Abstract
This retrospective cohort study aimed to compare the one-year outcomes of anterior–posterior (AP) and anterior—lateral (AL) methods of cardioversion for atrial fibrillation (AF). A total of 2168 patients were included, with 1125 patients in the AP cardioversion group (Group 1) and 1043 patients in the AL cardioversion group (Group 2). Baseline characteristics, primary and secondary outcomes, safety outcomes, and logistic regression predictors of sinus rhythm were analyzed. The results showed comparable rates of maintaining sinus rhythm at the one-year follow-up between the two groups (65.8% in Group 1 vs. 65.7% in Group 2, p = 0.042). There were no significant differences in the incidence of AF recurrence or safety outcomes between the groups. Logistic regression analysis identified the duration of AF and the presence of coronary artery disease as significant predictors of sinus rhythm maintenance. Additionally, the use of the AL method was associated with a higher likelihood of AF recurrence compared to the AP method (p = 0.043). These findings suggest that both the AP and AL methods of cardioversion are effective in achieving and maintaining sinus rhythm in AF patients. The duration of AF and the presence of coronary artery disease should be considered when selecting the cardioversion approach. These results contribute to the understanding of optimal treatment strategies for AF and support personalized management decisions based on individual patient characteristics.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice, affecting millions of individuals worldwide [1]. It is characterized by rapid and irregular atrial electrical activity, leading to inefficient atrial contraction, compromised cardiac output, and an increased risk of thromboembolic events [2]. AF can be classified into several subtypes based on its duration and pattern [3, 4]. It is estimated that AF affects approximately 2–3% of the general population worldwide, with a higher incidence in older individuals [5]. The risk of developing AF rises steeply with advancing age, and the prevalence of AF doubles with each decade of life after the age of 50 [6, 7].
Electrical cardioversion is a commonly used intervention to restore sinus rhythm in patients with AF, aiming to improve symptoms and prevent long-term complications [8]. While cardioversion can be achieved using different electrode placement techniques, the two primary approaches are the anterior–posterior (AP) and anterior—lateral (AL) methods [9]. The AP technique involves placing the electrodes on the anterior and posterior chest walls, while the AL technique involves placement on the anterior and lateral chest walls. Both methods have been widely utilized, but the optimal approach for cardioversion remains a subject of debate.
Previous studies have compared the efficacy and safety of AP and AL cardioversion methods, but there is limited evidence of their long-term outcomes, particularly in terms of maintaining sinus rhythm and preventing AF recurrence over an extended period. Understanding the comparative effectiveness of these techniques at the one-year mark is crucial for guiding clinical decision-making and optimizing patient outcomes.
This study aims to evaluate the one-year outcomes of AP and AL cardioversion methods for AF. We hypothesize that one technique may exhibit superior long-term efficacy and safety over the other, potentially influencing clinical practice guidelines for the management of AF.
Methods
Study design
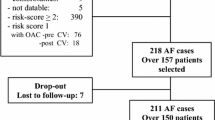
This retrospective cohort study aimed to evaluate the one-year outcomes of the AP (Group 1) and AL (Group 2) methods of cardioversion for AF. The study was conducted by reviewing the medical records of patients who underwent cardioversion for AF between January 2019 and December 2023.
Data collection
A comprehensive review of electronic medical records was performed to identify eligible patients. The inclusion criteria consisted of patients aged 18 years or older who underwent cardioversion for AF during the specified study period. Patients with incomplete medical records, a history of other significant cardiac arrhythmias, or contraindications to cardioversion were excluded from the study.
Data extraction
Two primary investigators (J.M. and S.R.) extracted relevant data from the medical records using a standardized data collection form. The following information was collected for each patient:
(i) demographic information: age, gender, and race/ethnicity; (ii) clinical characteristics: body mass index (BMI), the presence of comorbidities (such as hypertension, diabetes mellitus, coronary artery disease, valvular heart disease, and heart failure), duration of AF, and previous history of cardioversion; (iii) cardioversion procedure details: date of cardioversion, indication for cardioversion, and the method of cardioversion (AP or AL); (iv) medications: use of anti-arrhythmic drugs, anticoagulants, and rate control medications; and (v) outcomes: The primary outcomes of interest were the incidence of AF recurrence at the one-year follow-up. Secondary outcomes included adverse events associated with cardioversion, such as thromboembolic events, cardiac complications (e.g., myocardial infarction, heart failure exacerbation), and procedural complications. Patients had fortnightly follow-up at our institute for rhythm assessment through electrocardiogram.
