 53(9), 2988–2990. https://doi.org/10.1161/STROKEAHA.122.040006
Paraskevas, K. I., de Borst, G. J., & Veith, F. J. (2019). Why randomized controlled trials do not always reflect reality. Journal of Vascular Surgery, 70(2), 607-614 e603. https://doi.org/10.1016/j.jvs.2019.01.052
Roche, A., Griffin, E., Looby, S., Brennan, P., O’Hare, A., Thornton, J., Boyle, K., Williams, D., Moynihan, B., & Power, S. (2019). Direct carotid puncture for endovascular thrombectomy in acute ischemic stroke. Journal of NeuroInterventional Surgery, 11(7), 647–652. https://doi.org/10.1136/neurintsurg-2018-014586
Rubiera, M., Ribo, M., Delgado-Mederos, R., Santamarina, E., Delgado, P., Montaner, J., Alvarez-Sabin, J., & Molina, C. A. (2006). Tandem internal carotid artery/middle cerebral artery occlusion: An independent predictor of poor outcome after systemic thrombolysis. Stroke, 37(9), 2301–2305. https://doi.org/10.1161/01.STR.0000237070.80133.1d
Wiesmann, M., Kalder, J., Reich, A., Brockmann, M. A., Othman, A., Greiner, A., & Nikoubashman, O. (2016). Feasibility of combined surgical and endovascular carotid access for interventional treatment of ischemic stroke. Journal of NeuroInterventional Surgery, 8(6), 571–575. https://doi.org/10.1136/neurintsurg-2015-011719
Wiesmann, M., Kalder, J., Reich, A., Dekeyzer, S., Riabikin, A., Mpotsaris, A., & Nikoubashman, O. (2019). Combined surgical and endovascular carotid access for endovascular thrombectomy in acute ischemic stroke. World Neurosurgery, 132, e1–e4. https://doi.org/10.1016/j.wneu.2019.09.031
Yperzeele, L., Shoamanesh, A., Venugopalan, Y. V., Chapman, S., Mazya, M. V., Charalambous, M., Caso, V., Hacke, W., Bath, P. M., & Koltsov, I. (2023). Key design elements of successful acute ischemic stroke treatment trials. Neurological Research and Practice, 5(1), 1. https://doi.org/10.1186/s42466-022-00221-9
Zevallos, C. B., Farooqui, M., Quispe-Orozco, D., Mendez-Ruiz, A., Dajles, A., Garg, A., Galecio-Castillo, M., Patterson, M., Zaidat, O., & Ortega-Gutierrez, S. (2022). Acute carotid artery stenting versus balloon angioplasty for tandem occlusions: A systematic review and meta-analysis. Journal of the American Heart Association, 11(2), e022335. https://doi.org/10.1161/JAHA.121.022335
Zhu, F., Bracard, S., Anxionnat, R., Derelle, A. L., Tonnelet, R., Liao, L., Mione, G., Humbertjean, L., Lacour, J. C., Hossu, G., Anadani, M., Richard, S., & Gory, B. (2019). Impact of emergent cervical carotid stenting in tandem occlusion strokes treated by thrombectomy: A review of the TITAN collaboration. Frontiers in Neurology, 10, 206. https://doi.org/10.3389/fneur.2019.00206
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was provided.
Author information
Authors and Affiliations
Contributions
NJD, STG, HBH and TRD designed the study, wrote the manuscript and interpreted the data. NJD contributed to data acquisition and analysis. OAO, JK, EM, PRK, TS and TB contributed to data acquisition and interpretation. All authors have revised and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local ethics committee of the Justus-Liebig University, Giessen, Germany (reference AZ 220/21).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Diel, N.J., Gerner, S.T., Alhaj Omar, O. et al. Rendezvous intervention using combined surgical carotid endarterectomy followed by endovascular thrombectomy in patients with acute tandem occlusions: a proof-of-concept experience at a tertiary care center. Neurol. Res. Pract. 5, 60 (2023). https://doi.org/10.1186/s42466-023-00290-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42466-023-00290-4