Abstract
In the context of ARVC, a systematic review of the validation of the ARVC risk score can provide insights into the accuracy and reliability of this score in identifying patients at high risk of ARVC. Digital databases were searched to identify the relevant studies using Medical Subject Headings (MeSH). A total of 8 studies were included in this systematic review. A total of 8 studies were included in this review. The review found that the sensitivity of the ARVC risk scores ranged from 80 to 95%, and the specificity ranged from 31 to 79%. The PPV was 55%, and the NPV was 88%. The ARVC score provided a C-index for a 5-year VA risk prediction of 0.84 [95% CI (0.74–0.93)] and a Harrell C-index of 0.70 (95% CI 0.65–0.75). The calibration slope was 1.01 (95% CI 0.99–1.03). ARVC score demonstrated a significant event 5-year threshold between 15 and 20% and the classical ARVC 5-years/freedom-from-VA rate was 0.76(0.66–0.89) and the non-classical form 5-years/freedom-from-VA rate was 0.58 (0.43–0.78). In conclusion, the validation of ARVC risk scores is an essential step toward improving the accuracy of ARVC diagnosis and risk stratification. Further studies are needed to establish the accuracy and reliability of ARVC risk scores and to address the limitations of the current evidence.
Similar content being viewed by others
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a genetic disorder of the heart that increases the risk of life-threatening ventricular arrhythmias (VA) and sudden cardiac death (SCD), particularly in the young population and athletes [1,2,3,4,5,6,7,8]. Early diagnosis of ARVC is essential for effective risk stratification and prompt initiation of treatment to prevent SCD, and an implantable cardioverter defibrillator (ICD) is a cornerstone of primary and secondary prevention [3]. However, the diagnosis of ARVC remains challenging due to its heterogeneous presentation, and its subjectivity limits current diagnostic criteria [1]. To address this issue, various risk scores have been proposed to improve the accuracy of ARVC diagnosis [5, 6].
ARVC risk scores are tools used by healthcare professionals to assess the risk of adverse events, such as ventricular arrhythmias and sudden cardiac death, in individuals with ARVC. These risk scores are valuable for guiding treatment decisions, including the implantation of defibrillators, which can shock the heart back into a normal rhythm if a dangerous arrhythmia occurs. One of the most widely used tools for assessing ARVC risk is the ARVC Risk Stratification Score [5]. This score incorporates various key factors such as the presence and frequency of ventricular arrhythmias, family history of sudden cardiac death, specific electrocardiographic abnormalities, and the extent of right ventricular involvement as seen in imaging studies [3]. By considering these elements, healthcare providers can categorize patients into different risk groups, enabling them to tailor treatment plans accordingly. Another critical aspect of ARVC risk assessment is genetic testing. Genetic mutations are often associated with ARVC, and identifying these mutations in patients and their family members can significantly influence risk stratification. Certain genetic mutations are linked to a higher likelihood of developing ARVC and experiencing severe arrhythmias. Therefore, genetic testing plays an essential role in refining ARVC risk scores and guiding personalized management approaches [1,2,3,4,5,6,7,8].
In the context of ARVC, a systematic review of the validation of ARVC risk scores can provide insights into the accuracy and reliability of these scores in identifying patients at high risk of ARVC. The review results can provide important information for clinicians and researchers in making informed decisions about using ARVC risk scores for the ARVC risk of SCD. Overall, validating ARVC risk scores is a crucial step toward improving the accuracy of ARVC diagnosis and reducing the risk of sudden cardiac death in affected individuals. A systematic review of the available evidence can provide valuable insights into the reliability and usefulness of these scores and guide the development of improved diagnostic strategies for ARVC.
Methods
This review followed the Preferred Reporting Items in Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines and data from the original articles included in this review can be obtained in the reference section and Table 1 [9].
Search strategy and selection criteria
PubMed/MEDLINE, EMBASE, Web of Science, CINAHL, and Scopus were searched using various Medical Subject Headings (MeSH) combinations to identify the relevant studies. No time filters and language restrictions were placed on the search algorithm and backward snowballing was used to identify missing articles in the primary search. The MeSH consisted of the following words: “arrhythmogenic right ventricular cardiomyopathy” OR “arrhythmogenic right ventricular dysplasia” OR “ARVC” OR “ARVD” AND “ARVC risk calculator” AND “external validation” OR “internal validation” OR “efficacy” OR “sensitivity.” The Boolean operators were used to combine the subsets, and the results were downloaded into the Covidence library.
Two investigators (M.M. and J.M.) reviewed the titles and abstracts independently. The studies showing validation of the ARVC risk calculator by Marcus et al. were selected for full-text review. They included randomized controlled trials and other observational studies for this study question. All other manuscripts, including case reports, preprints, conference papers, and editor letters, were excluded. All data were validated by the lead author (J.M.); in case of missing data, authors of the original manuscripts were contacted for data review. The last search ended on Feb 14, 2023.
Data extraction/data analysis and quality assessment
The two authors extracted data about the patient demographics, 2020 Task Force Criteria for ARVC diagnosis, and validation parameters (J.B. and J.M.). Detailed patient-level and study-oriented characteristics were abstracted in Table 1. The statistical analysis was performed using the standard statistical analysis software (The Statistical Package for Social Sciences version 26). Continuous data were presented as mean and standard deviation (SD), while categorical data were presented as frequency (n) and percentages (%).