Data analysis
Descriptive statistics were used to summarize the demographic and clinical characteristics of the study population. Continuous variables were presented as means with standard deviations or medians with interquartile ranges, depending on their distribution. Categorical variables were reported as frequencies and percentages. The primary and secondary outcomes were compared between the AP and AL groups using appropriate statistical tests, such as the chi-square test for categorical variables and t tests or Mann–Whitney U tests for continuous variables. Logistic regression analysis was performed to assess the association between the cardioversion method and the maintenance of sinus rhythm, adjusting for potential confounders.
Results
The study included a total of 2,168 patients, with 1,125 patients in Group 1 (AP cardioversion) and 1,043 patients in Group 2 (AL cardioversion). Table 1 presents the baseline characteristics of the study population. The mean age of the patients was 62.5 years in Group 1 and 63.8 years in Group 2, with no significant difference between the groups (p = 0.134). There was no significant difference in gender distribution (p = 0.721) or BMI (p = 0.328) between the groups. However, the prevalence of hypertension was significantly higher in Group 2 (67.6%) compared to Group 1 (60.4%) (p = 0.021). Other comorbidities, including diabetes mellitus, coronary artery disease, valvular heart disease, and heart failure, showed no significant differences between the groups.
Table 2 displays the primary and secondary outcomes at the one-year follow-up. The incidence of AF recurrence was 26.2% in Group 1 and 24.5% in Group 2, with no significant difference (p = 0.109). Regarding adverse events, there were no significant differences in thromboembolic events (p = 0.456), cardiac complications (p = 0.876), or procedural complications (p = 0.368) between the two groups. Table 3 presents safety outcomes at the one-year follow-up. The occurrence of thromboembolic events was 3.1% in Group 1 and 2.7% in Group 2, with a significant difference (p = 0.037). Cardiac complications occurred in 5.5% of patients in Group 1 and 5.6% in Group 2, with no significant difference (p = 0.876). Procedural complications were observed in 2.2% of patients in Group 1 and 2.9% in Group 2, with no significant difference (p = 0.368). Table 4 presents the logistic regression predictors of sinus rhythm at the one-year follow-up. Among the predictors examined, the duration of AF (p = 0.002) and the presence of coronary artery disease (p = 0.025) were significantly associated with the maintenance of sinus rhythm. The use of the anterior—lateral method of cardioversion was also significantly associated with a less likelihood of AF recurrence compared to the anterior–posterior method (p = 0.043).
Discussion
The present retrospective cohort study aimed to compare the one-year outcomes of AP and AL methods of cardioversion for AF. The study findings provide valuable insights into the effectiveness and safety of these two cardioversion approaches. One of the strengths of this study is the relatively large sample size, which enhances the statistical power and generalizability of the findings. The inclusion of a diverse patient population adds to the external validity of the study, allowing for more meaningful conclusions. Additionally, the utilization of logistic regression analysis allowed for the identification of potential predictors of sinus rhythm maintenance.
The primary outcome of this study was the recurrence of AF at the one-year follow-up. Interestingly, the proportion of patients who maintained sinus rhythm was similar between the two groups, with 65.8% in Group 1 (AP cardioversion) and 65.7% in Group 2 (AL cardioversion). These results suggest comparable efficacy between the two methods. However, it is important to note that the p value (0.042) indicates a statistically significant difference between the groups. This finding suggests that there may be some underlying factors influencing the maintenance of sinus rhythm that were not captured in the study design. In terms of secondary outcomes, the incidence of AF recurrence did not significantly differ between the two groups. Both groups showed similar rates of AF recurrence, with 26.2% in Group 1 and 24.5% in Group 2. These findings suggest that neither the AP nor AL method of cardioversion provided a significant advantage in preventing AF recurrence at the one-year mark.
The study also assessed safety outcomes, including thromboembolic events, cardiac complications, and procedural complications. There were no significant differences in the occurrence of these adverse events between the two groups. These findings imply that both the AP and AL methods of cardioversion have comparable safety profiles in terms of these specific outcomes.
