Abstract
Background
The prognostic significance of resting heart rate and its therapeutic target in atrial fibrillation (AF) is uncertain. We sought to investigate the relationship between resting heart rate and cardiovascular outcomes in patients with non-paroxysmal AF (non-PAF).
Methods
In this propensity score-weighted, multi-center prospective cohort study, 3217 patients with non-PAF were analyzed. Patients were categorized according to the baseline resting heart rate and cardiovascular outcomes were accessed for a median follow-up of 30 months. The primary outcome was a composite of cardiovascular death, heart failure hospitalization, and myocardial infarction/critical limb ischemia.
Results
Freedom from primary outcome was longest among patients with resting heart rate 80–99 beats per minute (bpm) whereas shortest among those with ≤ 59 bpm (weighted log rank, p = 0.008). Compared with heart rate ≥ 100 bpm, resting heart rate 80–99 and 60–79 bpm was associated with reduced risk of primary outcome (weighted hazard ratio [WHR] 0.52, 95% confidence interval [CI] 0.32–0.84, p = 0.008 and WHR 0.58, 95% CI 0.37–0.92, p = 0.021 for heart rate 80–99 and 60–79 bpm, respectively). Using weighted restricted cubic spline curves, there was a U-shaped association between the resting heart rate and primary outcome with reduced risk of primary outcome in heart rate range of 68–99 bpm. This association was maintained regardless of atrioventricular node (AVN) blocker use or persistent/permanent AF (p for interaction 0.767 for AVN blocker use and 0.720 for AF type).
Conclusion
Resting heart rate was associated with cardiovascular outcomes in patients with non-PAF and those with resting heart rate between 68 and 99 bpm had lower risk of adverse cardiovascular events regardless of AVN blocker use or persistent/permanent AF.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is associated with stroke, myocardial infarction, heart failure (HF), and cardiovascular death [1,2,3,4]. AF is increasingly prevalent with increasing longevity and is associated with significant morbidity and mortality. Because previous studies failed to show improved prognosis with rhythm control [5,6,7,8,9], rate control has become the cornerstone of AF therapy. Rate control has been attempted as background therapy in nearly all patients with AF and is crucial in patients already on rhythm control as well because controlled rate should be maintained during relapses of AF [10]. Theoretically, rapid ventricular rate in patients with AF is believed to have a role in the development or worsening of HF due to loss of atrial contraction, reduced ventricular filling and stroke volume [10, 11]. Although there were reasons to expect improved prognosis under strict rate control, the RACE-II (Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II) trial demonstrated no significant difference in cardiovascular outcomes between patients with strict rate control (< 80 beats per minute [bpm]) versus lenient rate control (< 110 bpm) [12]. Because of the non-inferiority of lenient rate control compared to strict rate control, professional guidelines [2] now recommend a heart rate target of < 110 bpm. However, along with still existing theoretical concerns of lenient rate control, clinicians make varying decisions given the broad range of guideline heart rate target recommendation. Our study sought to investigate the therapeutic target for resting heart rate in patients with non-paroxysmal AF (non-PAF) and its association with cardiovascular outcomes.
Methods
Data source and study population
The COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) registry is an ongoing prospective observational registry at 18 tertiary hospitals from all geographical regions of Republic of Korea. Detailed descriptions are available in previous studies [13]. In brief, the aim of the CODE-AF registry is to assess the clinical epidemiology of patients with AF and to determine the diagnostic and therapeutic processes applied to these patients, along with their clinical outcomes. All patients provided written informed consent. The registry was designed by the Korea Heart Rhythm Society, approved by the ethics committee of each center (4-2016-0105), and registered at ClinicalTrials.gov (NCT02786095).
A total of 11,527 non-valvular AF patients who sought treatment between June 2016 and July 2020 were enrolled. Eligible patients of the registry were > 18 years old with AF and patients without transient AF with reversible causes, or need for chronic anticoagulation to treat conditions other than AF, such as valve prosthesis, deep venous thrombosis (DVT), and pulmonary thromboembolism (PE). After enrollment, each patient was scheduled to be followed up every 6 months either by out-patient clinic visit or telephone contact. Each patient was accessed at enrollment regarding demographics, detailed medical history, and laboratory measures. Resting heart rate and heart rhythm were obtained at baseline from a 12-lead electrocardiogram (ECG), measured after five minutes of rest in the supine position. AF diagnosis was classified as persistent or permanent AF. HF diagnosis was based on medical history or clinical judgment along with laboratory and echocardiographic findings. Patients with body mass index (BMI) > 25 kg/m2 were considered obese according to Asian guideline on definition of obesity [14].
