Abstract
Background
This study aims to investigate the current status of AF (atrial fibrillation) catheter ablation in Korea.
Methods
The patients who underwent AF catheter ablation from September 2017 to December 2019 were prospectively enrolled from 37 arrhythmia centers. Demographic data, procedural characteristics, the extent of catheter ablation, acute success of the ablation lesion set, rate and independent risk factor for recurrence of AF were analyzed.
Results
A total of 2402 AF patients [paroxysmal AF (PAF) 45.7%, persistent AF (PeAF) 43.1% and redo AF 11.2%] were included. Pulmonary vein isolation (PVI) was performed in 2378 patients (99%) and acute success rate was 97.9%. Additional non-PV ablation (NPVA) were performed in 1648 patients (68.6%). Post-procedural complication rate was 2.2%. One-year AF-free survival rate was 78.6% and the PeAF patients showed poorer survival rate than the ones with other types (PeAF 72.4%, PAF 84.2%, redo AF 80.0%). Additional NPVA did not influence the recurrence of AF in the PAF patients (PVI 17.0% vs. NPVA 14.6%, P value 0.302). However, it showed lower AF recurrence rate in the PeAF patients (PVI 34.9% vs. NPVA 24.4%, P value 0.001). Valvular heart disease, left atrial diameter, PeAF, PVI alone, need of NPVA for terminating AF, and failed ablation were independent predictors of AF recurrence.
Conclusions
Additional NPVA was associated better rhythm outcome in the patients with PeAF, not in the ones with PAF. The independent risk factors for AF recurrence in Korean population were similar to previous studies. Further research is needed to discover optimal AF ablation strategy.
Similar content being viewed by others
Background
Atrial fibrillation (AF) is the most common sustained arrhythmia and causes serious cardiovascular diseases such as stroke and heart failure in the long term. In Korea, the incidence of AF in 2015 was 17.1 per 10,000 persons-year that was gradually increased from 2008, and its prevalence was 0.67% which was 1.7 times higher than that in 2008 [1]. AF-related hospitalization and outpatient clinic visits increased year by year, and consequent healthcare expenditure also continuously increased [2]. The main stems of AF treatment involve avoiding stroke, improving AF-related symptoms, controlling the heart rate or rhythm, and managing cardiovascular risk factors and concomitant diseases [3]. Catheter ablation of AF was effective in suppressing AF symptoms refractory to antiarrhythmic drug treatment, and recurrence of AF was smaller than medical therapy [4]. It has also been shown to improve quality of life and mortality and cardiovascular outcomes such as stroke, bleeding, and heart failure [5,6,7]. In Korea, AF catheter ablation has increased gradually and safely performed [8, 9]. However, there are little data on the current status of AF ablation in Korea. This study aims to establish a prospective AF ablation registry to investigate the current status of AF catheter ablation in Korea.
Methods
Study population
The Korean Heart Rhythm Society Ablation Registry for AF (KARA) is an investigator-initiated, multicenter, prospective registry of catheter ablation for AF. This study was approved by the Institutional Review Board of Seoul National University Hospital and each participating arrhythmia center. Written informed consent was obtained from study subjects. The study subjects were the patients who underwent AF catheter ablation for antiarrhythmic drug (AAD)-refractory symptoms from September 2017 to May 2020 in Korea. Young patients under the age of 19, the patients with cognitive impairments that could not understand informed consent, and the patients who did not consent to participate in the study were excluded from the registration.