The overall quality of the studies was assessed using the Oxford Quality Scoring System (Jadad) for RCTs, and the Newcastle–Ottawa scale was used for the assessment of observational studies. The study quality is presented in Additional file 1: Fig. S1.
Results
Search results
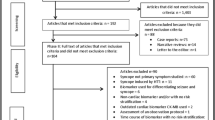
In general, 37 records were searched using the databases. After the removal of duplicates (25) and irrelevant items (2), 10 papers were screened for their titles and abstracts. Ultimately, 8 studies were identified as potentially eligible for our systematic review. The retrieval process flowchart is shown in Fig. 1.
Study outcomes
All study-level characteristics are shown in Table 1 [1,2,3,4,5,6,7,8]. Aquaro (2020) conducted a retrospective cohort study involving 140 participants to assess Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) risk using different criteria, including the ITFC consensus statement, HRS criteria, and an ARVC risk score. The ARVC risk score demonstrated high sensitivity (95%) but relatively low specificity (31%) for predicting major events. It was noted that using a 5-year ARVC risk score > 10% could prevent more events compared to other criteria but at the expense of increased ICD implantations. In the same cohort, Aquaro (2020) also compared the sensitivity and specificity of cardiac magnetic resonance imaging (CMR) and the ARVC risk score. CMR had a sensitivity of 75% and specificity of 67%, while the ARVC risk score had a higher sensitivity of 83% but lower specificity (39%). The study also explored factors such as left ventricular (LV) involvement in ARVC presentations. Gasperetti (2020) conducted a prospective cohort study with 25 participants to assess ARVC risk using the 2010 Task Force Criteria and the ARVC risk score. The study found that clinical detraining had a positive effect on reducing arrhythmias but did not significantly reverse remodeling of right ventricular ejection fraction (RVEF). Casella (2020) conducted a retrospective cohort study involving 101 participants to compare ITFC risk assessment models with an ARVC risk calculator. The ARVC risk calculator appeared effective in predicting arrhythmic risk in classical ACM forms but underperformed in non-classical forms. The study suggested that an integration with invasive assessment techniques might be necessary in cases with early left ventricular involvement. Baudinaud (2021) conducted a retrospective cohort study with 128 participants, using the 2015 ARVC Task Force Consensus criteria and an ARVC risk score. The ARVC risk score showed a sensitivity of 80% and specificity of 79%. During the follow-up, the model provided good discrimination for predicting ventricular arrhythmias. However, it tended to overestimate the risk when applying certain thresholds. Carrick (2022) conducted a retrospective cohort study with 408 participants, utilizing an ARVC risk calculator. The study found that cumulative ventricular arrhythmia (VA)-free survival at 5 years was 71.3%. The study identified several predictors of VA events, including left ventricular ejection fraction (LVEF), anti-arrhythmic medications, exercise, beta-blockers, non-sustained ventricular tachycardia (NSVT), T-wave inversion, and right ventricular (RV) dysfunction. Jorda (2022) conducted a retrospective cohort study with 429 participants, using an ARVC risk calculator. The study revealed that the ARVC risk prediction model provided accurate prognostic information, especially in patients without a prior history of sustained ventricular arrhythmias (VA) at diagnosis. It generally outperformed other published decision algorithms in predicting long-term arrhythmic risk. Protonotarios (2022) conducted a retrospective cohort study with 554 participants, assessing ARVC risk using an ARVC risk score. The corrected 2019 ARVC risk score demonstrated reasonable discriminative ability but tended to overestimate risk. Its performance was better among gene-positive patients, especially in the PKP2 subgroup, but less effective in gene-elusive patients. The predictive power of individual risk markers varied by genotype.
Discussion
The review identified 8 studies evaluating the ARVC risk score proposed in the literature. All studies included a diverse range of populations, including patients with ARVC, healthy controls, and patients with other cardiac conditions. The studies used various measures of accuracy, such as sensitivity, specificity, positive predictive value, and negative predictive value, to evaluate the performance of the ARVC risk scores. The results of the review suggest that the validation of ARVC risk scores is still in its early stages, and further studies are needed to establish the accuracy and reliability of these scores. The review found that the sensitivity of the ARVC risk scores ranged from 80 to 95%, and the specificity ranged from 31 to 79%. The PPV was 55%, and the NPV was 88%. The variability in the performance of the ARVC risk scores across studies can be attributed to differences in the populations, the methods used to validate the scores and the diagnostic criteria used for ARVC.