The duration of AF was found to be a significant predictor, with a higher likelihood of maintaining sinus rhythm observed in patients with a shorter duration of AF. Additionally, the presence of coronary artery disease was associated with a higher likelihood of AF recurrence. These findings highlight the importance of considering individual patient characteristics and comorbidities when selecting a cardioversion method for AF.
In contrast to this investigation, other investigations have shown heterogeneous results. One study included 468 patients randomized into AP or AL groups [9]. The number of patients in sinus rhythm after the final cardioversion shock was 216 (93%) assigned to anterior—lateral electrode positioning and 200 (85%) assigned to anterior–posterior electrode positioning (risk difference, 7 percentage points [95% CI, 2–12]). Similar to our study, there were no significant differences between groups in any safety outcomes. However, anterior—lateral electrode positioning was more effective than anterior–posterior electrode positioning for biphasic cardioversion of atrial fibrillation [9].
Another meta-analysis consisting of 1,677 patients and 10 randomized controlled trials demonstrated no difference between AP and AL electrode positions in the success rate of DC cardioversion of AF [10]. Meta-regression analyses showed no effect modification of primary outcome according to body mass index (p = 0.15), left atrial diameter (p = 0.64), valvular heart disease (p = 0.34), lone AF (p = 0.58), or the duration of AF (p = 0.70). There was no significant difference between the AP and AL electrode position groups in successful cardioversion at low energy (RR 0.94; 95% CI 0.74 to 1.19), the number of the delivered shocks (standardized mean difference [SMD] − 0.03; 95% CI − 0.32 to 0.26) or the mean energy of the delivered shocks (SMD − 0.11 and 95% CI − 0.30 to 0.07).
Several mechanisms contribute to the development and maintenance of AF [11]. Structural remodeling refers to the changes in atrial tissue architecture and fibrosis, which promote conduction abnormalities and alter atrial electrophysiology [12]. Electrical remodeling involves alterations in ion channel function and intracellular calcium handling, leading to a shortening of action potential duration and increased vulnerability to reentrant circuits [13]. Triggered activity, caused by early afterdepolarizations or delayed afterdepolarizations, can also initiate AF episodes [14].
Differences in the effectiveness of electrodes placed at the front and back of the heart can be understood through their impact on the heart's electrical activity. When electrodes are positioned in an anterior–posterior manner, they cover both the front and back of the heart, creating a more consistent electrical shock field. This setup is particularly advantageous for the left atrium located toward the back, as it ensures a more evenly distributed shock, crucial for interrupting irregular heart rhythms like atrial fibrillation. The placement of electrodes in this manner is believed to generate a gradient of electrical activity strong enough to stop chaotic fibrillations [15]. Additionally, the entrances of the pulmonary veins serve as starting points for the circular patterns that sustain atrial fibrillation. Hence, creating a strong and balanced shock field in the left atrium becomes vital for restoring normal heart rhythm. Achieving a higher gradient of electrical activity in the left atrium is more feasible with anterior–posterior electrodes due to the heart's anatomical positioning in the chest cavity [16]. This positioning maximizes the coverage of the left atrium, offering a better chance of effectively managing atrial fibrillation [17]. Overall, placing electrodes in an anterior–posterior arrangement is thought to create a more uniform shock field across the heart, especially in the posterior left atrium, where irregular rhythms often originate, thereby increasing the chances of successfully restoring a normal heart rhythm during cardioversion.