In this study, we included non-PAF patients whose baseline ECG were identified as AF or atrial flutter at the time acquisition. Patients without an out-patient clinic visit or telephone contact for more than 365 days, missing baseline medical data, who were paced permanently were excluded from our study sample. Finally, a total of 3217 non-PAF patients were included and categorized into the following groups according to baseline resting heart rate: ≥ 100 bpm, 80–99 bpm, 60–79 bpm, and ≤ 59 bpm.
Outcome definition and follow-up
The primary outcome was a composite of cardiovascular death, HF hospitalization, and myocardial infarction/critical limb ischemia (CLI). The secondary outcomes were the individual components of the primary outcome. HF hospitalization included hospital admission due to new onset or worsening signs and symptoms of HF irrespective of LVEF. Myocardial infarction was defined as clinical evidence of myocardial ischemia with myocardial necrosis from laboratory findings. Critical limb ischemia (CLI) was defined as presence of ischemic resting pain, ulcer, or gangrene with lower extremity peripheral artery disease. Patients were followed up until the study outcome occurred, censoring, the end of the study period, or death.
Study design and statistical analysis
To make an unbiased comparison between the resting heart rate groups, we used an inverse probability of treatment weight (IPTW) approach. The propensity score, which is the probability of receiving treatment, was estimated using a multinomial logistic regression based on sociodemographic factors, medical history and medication use (variables in Table 1). We examined the balance across the resting heart rate groups using the absolute standardized differences of all covariates with a threshold of 0.1, above which to indicate imbalance. The weights were truncated at the 1st and 99th percentiles to avoid extreme weights. The baseline characteristics of the study population were compared as counts and percentages for categorical variables and medians with 25th and 75th percentiles for continuous variables across the resting heart rate groups. The time to event was calculated as months from the date of entry into the CODE-AF registry to the date of first occurrence of primary outcome.
We assessed the freedom from primary and secondary outcomes by performing an IPTW-weighted Kaplan Meier analysis and compared the difference among the resting heart rate groups with a weighted log rank test. We conducted IPTW-weighted Cox regression analysis to assess the association between resting heart rate groups and primary and secondary outcomes and calculated the weighted hazard ratios (WHR) and 95% confidence intervals (95% CI) using heart rate ≥ 100 bpm as the reference category. In addition, for the graphic assessment of the effects of resting heart rate as a continuous variable, IPTW-weighted restricted cubic spline curves were presented and three knots were located at the 10th, 50th, and 90th percentiles of resting heart rate range.
All analyses were performed using R statistics, version 4.0.2 (R Foundation for Statistical Computing), and a two-sided p value < 0.05 was considered statistically significant.
Subgroup analysis
To assess potential interaction of baseline covariates on the association between resting heart rate and adverse cardiovascular events, we performed subgroup analyses for the primary outcome stratified by AF type (either persistent or permanent AF), sex, age, hypertension, diabetes, obesity, atrioventricular nodal (AVN) blocker use, and anti-arrhythmic drug (AAD) use. AVN blockers included beta-blockers, non-dihydropyridine calcium-channel blockers, and digoxin. AADs included flecainide, propafenone, sotalol, dronedarone, or amiodarone.
Results
Study population
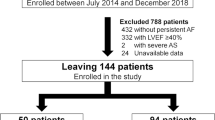
The baseline characteristics of the study population are presented in Table 1. Among the 3,217 non-PAF patients, 8.9% (n = 286) had resting heart rate of ≤ 59 bpm, 42.9% (n = 1379) had 60–79 bpm, 37.1% (n = 1194) had 80–99 bpm, and 11.1% (n = 358) had ≥ 100 bpm. Patients with baseline resting heart rate ≥ 100 bpm were more likely to be female, have a history of diabetes or HF, and prescribed with AVN blockers whereas less likely to have a history of stroke or PAOD, and prescribed with AADs. In contrast, age, CHA2DSc-VASc score and HAS-BLED score were similar across the resting heart rate groups (Table 1). After the IPTW, the baseline characteristics were well balanced across the resting heart rate groups (Additional file 1: Table S1).