ARVC is a rare, inherited heart disorder that primarily affects the right ventricle, one of the heart's four chambers [1]. This condition is characterized by the progressive replacement of normal heart muscle tissue with fatty and fibrous tissue, leading to structural and functional abnormalities in the right ventricle. ARVC is also known by various names, including Arrhythmogenic Right Ventricular Dysplasia (ARVD) or Arrhythmogenic Cardiomyopathy (ACM). ARVC is primarily a genetic disorder, with several identified genetic mutations associated with its development [9, 10]. These mutations often follow an autosomal dominant inheritance pattern, meaning that an affected individual has a 50% chance of passing the mutation on to their offspring [11]. Mutations in genes encoding proteins involved in cell-to-cell adhesion in the heart, such as desmosomes, are commonly implicated in ARVC. The clinical manifestations of ARVC can vary widely among affected individuals. Some individuals may remain asymptomatic for an extended period, while others may experience a range of cardiac symptoms, including palpitations, arrhythmias, chest pain, and, in severe cases, heart failure [12]. One of the most critical and life-threatening complications of ARVC is the risk of ventricular arrhythmias, which can lead to sudden cardiac death, especially in young individuals and athletes [13]. Diagnosing ARVC can be challenging due to its heterogeneous presentation. The 2020 Task Force Criteria for ARVC diagnosis is a widely accepted set of guidelines used by clinicians to evaluate patients suspected of having ARVC [14]. These criteria include clinical, electrocardiographic, imaging, and genetic factors to make a comprehensive diagnosis [12]. In recent years, researchers and clinicians have explored the use of ARVC risk scores to improve the accuracy of diagnosis and risk stratification. These risk scores incorporate various clinical and genetic factors to assess an individual's risk of developing ventricular arrhythmias and other complications associated with ARVC [1,2,3,4,5,6,7,8]. Validation studies have shown promising results, with some risk scores demonstrating improved sensitivity compared to traditional diagnostic criteria. ARVC risk scores are instrumental tools in addressing the diagnostic challenges posed by this complex and potentially life-threatening heart condition [7, 8]. ARVC is notorious for its variable clinical presentation, making accurate diagnosis a formidable task. Traditional diagnostic criteria, such as the 2020 Task Force Criteria, while valuable, are not without limitations, particularly in terms of sensitivity and specificity [14]. ARVC risk scores, therefore, play a pivotal role in improving diagnostic accuracy and risk assessment. These risk scores are essentially mathematical models or algorithms that integrate a range of clinical, imaging, and genetic factors to provide a comprehensive assessment of an individual's risk of ARVC. Their primary objective is to offer a more accurate evaluation, especially when dealing with cases featuring atypical or subtle clinical features [2,3,4,5]. By incorporating multiple dimensions of patient data, these scores can assist clinicians in making more informed decisions about diagnosis and risk stratification. The components of ARVC risk scores are multifaceted. They encompass clinical factors, including the presence of symptoms like palpitations, syncope, chest pain, and a family history of ARVC or sudden cardiac death. Additionally, abnormal ECG findings, such as specific arrhythmias or ECG changes, may contribute to the score. Cardiac imaging data, such as echocardiography, MRI, or CT, are critical for revealing structural abnormalities in the right ventricle and are thus included in the risk assessment [15,16,17,18,19]. Furthermore, genetic testing, which identifies mutations in genes linked to ARVC, particularly those associated with desmosomes, can serve as a potent risk factor and is incorporated into some risk scores [20,21,22,23,24]. In specific cases, exercise stress testing may also be employed as part of risk assessment, given that ARVC symptoms can manifest or worsen during physical exertion [25]. It is imperative to underscore that the development and validation of ARVC risk scores are ongoing processes. Validation studies are essential to assess the accuracy and reliability of these scores across diverse patient populations. Additionally, as our understanding of ARVC continues to evolve, refinements and updates to these risk scores may be necessary to enhance their predictive power and clinical utility. Collaborative efforts among researchers, clinicians, and geneticists are critical in achieving more accurate and personalized risk assessments for ARVC, ultimately leading to improved patient outcomes and better management of this challenging cardiac condition. ICDs are efficient in preventing SCD in patients with ARVC, especially in young individuals [26,27,28,29]. However, despite significant efforts, guidelines on ICD placement in ARVC are still based on expert consensus, which can lead to several unnecessary implantations. Hence, there is a need for a validated and tested risk score similar to hypertrophic cardiomyopathy, which should be implemented in guidelines after extensive validation studies. In one study by Cadrin-Tourigny et al., the ARVC risk score resulted in a 20.6% reduction in ICD placement as compared with the 2015 consensus, at the same level of protection (89.9%) [10]. In Baudinaud et al., the model successfully discriminated against patients with ventricular arrhythmia during follow-up [4]. However, there was significant risk overestimation in the low-risk group. Similarly, Aquaro et al. conducted a validation study of the ARVC risk score in a cohort of 140 patients [1]. The ARVC score discriminated against patients with ventricular arrhythmias well during follow-up and was superior to ITFC and HRS criteria. Protonotarious et al. noticed a good accuracy of the ARVC risk score but revealed a much lower event rate and a significant overestimation of risk compared with the original paper [8]. The main implication of this paper was the incorporation of genotype in future iterations of risk models in ARVC. Ethnic differences must also be added to the complexity and left predominant ARVC may require such prediction models for future research.
Diagnosing ARVC requires a comprehensive evaluation based on clinical, imaging, histological, and genetic criteria [14]. The diagnostic process aims to establish a definitive diagnosis while considering the hereditary nature of the disease and its potentially life-threatening consequences. Below is an expanded discussion of the diagnostic criteria for ARVC:
Clinical evaluation is the initial step in the diagnosis of ARVC and involves a thorough assessment of the patient's medical history and physical examination. Key clinical features that may raise suspicion of ARVC include Ventricular arrhythmias. Identification of ARVC in close relatives, especially in a pattern consistent with autosomal dominant inheritance, warrants further investigation. Symptoms such as exercise intolerance, palpitations, syncope, and dyspnea, may indicate ventricular dysfunction. Specific findings on physical examination, including abnormal heart sounds, murmurs, or signs of right heart failure. Cardiac imaging plays a crucial role in diagnosing ARVC and includes a combination of various modalities: [30,31,32,33,34,35,36].