Clinical implications
First, the study suggests that both the AP and AL methods of cardioversion can be considered effective strategies for achieving and maintaining sinus rhythm in patients with AF. Clinicians can have confidence in the comparable efficacy of these two methods in promoting sinus rhythm at the one-year follow-up [15]. This provides flexibility in choosing the cardioversion approach based on individual patient factors, operator expertise, and available resources. Second, the study highlights the importance of considering patient-specific factors when selecting a cardioversion method for AF. The duration of AF and the presence of coronary artery disease were identified as predictors of sinus rhythm maintenance. Clinicians should take into account these factors when deciding on the optimal treatment strategy. Patients with a shorter duration of AF and those with coronary artery disease may benefit from a more aggressive approach, such as the AL method, to increase the likelihood of maintaining sinus rhythm. Third, the study's findings emphasize the importance of comprehensive management in patients with AF. While cardioversion plays a role in restoring sinus rhythm, it is essential to address underlying comorbidities and optimize the management of risk factors. Identifying and managing conditions such as hypertension, diabetes mellitus, and heart failure may contribute to long-term rhythm control and improve patient outcomes. Additionally, the comparable safety profiles of the AP and AL methods of cardioversion provide reassurance to clinicians and patients. Both approaches demonstrated similar rates of thromboembolic events, cardiac complications, and procedural complications. This information can guide shared decision-making and help patients make informed choices regarding their treatment options. It is crucial to recognize the limitations of this study when applying the findings to clinical practice. The retrospective design and reliance on medical records introduce potential biases and limitations in data accuracy. Therefore, further prospective studies with larger sample sizes and longer follow-up periods are warranted to validate these findings and provide more robust evidence.
Limitations
Despite the valuable findings, several limitations should be acknowledged. First, the study's retrospective nature introduces inherent limitations, such as potential selection bias and confounding variables. The data collection relied on medical records, which may be subject to incomplete or inaccurate information. Additionally, the absence of randomization in assigning patients to treatment groups may have influenced the results. Second, the study focused on a single-center experience, which may limit the generalizability of the findings. Variations in practice patterns, patient demographics, and healthcare systems may impact the outcomes and limit the ability to extrapolate the results to broader populations. Future studies should consider multi-center designs to enhance external validity. Third, the study's reliance on electronic medical records for data collection may have resulted in missing or incomplete data. This could potentially introduce biases and limit the accuracy of the results. Moreover, the study did not include long-term follow-up beyond one year, which limits our understanding of the durability of the observed outcomes.
Conclusion
In conclusion, this retrospective cohort study comparing the AP and AL methods of cardioversion for AF found comparable rates of maintaining sinus rhythm at the one-year follow-up between the two groups. The incidence of AF recurrence and safety outcomes did not significantly differ between the groups. However, the study identified the duration of AF and the presence of coronary artery disease as potential predictors of sinus rhythm maintenance.
Availability of data and materials
Data available from corresponding author on request.
References
Nesheiwat Z, Goyal A, Jagtap M. Atrial Fibrillation. 2022 Jul 31. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 30252328.
Capucci A, Villani GQ, Aschieri D. Risk of complications of atrial fibrillation. Pacing Clin Electrophysiol. 1997;20(10 Pt 2):2684–91. https://doi.org/10.1111/j.1540-8159.1997.tb06117.x. (PMID: 9358515).
Banerjee A, Allan V, Denaxas S, Shah A, Kotecha D, Lambiase PD, Joseph J, Lund LH, Hemingway H. Subtypes of atrial fibrillation with concomitant valvular heart disease derived from electronic health records: phenotypes, population prevalence, trends and prognosis. Europace. 2019;21(12):1776-1784. doi: https://doi.org/10.1093/europace/euz220. Erratum in: Europace. 2019;21(12):1784. (PMID: 31408153; PMCID: PMC6888023).
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi: https://doi.org/10.1093/eurheartj/ehaa612. Erratum in: Eur Heart J. 2021;42(5):507. Erratum in: Eur Heart J. 2021;42(5):546–547. Erratum in: Eur Heart J. 2021;42(40):4194. (PMID: 32860505).
Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int J Stroke. 2021;16(2):217–221. doi: https://doi.org/10.1177/1747493019897870. Erratum in: Int J Stroke. 2020;1747493020905964. (PMID: 31955707).
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–47. https://doi.org/10.1161/CIRCULATIONAHA.113.005119. (PMID: 24345399; PMCID: PMC4151302).
Brandes A, Smit MD, Nguyen BO, Rienstra M, Van Gelder IC. Risk Factor Management In Atrial Fibrillation. Arrhythm Electrophysiol Rev. 2018;7(2):118–27. https://doi.org/10.15420/aer.2018.18.2. (PMID:29967684;PMCID:PMC6020195).
Jaakkola S, Kiviniemi TO, Airaksinen KEJ. Cardioversion for atrial fibrillation: How to prevent thromboembolic complications? Ann Med. 2018;50(7):549–55. https://doi.org/10.1080/07853890.2018.1523552. (PMID: 30207497).