Clinical outcomes
The IPTW-weighted Kaplan Meier analyses for the resting heart rate groups are presented in Fig. 1. Resting heart rate 80–99 bpm was associated with longest whereas ≤ 59 bpm with shortest survival free of primary outcomes (IPTW-weighted log rank, p = 0.008). Compared with heart rate ≥ 100 bpm, resting heart rate 80–99 (IPTW-weighted log rank, p = 0.01) and 60–79 bpm (IPTW-weighted log rank, p = 0.027) was associated with reduced risk of primary outcome whereas resting heart rate ≤ 59 bpm was not (IPTW-weighted log rank, p = 0.998).
IPTW-weighted freedom from adverse cardiovascular events according to resting heart rate. Composite outcome included myocardial infarction/CLI, heart failure hospitalization, cardiovascular death. CI confidence interval, CLI critical limb ischemia, HR hazard ratio. Other abbreviations are the same as in Table 1
The IPTW-weighted event rate (ER) and hazard ratios (HRs) of the primary and secondary outcomes according to resting heart rate groups are presented in Table 2. During a median follow-up of 30 months, IPTW-weighted ER of primary outcome was highest in those with heart rate ≥ 100 bpm and lowest in those with heart rate 80–99 bpm (IPTW weighted ER 37.8 and 19.4, respectively). This tendency was consistently found in a separate analysis for HF hospitalization whereas the IPTW-weighted ER for cardiovascular death was lowest in the 60–79 bpm heart rate group. In the IPTW-weighted Cox regression analysis, both 80–99 bpm and 60–79 bpm heart rate groups showed a reduced risk of primary outcome compared with ≥ 100 bpm heart rate group, and risk reduction was more significant in those with heart rate between 80 and 99 bpm (IPTW-weighted HR 0.52, 95% CI 0.32–0.84, p = 0.008 for 80–99 bpm versus IPTW-weighted HR 0.58, 95% CI 0.37–0.92, p = 0.021 for 60–79 bpm) (Table 2). This tendency was maintained in a separate analysis for HF hospitalization (IPTW-weighted HR 0.51, 95% CI 0.28–0.94, p = 0.029 for the 80–99 bpm heart rate group versus IPTW-weighted HR 0.64, 95% CI 0.36–1.12, p = 0.119 for the 60–79 bpm heart rate group) whereas not maintained for myocardial infarction/CLI or cardiovascular death.
In the IPTW-weighted restricted cubic spline curves using resting heart rate 100 bpm as the reference, resting heart rate > 100 bpm and < 56 bpm was associated with increased whereas 68–99 bpm was associated with reduced risk of primary outcome. Similar trend was identified for HF hospitalization and cardiovascular death whereas resting heart rate had no prognostic significance for myocardial infarction/CLI (Fig. 2).
IPTW-weighted restricted cubic spline curves for the composite outcome using resting heart rate 100 bpm as the reference. Composite outcome included myocardial infarction/CLI, heart failure hospitalization, cardiovascular death. CI confidence interval, CLI critical limb ischemia, HR hazard ratio. Other abbreviations are the same as Table 1
Subgroup analysis
The risk of primary outcome according to resting heart rate stratified by AF type, sex, age, hypertension, diabetes, obesity, AVN blocker use, and AAD use is presented in Table 3. The association between resting heart rate and primary outcome was consistent with the main analysis regardless of AF type, sex, age, hypertension, diabetes, obesity, and AVN blocker use. However, significant interaction with AAD use was identified (p for interaction 0.039). Among patients with AADs, the risk of primary outcome tended to increase as resting heart rate decreased. Among patients without AADs, the association between resting heart rate and primary outcome was similar to the main analysis.
Discussion
Main findings
In this prospective AF registry, we investigated the association between resting heart rate and cardiovascular outcomes in patients with non-PAF. We found that resting heart rate 68–99 bpm was associated with reduced whereas > 100 and ≤ 59 bpm was associated with increased risk of adverse cardiovascular events independent of AVN blocker use or AF type (persistent or permanent). Given the broad guideline heart rate target recommendation, the results of this study may provide guidance on rate control strategy in clinical practice among patients with non-PAF.