Echocardiography: Transthoracic echocardiography (TTE) is the initial imaging modality to assess right ventricular size, function, and wall motion abnormalities. Findings such as localized wall motion abnormalities and right ventricular dilatation are suggestive of ARVC. Cardiac MRI is highly sensitive for detecting structural abnormalities, particularly fat infiltration and fibrosis within the right ventricle. Late gadolinium enhancement (LGE) on MRI is a hallmark of ARVC and indicates myocardial fibrosis. Right Ventriculography: Right ventriculography can reveal regional wall motion abnormalities, especially during electrophysiological studies. Endomyocardial biopsy is sometimes necessary to obtain histological evidence of fibrofatty replacement of myocardium, supporting the diagnosis of ARVC. However, it is important to note that endomyocardial biopsy has low sensitivity. It is usually reserved for cases with atypical clinical and imaging features or when other diagnostic tests are inconclusive. ARVC is often considered a genetic disorder, and genetic testing can be instrumental in confirming the diagnosis. Genetic testing can identify mutations in genes associated with ARVC, such as PKP2, DSP, DSG2, DSC2, and others. A positive genetic test, in combination with clinical and imaging findings, strengthens the diagnosis and helps identify at-risk family members [37,38,39].
The treatment of ARVC is a multifaceted approach aimed at managing symptoms, preventing life-threatening arrhythmias, and reducing the risk of sudden cardiac death. Medications play a pivotal role in ARVC management [13, 40,41,42,43,44,45,46,47,48]. Anti-arrhythmic drugs like beta-blockers, amiodarone, and sotalol are commonly prescribed to stabilize the heart's electrical activity and minimize the occurrence of dangerous arrhythmias. Additionally, medications for heart failure, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), may be used to manage heart failure symptoms and improve overall heart function in cases where ARVC has progressed to heart failure. Lifestyle modifications are integral to ARVC management [42]. Patients are often advised to restrict their participation in high-intensity or competitive sports and activities due to the heightened risk of sudden cardiac death associated with ARVC. The level of restriction is tailored to individual risk factors and the severity of the condition. Furthermore, limiting or avoiding substances like alcohol, caffeine, and certain medications known to stimulate the heart can help reduce the risk of arrhythmias. Maintaining a healthy body weight through weight management is also crucial in alleviating strain on the heart and decreasing the risk of heart failure. ICDs are a vital component of ARVC treatment for individuals at high risk of life-threatening ventricular arrhythmias. These devices continuously monitor the heart's rhythm and can deliver a shock to restore normal rhythm during a dangerous arrhythmia [49,50,51]. ICDs serve as a crucial safety net, providing immediate intervention when needed and significantly improving survival rates in ARVC patients. In some cases, catheter ablation may be considered as a minimally invasive procedure to treat arrhythmias associated with ARVC. This procedure involves the use of catheters to deliver radiofrequency energy or cryotherapy to specific areas of the heart, disrupting abnormal electrical pathways. Catheter ablation can be an effective option when medications alone are insufficient in controlling arrhythmias. In the most severe cases of ARVC, heart transplantation may be contemplated as a last-resort treatment option [52,53,54,55,56,57]. This involves replacing the damaged heart with a healthy donor heart. However, heart transplantation is considered when ARVC has led to end-stage heart failure or when recurrent, life-threatening arrhythmias cannot be controlled by other therapeutic measures. Given the genetic basis of ARVC, individuals diagnosed with the condition are often advised to seek genetic counseling. Genetic counseling provides crucial information about the inheritance pattern of ARVC, enabling individuals to make informed decisions regarding family planning and understand the potential genetic implications for their relatives.
Limitations
The review also found that most of the studies were limited by their small sample size, retrospective design, and lack of randomized fashion. These limitations highlight the need for larger, prospective studies that can provide more robust evidence on the accuracy and reliability of ARVC risk scores. In addition, the review identified several areas that require further research, such as the validation of the ARVC risk score in asymptomatic individuals and the development of risk scores that incorporate genetic testing and imaging modalities. Despite the limitations of the current evidence, the review suggests that the ARVC risk score has the potential to improve the accuracy of ARVC diagnosis and risk stratification. The use of risk scores can help identify patients at high risk of ARVC, who can benefit from early intervention and close monitoring. In addition, the use of risk scores can reduce the variability in the diagnosis of ARVC and improve the consistency of clinical practice.
Conclusion
In conclusion, the validation of ARVC risk scores is an essential step toward improving the accuracy of ARVC diagnosis and risk stratification. The current evidence on the validation of ARVC risk scores is limited by small sample sizes, retrospective designs, and lack of external validation. Further studies are needed to establish the accuracy and reliability of ARVC risk scores and to address the limitations of the current evidence. Despite these limitations, ARVC risk scores have the potential to improve the accuracy of ARVC diagnosis and risk stratification and to guide clinical practice in the management of ARVC.
Availability of data materials
Data available in Table 1.
References
Aquaro GD, De Luca A, Cappelletto C, Raimondi F, Bianco F, Botto N, Barison A, Romani S, Lesizza P, Fabris E, Todiere G, Grigoratos C, Pingitore A, Stolfo D, Dal Ferro M, Merlo M, Di Bella G, Sinagra G. Comparison of different prediction models for the indication of implanted cardioverter defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy. ESC Heart Fail. 2020;7(6):4080–8. https://doi.org/10.1002/ehf2.13019.