Data collection
All data were collected in each practicing center and sent to the core laboratory, Seoul National University Hospital. Baseline data included the patients’ demographics (e.g., age, height, body weight, and sex), procedure date, type of AF, an indication of catheter ablation, cardiovascular comorbidities such as heart failure, hypertension, diabetes mellitus, cerebrovascular accident or arterial thromboembolic event, ischemic heart disease, valvular heart disease, peripheral arterial disease, presence of any cardiomyopathy, chronic kidney disease, obstructive sleep apnea, and history of any cardiac surgery, prescription of oral anticoagulants or antiplatelet agents, left ventricular (LV) ejection fraction (EF), and left atrial (LA) anteroposterior diameter. Procedural data included the number of previous AF ablation(s), an electrocardiographic (ECG) rhythm at the beginning of the procedure, mode of ablation energy, vendor name of three-dimensional mapping system, procedural time, ablation time, fluoroscopic time, ablation lesion and acute result of each ablation lesion. Acute success of each ablation lesion was assessed by each operator and was defined as entrance and/or exit block for pulmonary vein (PV) or superior vena cava (SVC) isolation, bidirectional block by differential pacing for linear ablation, and disappearance of trigger beat from specific anatomical site for focal trigger ablation. If there was no record of confirmation, the lesion set was considered incomplete. Information for acute complications before discharge and their management were also collected.
Follow-up
Mandatory follow-up visits were performed at 3, 6, and 12 months after the procedure. Twelve-lead ECG was performed at each visit. Long-term ECG test, such as Holter or event recorder was not mandatory, and its use was at the operator’s discretion. Additional clinic visits and ECG tests were allowed when the patient became symptomatic or the operator suspected recurrence. At each follow-up visit, cardiovascular outcomes (e.g., ischemic stroke/transient ischemic attack, systemic embolism, aggravation of heart failure, myocardial infarction, and all-cause death), ECG rhythm, and use of AAD were collected. Recurrence of AF was defined as the occurrence of any atrial tachyarrhythmia in 12-lead ECG or lasting more than 30 s in long-term ECG monitoring. The first 90 days from the procedure was regarded as a blanking period, and the recurrence of AF was ignored during this period.
Statistical analysis
Categorical variables were expressed as frequency and percentage. Normally distributed continuous variables were expressed as mean ± standard deviation. The variables that were not normally distributed were expressed as the median [lowest quartile, highest quartile]. The recurrence of AF was compared by the Kruskal–Wallis test and Mann–Whitney test with Bonferroni correction according to the type of AF (paroxysmal, persistent and redoAF). It was also evaluated by Kaplan–Meier survival analysis with the Log-rank test. Cox-proportional hazard model was used to elucidate independent predictors for recurrence of AF. A P value less than 0.05 was considered statistically significant in Kaplan–Meier survival analysis, Cox-proportional regression analysis, and Kruskal–Wallis test for recurrence of AF. In case of intergroup analysis by Mann–Whitney test, P value less than 0.017 was considered significant. All statistical analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA) & R software version 4.0.2 (R foundation for Statistical Computing, Vienna, Austria).
Results
Subject enrollment and baseline characteristics
Between September 2017 and May 2020, 3239 patients with AF who underwent catheter ablation from 37 centers were enrolled in this registry. Among them, 486 patients enrolled in 2020 were excluded in the present analysis because the follow-up duration was < 1 year. Three hundred and fifty-one patients with incomplete follow-up data were also excluded from the analysis. Finally, 2402 patients were included in this analysis (Fig. 1). The mean age was 60.2 ± 9.6 years old, and the male was 73.6% (n = 1767). The proportion of paroxysmal AF was 45.7% (n = 1097) and that of persistent AF and redo ablation were 43.1% (n = 1035) and 11.2% (n = 270), respectively. Hypertension was the most common comorbidities (n = 1218, 50.7%), was followed by diabetes mellitus (n = 434, 18.1%), heart failure (n = 259, 10.8%), and cerebrovascular accident (n = 219, 9.1%). Proportion of the patients with structural heart diseases such as ischemic heart disease, cardiomyopathy, valvular heart disease, and history of cardiac operation were 7.4% (n = 178), 3.9% (n = 93), 3.8% (n = 92), and 2.1% (n = 51), respectively. A number of 2267 patients (94.4%) received oral anticoagulant before the procedure and direct oral anticoagulants were used in most patients (n = 1996, 83.1%). The mean LV EF was 59%, and LA diameter was 43 mm (Table 1). About 90% of the cases were the first-time AF ablation (n = 2132, 88.8%). The proportion of cryoablation was 7.9% (n = 190). Mean procedure time, ablation time, and fluoroscopic time were 197.6 ± 90.2, 57.4 ± 42.0, and 33.8 ± 27.0 min (Table 2).