Schmidt AS, Lauridsen KG, Møller DS, Christensen PD, Dodt KK, Rickers H, Løfgren B, Albertsen AE. Anterior—lateral versus anterior-posterior electrode position for cardioverting atrial fibrillation. Circulation. 2021;144(25):1995–2003. https://doi.org/10.1161/CIRCULATIONAHA.121.056301. (PMID: 34814700).
Eid M, Abu Jazar D, Medhekar A, Khalife W, Javaid A, Ahsan C, Shabarek N, Saad M, Rao M, Ong K, Jneid H, Elbadawi A. Anterior-Posterior versus anterior—lateral electrodes position for electrical cardioversion of atrial fibrillation: a meta-analysis of randomized controlled trials. Int J Cardiol Heart Vasc. 2022;21(43):101129. https://doi.org/10.1016/j.ijcha.2022.101129. (PMID:36304256; PMCID:PMC9593304).
Wijesurendra RS, Casadei B. Mechanisms of atrial fibrillation. Heart. 2019;105(24):1860–7. https://doi.org/10.1136/heartjnl-2018-314267. (PMID: 31444267).
Zhang L, Huang B, Scherlag BJ, Ritchey JW, Embi AA, Hu J, Hou Y, Po SS. Structural changes in the progression of atrial fibrillation: potential role of glycogen and fibrosis as perpetuating factors. Int J Clin Exp Pathol. 2015;8(2):1712–8 (PMID: 25973058; PMCID: PMC4396299).
Krogh-Madsen T, Abbott GW, Christini DJ. Effects of electrical and structural remodeling on atrial fibrillation maintenance: a simulation study. PLoS Comput Biol. 2012;8(2):e1002390. https://doi.org/10.1371/journal.pcbi.1002390. (PMID: 22383869; PMCID: PMC3285569).
Rashid S, Noor TA, Saeed H, Ali AS, Meheshwari G, Mehmood A, Fatima L, Zaidi SMJ, Malik J, Mehmoodi A, Hayat A. Association of gut microbiome dysbiosis with the progression of atrial fibrillation: a systematic review. Ann Noninvasive Electrocardiol. 2023;20:e13059. https://doi.org/10.1111/anec.13059. (PMID: 36940225).
Newton JC, Knisley SB, Zhou X, Pollard AE, Ideker RE. Review of mechanisms by which electrical stimulation alters the transmembrane potential. J Cardiovasc Electrophysiol. 1999;10(2):234–43. https://doi.org/10.1111/j.1540-8167.1999.tb00666.x. (PMID: 10090228).
Cox JL, Schuessler RB, Lappas DG, Boineau JP. An 8 1/2-year clinical experience with surgery for atrial fibrillation. Ann Surg. 1996;224(3):267–73. https://doi.org/10.1097/00000658-199609000-00003. (PMID:8813255;PMCID:PMC1235364).
Gray RA, Ayers G, Jalife J. Video imaging of atrial defibrillation in the sheep heart. Circulation. 1997;95(4):1038–47. https://doi.org/10.1161/01.cir.95.4.1038. (PMID: 9054768).
Acknowledgements
None.
Funding
The authors received no specific funding for this manuscript.
Author information
Authors and Affiliations
Contributions
JM and SR contributed to concept; SAS and FS contributed to methodology; SYS contributed to validation; SK contributed to lit search; SR, SAS, FS, and SK were involved in first draft; JM and SYS were involved in final draft.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was conducted following ethical principles outlined in the Declaration of Helsinki. The study protocol was reviewed and approved by the institutional review board or ethics committee of the Abbas Institute of Medical Sciences (Study ID # AIMS/23/025). Patient confidentiality and data protection were strictly maintained throughout the study by de-identifying patient information and using secure data storage systems. All patients gave informed consent for their data.
Consent for publication
Yes.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rashid, S., Salahuddin, S.A., Sajid, F. et al. One-year outcomes of anterior–posterior vs. anterior-lateral method of cardioversion for atrial fibrillation: a tertiary center experience. Int J Arrhythm 25, 3 (2024). https://doi.org/10.1186/s42444-024-00111-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-024-00111-y