Aquaro GD, De Luca A, Cappelletto C, Raimondi F, Bianco F, Botto N, Lesizza P, Grigoratos C, Minati M, Dell’Omodarme M, Pingitore A, Stolfo D, Ferro MD, Merlo M, Di Bella G, Sinagra G. Prognostic value of magnetic resonance phenotype in patients with arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2020;75(22):2753–65. https://doi.org/10.1016/j.jacc.2020.04.023.
Gasperetti A, Dello Russo A, Busana M, Dessanai M, Pizzamiglio F, Saguner AM, Te Riele ASJM, Sommariva E, Vettor G, Bosman L, Duru F, Zeppilli P, Di Biase L, Natale A, Tondo C, Casella M. Novel risk calculator performance in athletes with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2020;17(8):1251–9. https://doi.org/10.1016/j.hrthm.2020.03.007.
Baudinaud P, Laredo M, Badenco N, Rouanet S, Waintraub X, Duthoit G, Hidden-Lucet F, Redheuil A, Maupain C, Gandjbakhch E. External validation of a risk prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. Can J Cardiol. 2021;37(8):1263–6. https://doi.org/10.1016/j.cjca.2021.02.018.
Carrick RT, Te Riele ASJM, Gasperetti A, Bosman L, Muller SA, Pendleton C, Tichnell C, Murray B, Yap SC, van den Berg MP, Wilde A, Zeppenfeld K, Hays A, Zimmerman SL, Tandri H, Cadrin-Tourigny J, van Tintelen P, Calkins H, James CA, Wu KC. Longitudinal prediction of ventricular arrhythmic risk in patients with arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2022;15(11):e011207. https://doi.org/10.1161/CIRCEP.122.011207.
Casella M, Gasperetti A, Gaetano F, Busana M, Sommariva E, Catto V, Sicuso R, Rizzo S, Conte E, Mushtaq S, Andreini D, Di Biase L, Carbucicchio C, Natale A, Basso C, Tondo C, Dello Russo A. Long-term follow-up analysis of a highly characterized arrhythmogenic cardiomyopathy cohort with classical and non-classical phenotypes-a real-world assessment of a novel prediction model: does the subtypy matter. Europace. 2020;22(5):797–805. https://doi.org/10.1093/europace/euz352.
Jordà P, Bosman LP, Gasperetti A, Mazzanti A, Gourraud JB, Davies B, Frederiksen TC, Weidmann ZM, Di Marco A, Roberts JD, MacIntyre C, Seifer C, Delinière A, Alqarawi W, Kukavica D, Minois D, Trancuccio A, Arnaud M, Targetti M, Martino A, Oliviero G, Pipilas DC, Carbucicchio C, Compagnucci P, Dello Russo A, Olivotto I, Calò L, Lubitz SA, Cutler MJ, Chevalier P, Arbelo E, Priori SG, Healey JS, Calkins H, Casella M, Jensen HK, Tondo C, Tadros R, James CA, Krahn AD, Cadrin-Tourigny J. Arrhythmic risk prediction in arrhythmogenic right ventricular cardiomyopathy: external validation of the arrhythmogenic right ventricular cardiomyopathy risk calculator. Eur Heart J. 2022;43(32):3041–52. https://doi.org/10.1093/eurheartj/ehac289.
Protonotarios A, Bariani R, Cappelletto C, Pavlou M, García-García A, Cipriani A, Protonotarios I, Rivas A, Wittenberg R, Graziosi M, Xylouri Z, Larrañaga-Moreira JM, de Luca A, Celeghin R, Pilichou K, Bakalakos A, Lopes LR, Savvatis K, Stolfo D, Dal Ferro M, Merlo M, Basso C, Freire JL, Rodriguez-Palomares JF, Kubo T, Ripoll-Vera T, Barriales-Villa R, Antoniades L, Mogensen J, Garcia-Pavia P, Wahbi K, Biagini E, Anastasakis A, Tsatsopoulou A, Zorio E, Gimeno JR, Garcia-Pinilla JM, Syrris P, Sinagra G, Bauce B, Elliott PM. Importance of genotype for risk stratification in arrhythmogenic right ventricular cardiomyopathy using the 2019 ARVC risk calculator. Eur Heart J. 2022;43(32):3053–67. https://doi.org/10.1093/eurheartj/ehac235.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71. https://doi.org/10.1136/bmj.n71.
Cadrin-Tourigny J, Bosman LP, Nozza A, Wang W, Tadros R, Bhonsale A, Bourfiss M, Fortier A, Lie ØH, Saguner AM, Svensson A, Andorin A, Tichnell C, Murray B, Zeppenfeld K, van den Berg MP, Asselbergs FW, Wilde AAM, Krahn AD, Talajic M, Rivard L, Chelko S, Zimmerman SL, Kamel IR, Crosson JE, Judge DP, Yap SC, van der Heijden JF, Tandri H, Jongbloed JDH, Guertin MC, van Tintelen JP, Platonov PG, Duru F, Haugaa KH, Khairy P, Hauer RNW, Calkins H, Te Riele ASJM, James CA. A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. Eur Heart J. 2019;40(23):1850–8. https://doi.org/10.1093/eurheartj/ehz103.
Wang Y, Fang Y, Zhang D, Li Y, Luo S. A rare case of arrhythmogenic right ventricular cardiomyopathy associated with LAMA2 mutation: a case report and literature review. Front Med (Lausanne). 2022;18(9):922347. https://doi.org/10.3389/fmed.2022.922347.