Heart rate and cardiovascular outcomes
There are scarce data to guide the resting heart rate target in patients with AF. RACE II study [12] showed that lenient rate control (< 110 bpm) is non-inferior to strict rate control (< 80 bpm) in patients with permanent AF and the professional guidelines now recommend a resting heart rate target of < 110 bpm [2, 4]. The upper heart rate target (< 100 bpm) suggested in our study is similar to RACE-II trial (< 110 bpm) considering the heart rate variability in patients with AF. However, this study also suggested that resting heart rate ≥ 100 or ≤ 59 bpm might be associated with increased risk of adverse cardiovascular events. Consistent with our findings, Van Gelder et al. [15] compared the RACE (RAte Control vs. Electrical cardioversion) and AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm Management) study and showed that although there was no favorable trends toward either heart rate target of < 80 bpm or < 100 bpm, both heart rate groups had better clinical outcomes than the ≥ 100 bpm heart rate group.
In terms of lower heart rate target, slow resting heart rate in patients with AF has been reported to be associated with chronotropic incompetence and pacemaker implantation [15, 16]. This implies that AF patients with relatively slow resting heart rate may have underlying autonomic nervous dysfunction or conduction system disorder, which might have translated into loss of clinical benefit among those with heart rate < 68 bpm shown in the spline curves [15, 16]. The lower heart rate target (≥ 68 bpm) suggested in this study have not been traditionally considered slow and may have clinical implications among those already on AVN blockers.
In a hemodynamic point of view, ventricular rate that is either too fast or too slow is detrimental in patients with AF and the therapeutic heart rate target should be the heart rate at which cardiac output is least compromised [10, 17, 18]. Rawles [19] used mathematical models to investigate the net effect of ventricular rate on cardiac output in patients with AF. They suggested that resting ventricular rate around 90 bpm is the heart rate at which cardiac output is least compromised and is line with our study findings. Similarly, a rather fast lower heart rate target (≥ 68 bpm) suggested might be attributable to reduced stroke volume resulting from loss of atrial contraction in AF, and AF patients might require a relatively faster resting heart rate to generate equivalent cardiac output compared with those at sinus rhythm [18, 19].
Subgroup analysis
In this study, the association between resting heart rate and primary outcome was not affected by AF type (persistent vs permanent), age, sex, HTN, DM, obesity, or AVN blocker use. Rate control strategy is a background therapy for nearly all patients with AF [10] and our results may apply to those already on AVN blockers. In contrast, a significant interaction with AADs was identified, and our results suggest that resting heart rate has no prognostic significance among AAD users. The reason is unclear but patients on AADs are more likely to experience multiple episodes of sinus to AF rhythm and vice versa, and the resting heart rate measured in our study might not reflect the average heart rate at which AAD users were at predominantly.
Limitation
There are several limitations in this study. First, despite efforts to make unbiased comparison between the resting heart rate groups using propensity score models, residual confounding may exist due to the observational nature of the study. Second, the resting heart rate measured in this study was a single-time point measure without time dependent updates. Third, the CODE-AF registry used in this study included AF patients from tertiary hospitals and might not represent the general AF patients. Fourth, HF diagnosis was based on clinical assessment and medical history and thus might have been both over and under-diagnosed considering the similarity between HF and AF symptoms. Fifth, the resting heart rate was measured from a single baseline ECG and might not reflect the average resting heart rate throughout the day.
Conclusion
In this prospective AF registry, we found that resting heart rate 68–99 bpm was associated with reduced whereas > 100 and ≤ 59 bpm was associated with increased risk of adverse cardiovascular events regardless of AVN blocker use or AF type. Given the broad guideline heart rate target recommendations, the results of this study may provide guidance on rate control strategy in clinical practice.
Availability of data and materials
The collected data were registered in the internet-based clinical research and trial management system (iCReaT, http://icreat.nih.go.kr); investigators can apply for use of the database.
Abbreviations
- AAD:
-
Anti-arrhythmic drug
- AF:
-
Atrial fibrillation
- AVN:
-
Atrioventricular nodal
- BMI:
-
Body mass index
- bpm:
-
Beats per minute
- CKD:
-
Chronic kidney disease
- CLI:
-
Critical limb ischemia
- DVT:
-
Deep venous thrombosis
- ECG:
-
Electrocardiogram
- OAC:
-
Oral anticoagulant
- PE:
-
Pulmonary thromboembolism
- HF:
-
Heart failure
References
Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120(9):1501–17. https://doi.org/10.1161/CIRCRESAHA.117.309732.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612.