Acute procedural success rates
A number of 2378 patients received PVI (99.0%) and complete isolation was achieved in 97.9% of the patients. A dormant conduction test was performed on 36.5% of the patients. Additional non-PV ablation (NPVA) were performed in 1648 patients (68.6% of total), mostly atrial linear ablations (n = 1511, 62.9% of total). The most performed lesion was cavotricuspid isthmus (CTI) line (n = 1366, 56.9%), followed by LA roof line (n = 338, 14.1%), mitral isthmus line (n = 205, 8.5%), linear ablation between both inferior PVs (inferior line) (n = 142, 5.9%), superior vena cava (SVC)—interatrial septal (IAS) line (n = 149, 6.2%), and LA anterior line (n = 97, 4.0%). Non-PV trigger ablation was performed in 405 patients (16.9%). SVC isolation (n = 266, 11.1%), focal ablation on LA appendage (n = 127, 5.3%), and coronary sinus (n = 111, 4.6%) were performed. CTI ablation and SVC isolation showed high acute success rates (97.1% and 91.7%, respectively). Other linear ablations or focal ablations showed modest or low success rates (Table 3). Focal ablation based on complex fractionated atrial electrogram (CFAE) was performed in 254 patients (10.6%). About a half of the patients (n = 1265, 52.7%) were sinus rhythm before the beginning of the procedure. Direct current (DC) cardioversion was performed in 439 patients (18.3%), and 193 patients (8.0%) showed sustained AF at the end of the procedure. After ablation, AF induction test was performed in about 70% of the patients.
Post-procedural complications
Post-procedural complication rate was 2.2% (n = 54). The most common complication was cardiac tamponade (n = 15, 0.6%). Access site complications (n = 11, 0.5%) and pericardial effusion (n = 6, 0.2%) were followed. There was no procedure-related death in this registry (Table 4).
Rhythm control outcome and independent predictors for recurrence of atrial fibrillation
Sixty percent of the patients received any AAD after the blanking period (n = 1442, 60.2%). The patients with persistent AF were prescribed the AADs more frequently compared to the patients with paroxysmal AF and redo AF (68.0%, 54.1%, and 53.7%, respectively; P value < 0.001) (Fig. 2A). Among 2397 patients, freedom from AF at one year was achieved in 1888 patients (78.6%). Those of the patients with paroxysmal, persistent and redo AF were 84.6%, 72.4%, and 80%, respectively (P value < 0.001). In intergroup analysis, the patients with persistent AF showed statistically higher recurrence rate compared to the patients with paroxysmal and redo AF [P value (persistent AF vs. paroxysmal AF) < 0.001; (persistent AF vs. redo AF) 0.012]. The recurrence rates of the patients with paroxysmal AF and redo AF were not statistically different (P value 0.066) (Fig. 2B).
Use of antiarrhythmic drug after blanking period and recurrence rate of AF at 1 year. Use of antiarrhythmic drugs after blanking period (A) and AF recurrence rate at 1 year (B) were more frequent in the patients with persistent AF compared to the ones with paroxysmal AF and redo AF. AAD, antiarrhythmic drug; AF, atrial fibrillation; PAF, paroxysmal AF; PeAF, persistent AF
Kaplan–Meier survival analysis showed that the patients with persistent AF showed worse rhythm outcome compared to other types of AF [Log-rank P value (persistent AF vs. paroxysmal AF) < 0.001; (persistent AF vs. redo AF) 0.010]. There was no statistical difference between the patients with paroxysmal AF and redo AF (P value 0.070) (Fig. 3). There was no statistical difference in recurrence of AF according to ablation strategy (PVI alone vs. PVI and additional NPVA) in the patients with paroxysmal AF (17.0% vs. 14.6%, Log rank P value 0.284). However, the patients with persistent AF who received PVI and additional NPVA showed lower recurrence rate than ones received PVI alone (34.9% vs. 24.4%, Log rank P value 0.001) (Fig. 4).