Haugaa KH, Haland TF, Leren IS, Saberniak J, Edvardsen T. Arrhythmogenic right ventricular cardiomyopathy, clinical manifestations, and diagnosis. Europace. 2016;18(7):965–72. https://doi.org/10.1093/europace/euv340.
Gemayel C, Pelliccia A, Thompson PD. Arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2001;38(7):1773–81. https://doi.org/10.1016/s0735-1097(01)01654-0.
Bosman LP, Cadrin-Tourigny J, Bourfiss M, Aliyari Ghasabeh M, Sharma A, Tichnell C, Roudijk RW, Murray B, Tandri H, Khairy P, Kamel IR, Zimmerman SL, Reitsma JB, Asselbergs FW, van Tintelen JP, van der Heijden JF, Hauer RNW, Calkins H, James CA, Te Riele ASJM. Diagnosing arrhythmogenic right ventricular cardiomyopathy by 2010 Task Force Criteria: clinical performance and simplified practical implementation. Europace. 2020;22(5):787–96. https://doi.org/10.1093/europace/euaa039.
Femia G, Semsarian C, McGuire M, Sy RW, Puranik R. Long term CMR follow up of patients with right ventricular abnormality and clinically suspected arrhythmogenic right ventricular cardiomyopathy (ARVC). J Cardiovasc Magn Reson. 2019;21(1):76. https://doi.org/10.1186/s12968-019-0581-0.
Iyer VR, Chin AJ. Arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D). Am J Med Genet C Semin Med Genet. 2013;163C(3):185–97. https://doi.org/10.1002/ajmg.c.31368.
Leren IS, Saberniak J, Haland TF, Edvardsen T, Haugaa KH. Combination of ECG and echocardiography for identification of arrhythmic events in early ARVC. JACC Cardiovasc Imaging. 2017;10(5):503–13. https://doi.org/10.1016/j.jcmg.2016.06.011.
Oomen AWGJ, Semsarian C, Puranik R, Sy RW. Diagnosis of arrhythmogenic right ventricular cardiomyopathy: progress and pitfalls. Heart Lung Circ. 2018;27(11):1310–7. https://doi.org/10.1016/j.hlc.2018.03.023.
Fan X, Yang G, Duru F, Grilli M, Akin I, Zhou X, Saguner AM, Ei-Battrawy I. Arrhythmogenic cardiomyopathy: from preclinical models to genotype-phenotype correlation and pathophysiology. Stem Cell Rev Rep. 2023. https://doi.org/10.1007/s12015-023-10615-0.
Ohno S. The genetic background of arrhythmogenic right ventricular cardiomyopathy. J Arrhythm. 2016;32(5):398–403. https://doi.org/10.1016/j.joa.2016.01.006.
Marcus FI, Edson S, Towbin JA. Genetics of arrhythmogenic right ventricular cardiomyopathy: a practical guide for physicians. J Am Coll Cardiol. 2013;61(19):1945–8. https://doi.org/10.1016/j.jacc.2013.01.073.
Paul M, Schulze-Bahr E, Breithardt G, Wichter T. Genetics of arrhythmogenic right ventricular cardiomyopathy–status quo and future perspectives. Z Kardiol. 2003;92(2):128–36. https://doi.org/10.1007/s00392-003-0892-9.
James CA, Jongbloed JDH, Hershberger RE, Morales A, Judge DP, Syrris P, Pilichou K, Domingo AM, Murray B, Cadrin-Tourigny J, Lekanne Deprez R, Celeghin R, Protonotarios A, Asatryan B, Brown E, Jordan E, McGlaughon J, Thaxton C, Kurtz CL, van Tintelen JP. International evidence based reappraisal of genes associated with arrhythmogenic right ventricular cardiomyopathy using the clinical genome resource framework. Circ Genom Precis Med. 2021;14(3):e003273. https://doi.org/10.1161/CIRCGEN.120.003273.
Lombardi R, Marian AJ. Molecular genetics and pathogenesis of arrhythmogenic right ventricular cardiomyopathy: a disease of cardiac stem cells. Pediatr Cardiol. 2011;32(3):360–5. https://doi.org/10.1007/s00246-011-9890-2.
Krahn AD, Wilde AAM, Calkins H, La Gerche A, Cadrin-Tourigny J, Roberts JD, Han HC. Arrhythmogenic Right Ventricular Cardiomyopathy. JACC Clin Electrophysiol. 2022;8(4):533–53. https://doi.org/10.1016/j.jacep.2021.12.002.
Etchegary H, Enright G, Audas R, Pullman D, Young TL, Hodgkinson K. Perceived economic burden associated with an inherited cardiac condition: a qualitative inquiry with families affected by arrhythmogenic right ventricular cardiomyopathy. Genet Med. 2016;18(6):584–92. https://doi.org/10.1038/gim.2015.132.
Kowalik E, Włodarska EK, Woźniak O, Hoffman P. Economic evaluation of screening for familiar form of arrhythmogenic right ventricular cardiomyopathy in Poland. Kardiol Pol. 2007;65(12):1442–6.
Sen-Chowdhry S, Syrris P, McKenna WJ. Role of genetic analysis in the management of patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2007;50(19):1813–21. https://doi.org/10.1016/j.jacc.2007.08.008.
Te Rijdt WP, Jongbloed JD, de Boer RA, Thiene G, Basso C, van den Berg MP, van Tintelen JP. Clinical utility gene card for: arrhythmogenic right ventricular cardiomyopathy (ARVC). Eur J Hum Genet. 2014;22(2):293. https://doi.org/10.1038/ejhg.2013.124.