Goto S, Bhatt DL, Rother J, et al. Prevalence, clinical profile, and cardiovascular outcomes of atrial fibrillation patients with atherothrombosis. Am Heart J. 2008;156(5):855-863.e2. https://doi.org/10.1016/j.ahj.2008.06.029.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76. https://doi.org/10.1016/j.jacc.2014.03.022.
Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825–33. https://doi.org/10.1056/NEJMoa021328.
Van Gelder IC, Hagens VE, Bosker HA, et al. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002;347(23):1834–40. https://doi.org/10.1056/NEJMoa021375.
Carlsson J, Miketic S, Windeler J, et al. Randomized trial of rate-control versus rhythm-control in persistent atrial fibrillation: the Strategies of Treatment of Atrial Fibrillation (STAF) study. J Am Coll Cardiol. 2003;41(10):1690–6. https://doi.org/10.1016/s0735-1097(03)00332-2.
Hohnloser SH, Kuck KH, Lilienthal J. Rhythm or rate control in atrial fibrillation–Pharmacological Intervention in Atrial Fibrillation (PIAF): a randomised trial. Lancet. 2000;356(9244):1789–94. https://doi.org/10.1016/s0140-6736(00)03230-x.
Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358(25):2667–77. https://doi.org/10.1056/NEJMoa0708789.
Van Gelder IC, Rienstra M, Crijns HJ, Olshansky B. Rate control in atrial fibrillation. Lancet. 2016;388(10046):818–28. https://doi.org/10.1016/S0140-6736(16)31258-2.
Wyse DG. Therapeutic considerations in applying rate control therapy for atrial fibrillation. J Cardiovasc Pharmacol. 2008;52(1):11–7. https://doi.org/10.1097/FJC.0b013e31816d5f49.
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362(15):1363–73. https://doi.org/10.1056/NEJMoa1001337.
Kim H, Kim TH, Cha MJ, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J. 2017;47(6):877–87. https://doi.org/10.4070/kcj.2017.0146.
Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S. Criteria and classification of obesity in Japan and Asia-Oceania. World Rev Nutr Diet. 2005;94:1–12. https://doi.org/10.1159/000088200.
Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8(11):935–42. https://doi.org/10.1093/europace/eul106.
Corbelli R, Masterson M, Wilkoff BL. Chronotropic response to exercise in patients with atrial fibrillation. Pacing Clin Electrophysiol. 1990;13(2):179–87. https://doi.org/10.1111/j.1540-8159.1990.tb05068.x.
Kerr AJ, Williams MJ, Stewart RA. Ventricular rate and beat-to-beat variation of stroke volume in atrial fibrillation. Am J Cardiol. 2001;87(9):1116-1119.A9. https://doi.org/10.1016/s0002-9149(01)01475-8.
Camm AJ, Savelieva I, Lip GY, Guideline Development Group for the Ncgftmoaf. Rate control in the medical management of atrial fibrillation. Heart. 2007;93(1):35–8. https://doi.org/10.1136/hrt.2006.099903.
Rawles JM. What is meant by a “controlled” ventricular rate in atrial fibrillation? Br Heart J. 1990;63(3):157–61. https://doi.org/10.1136/hrt.63.3.157.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: BJ; Data curation: HJP, HTY; Formal analysis: THK; Funding acquisition: BJ; Investigation: JP; Methodology: JKP; Project administration: KWK, JS; Resources: JBK; Software: JK; Supervision: EKC; Validation: HWP; Visualization: YSL; Writing—original draft: HJP; Writing—review and editing: HTY.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
CODE-AF registry was designed by the Korea Heart Rhythm Society, approved by the ethics committee of each center (4-2016-0105), and registered at ClinicalTrials.gov (NCT02786095). All participants were provided written informed consent.
Consent for publication
All authors agree with publication of the manuscript.
Competing interests
Dr. Boyoung Joung has served as a speaker for Bayer, BMS/Pfizer, Medtronic, and Daiichi-Sankyo and has received research funds from Medtronic and Abbott. All other authors declare no competing interests. No fees were received personally.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Baseline characteristics of the study population by resting heart rate after IPTW.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, H., Yu, H.T., Kim, TH. et al. Resting heart rate and cardiovascular outcomes in patients with non-paroxysmal atrial fibrillation: CODE-AF registry. Int J Arrhythm 24, 15 (2023). https://doi.org/10.1186/s42444-023-00090-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-023-00090-6