Malik N, Mukherjee M, Wu KC, Zimmerman SL, Zhan J, Calkins H, James CA, Gilotra NA, Sheikh FH, Tandri H, Kutty S, Hays AG. Multimodality imaging in arrhythmogenic right ventricular cardiomyopathy. Circ Cardiovasc Imaging. 2022;15(2):e013725. https://doi.org/10.1161/CIRCIMAGING.121.013725.
Gandjbakhch E, Redheuil A, Pousset F, Charron P, Frank R. Clinical diagnosis, imaging, and genetics of arrhythmogenic right ventricular cardiomyopathy/dysplasia: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72(7):784–804. https://doi.org/10.1016/j.jacc.2018.05.065.
Borgquist R, Haugaa KH, Gilljam T, Bundgaard H, Hansen J, Eschen O, Jensen HK, Holst AG, Edvardsen T, Svendsen JH, Platonov PG. The diagnostic performance of imaging methods in ARVC using the 2010 Task Force criteria. Eur Heart J Cardiovasc Imaging. 2014;15(11):1219–25. https://doi.org/10.1093/ehjci/jeu109.
Conen D, Osswald S, Cron TA, Linka A, Bremerich J, Keller DI, Pfisterer ME, Buser PT. Value of repeated cardiac magnetic resonance imaging in patients with suspected arrhythmogenic right ventricular cardiomyopathy. J Cardiovasc Magn Reson. 2006;8(2):361–6. https://doi.org/10.1080/10976640500527082.
Marra MP, Leoni L, Bauce B, Corbetti F, Zorzi A, Migliore F, Silvano M, Rigato I, Tona F, Tarantini G, Cacciavillani L, Basso C, Buja G, Thiene G, Iliceto S, Corrado D. Imaging study of ventricular scar in arrhythmogenic right ventricular cardiomyopathy: comparison of 3D standard electroanatomical voltage mapping and contrast-enhanced cardiac magnetic resonance. Circ Arrhythm Electrophysiol. 2012;5(1):91–100. https://doi.org/10.1161/CIRCEP.111.964635.
Inciardi RM. Usefulness of strain imaging echocardiography in arrhythmogenic right ventricular cardiomyopathy: clinical perspective. Int J Cardiovasc Imaging. 2019. https://doi.org/10.1007/s10554-019-01706-6.
Mast TP, Taha K, Cramer MJ, Lumens J, van der Heijden JF, Bouma BJ, van den Berg MP, Asselbergs FW, Doevendans PA, Teske AJ. The prognostic value of right ventricular deformation imaging in early arrhythmogenic right ventricular cardiomyopathy. JACC Cardiovasc Imaging. 2019;12(3):446–55. https://doi.org/10.1016/j.jcmg.2018.01.012.
Campuzano O, Alcalde M, Berne P, Castro V, Guzzo G, Iglesias A, Alonso-Pulpon L, Garcia-Pavia P, Brugada J, Brugada R. Genetic testing of candidate genes in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Eur J Med Genet. 2012;55(4):225–34. https://doi.org/10.1016/j.ejmg.2012.02.007.
de Brouwer R, Bosman LP, Gripenstedt S, Wilde AAM, van den Berg MP, Peter van Tintelen J, de Boer RA, Te Riele ASJM, Netherlands ACM Registry. Value of genetic testing in the diagnosis and risk stratification of arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2022;19(10):1659–1665. https://doi.org/10.1016/j.hrthm.2022.05.038
Hall CL, Sutanto H, Dalageorgou C, McKenna WJ, Syrris P, Futema M. Frequency of genetic variants associated with arrhythmogenic right ventricular cardiomyopathy in the genome aggregation database. Eur J Hum Genet. 2018;26(9):1312–8. https://doi.org/10.1038/s41431-018-0169-4.
Corrado D, Wichter T, Link MS, Hauer RN, Marchlinski FE, Anastasakis A, Bauce B, Basso C, Brunckhorst C, Tsatsopoulou A, Tandri H, Paul M, Schmied C, Pelliccia A, Duru F, Protonotarios N, Estes NM 3rd, McKenna WJ, Thiene G, Marcus FI, Calkins H. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Circulation. 2015;132(5):441–53. https://doi.org/10.1161/CIRCULATIONAHA.115.017944.
Shah SN, Umapathi KK, Oliver TI. Arrhythmogenic Right Ventricular Cardiomyopathy. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470378/
Wichter T, Paul TM, Eckardt L, Gerdes P, Kirchhof P, Böcker D, Breithardt G. Arrhythmogenic right ventricular cardiomyopathy. Antiarrhythmic drugs, catheter ablation, or ICD? Herz. 2005;30(2):91–101. https://doi.org/10.1007/s00059-005-2677-6.
Migliore F, Zorzi A, Silvano M, Rigato I, Basso C, Thiene G, Corrado D. Clinical management of arrhythmogenic right ventricular cardiomyopathy: an update. Curr Pharm Des. 2010;16(26):2918–28. https://doi.org/10.2174/138161210793176491.
Silvano M, Mastella G, Zorzi A, Migliore F, Pilichou K, Bauce B, Rigato I, Perazzolo Marra M, Iliceto S, Thiene G, Basso C, Corrado D. Management of arrhythmogenic right ventricular cardiomyopathy. Minerva Med. 2016;107(4):194–216.
Corrado D, Buja G, Basso C, Thiene G. Clinical diagnosis and management strategies in arrhythmogenic right ventricular cardiomyopathy. J Electrocardiol. 2000;33:49–55. https://doi.org/10.1054/jclc.2000.20323.
Haugaa KH, Bundgaard H, Edvardsen T, Eschen O, Gilljam T, Hansen J, Jensen HK, Platonov PG, Svensson A, Svendsen JH. Management of patients with arrhythmogenic right ventricular cardiomyopathy in the nordic countries. Scand Cardiovasc J. 2015;49(6):299–307. https://doi.org/10.3109/14017431.2015.1086017.
Wang SS, Zhang ZW, Xu YM, Jiang QP, Li H, Qian MY, Li YF. Diagnosis and treatment of arrhythmogenic right ventricular cardiomyopathy in children. Zhongguo Dang Dai Er Ke Za Zhi. 2010;12(3):165–8.
Al-Aidarous S, Protonotarios A, Elliott PM, Lambiase PD. Management of arrhythmogenic right ventricular cardiomyopathy. Heart. 2023. https://doi.org/10.1136/heartjnl-2023-322612.
Schinkel AF. Implantable cardioverter defibrillators in arrhythmogenic right ventricular dysplasia/cardiomyopathy: patient outcomes, incidence of appropriate and inappropriate interventions, and complications. Circ Arrhythm Electrophysiol. 2013;6(3):562–8. https://doi.org/10.1161/CIRCEP.113.000392.
Sharma A, Assis F, James CA, Murray B, Tichnell C, Tandri H, Calkins H. Misdiagnosis of ARVC leading to inappropriate ICD implant and subsequent ICD removal—lessons learned. J Cardiovasc Electrophysiol. 2019;30(10):2020–6. https://doi.org/10.1111/jce.14088.
Migliore F, Viani S, Bongiorni MG, Zorzi A, Silvetti MS, Francia P, D’Onofrio A, De Franceschi P, Sala S, Donzelli S, Ricciardi G, Menardi E, Giammaria M, La Greca C, Bauce B, Rigato I, Iliceto S, Bertaglia E, Diemberger I, Corrado D. Subcutaneous implantable cardioverter defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy: Results from an Italian multicenter registry. Int J Cardiol. 2019;1(280):74–9. https://doi.org/10.1016/j.ijcard.2019.01.041.
Laredo M, Oliveira Da Silva L, Extramiana F, Lellouche N, Varlet É, Amet D, Algalarrondo V, Waintraub X, Duthoit G, Badenco N, Maupain C, Hidden-Lucet F, Maury P, Gandjbakhch E. GPUR Groupe Parisien Universitaire en Rythmologie Investigators. Catheter ablation of electrical storm in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2020;17(1):41–8. https://doi.org/10.1016/j.hrthm.2019.06.022.
Liang E, Wu L, Fan S, Hu F, Zheng L, Liu S, Fan X, Chen G, Ding L, Niu G, Yao Y. Catheter ablation of arrhythmogenic right ventricular cardiomyopathy ventricular tachycardia: 18-year experience in 284 patients. Europace. 2020;22(5):806–12. https://doi.org/10.1093/europace/euaa046.
Romero J, Grushko M, Briceño DF, Natale A, Di Biase L. Radiofrequency ablation in arrhythmogenic right ventricular cardiomyopathy (ARVC). Curr Cardiol Rep. 2017;19(9):82. https://doi.org/10.1007/s11886-017-0893-3.
Gasperetti A, Tandri H. Catheter ablation of ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy. Card Electrophysiol Clin. 2022;14(4):679–83. https://doi.org/10.1016/j.ccep.2022.08.004.
Gasperetti A, James CA, Chen L, Schenker N, Casella M, Kany S, Mathew S, Compagnucci P, Müssigbrodt A, Jensen HK, Svensson A, Costa S, Forleo GB, Platonov PG, Tondo C, Song JP, Dello Russo A, Ruschitzka F, Brunckhorst C, Calkins H, Duru F, Saguner AM. Efficacy of catheter ablation for atrial arrhythmias in patients with arrhythmogenic right ventricular cardiomyopathy-A multicenter study. J Clin Med. 2021;10(21):4962. https://doi.org/10.3390/jcm10214962.
Santangeli P, Zado ES, Supple GE, Haqqani HM, Garcia FC, Tschabrunn CM, Callans DJ, Lin D, Dixit S, Hutchinson MD, Riley MP, Marchlinski FE. Long-term outcome with catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2015;8(6):1413–21. https://doi.org/10.1161/CIRCEP.115.003562.
Acknowledgements
None
Funding
The authors received no specific funding for this manuscript.
Author information
Authors and Affiliations
Contributions
Concept AM, JM, SR. Methodology RP, SR, HARK. Validation SN, MUG. Lit search SR, RP, SR, HARK. First draft SR, RP, SR, HARK, SN, Final draft MUG, JB, JM, AM.
Corresponding author
Ethics declarations
Ethics approval and Consent to participate
Not applicable.
Consent for publication
Yes.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
. Study quality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rashid, S., Pahwani, R., Raj, S. et al. Validation of arrhythmogenic right ventricular cardiomyopathy risk calculator for sudden cardiac death: a systematic review. Int J Arrhythm 24, 25 (2023). https://doi.org/10.1186/s42444-023-00107-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-023-00107-0