Kaplan–Meier survival curve for recurrence of atrial tachyarrhythmia after AF catheter ablation. The patients with persistent AF showed the lowest AF free survival compared to the patients with paroxysmal AF and redo AF. There was no statistical difference between the patients with paroxysmal AF and redo AF. AF, atrial fibrillation; PAF, paroxysmal atrial fibrillation; PeAF, persistent atrial fibrillation
Kaplan–Meier survival curve for recurrence of atrial tachyarrhythmia according to the ablation strategies. Pulmonary vein isolation plus additional ablation did not influence the recurrence of AF in the patients with paroxysmal AF (A). However, it affected lower AF recurrence rate in the patients with persistent AF (B). AF, atrial fibrillation; PVI, pulmonary vein isolation
In univariable Cox-proportional analysis, presence of valvular heart disease (HR 2.46, 95% CI 1.780–3.396), LV EF (by 1%) (HR 0.99, 95% CI 0.976–0.995), LA diameter (by 1 mm) (HR 1.06, 95% CI 1.042–1.069), persistent AF (vs. paroxysmal AF) (HR 1.92, 95% CI 1.589–2.324), PVI alone (vs. PVI and additional NPVA) (HR 1.27, 95% CI 1.064–1.526), mode of AF termination (need of NPVA, need of DC cardioversion, and not terminated by any ablation vs. sinus rhythm before the first energy application), [HR 1.83, 95% CI 1.363–2.453; HR 1.77, 95% CI 1.411–2.215; HR 2.82, 95% CI 2.166–3.678] and not performing AF induction test (vs. no AF inducibility) (HR 1.22, 95% CI 1.003–1.486) were associated with the recurrence of AF. In multivariable Cox proportional hazard model, valvular heart disease (HR 1.60, 95% CI 1.139–2.253), LA diameter (HR 1.04, 95% CI 1.024–1.053), persistent AF (HR 1.43, 95% CI 1.152–1.764), PVI alone (HR 1.34, 95% CI 1.104–1.619), need of NPVA for terminating AF (HR 1.56, 95% CI 1.153–2.152) and not terminated by any ablation (HR 1.94, 95% CI 1.460–2.578) were independent predictors of AF recurrence (Table 5).
Discussion
Demographic profiles
This study is a multicenter, prospective registry that enrolled 37 arrhythmia centers in Korea. The demographic profiles of the study population, such as age, gender distribution, and type of AF were comparable to other Korean or foreign studies [8, 10, 11]. Of note, the proportion of heart failure patients is relatively low compared to other studies using the Korean claim database [1, 8]. However, the rate was similar compared to other cohort studies in Korea [12, 13]. NHIS claim data might be over-claimed the heart failure diagnosis related to some drug use and did not have echocardiographic parameters in it. On the other hand, our study had echocardiographic data that could identify the LV dysfunction more correctly.
Sleep apnea is known as a risk factor for AF [3]. The prevalence of sleep apnea in patients with AF was variable in previous studies, ranging from 18 to 49% [14, 15]. However, an awareness of sleep apnea is not widespread in clinical practice, and a diagnostic test is cumbersome. Therefore, the prevalence of sleep apnea might be underestimated in this study.
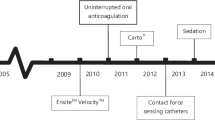
The proportion of cryoablation was small because the cryoablation system has been available since late 2018 in Korea, which was very late compared to other countries.
Procedure patterns
Pulmonary vein isolation is a standard procedure in AF ablation. All patients who underwent de novo AF ablation and the patients with AF recurrence were received PVI in this study. Some patients who did not receive PVI were the redo AF patients without PV reconnection. More than 60% of the procedure did not confirm the presence of the dormant conduction in the present registry. It is thought that controversial results for the effectiveness of elimination of the dormant conduction could affect the current practice pattern [16, 17]. Interestingly, the incidence of dormant conduction was 11% (n = 96/876) that was lower than in other studies [18, 19]. Further evaluations would be needed to clarify it. Additional NPVA were widely performed in this study. The most common lesion set was a CTI linear ablation (n = 1366, 56.9%). Typical atrial flutter often accompanied with AF and the CTI ablation is easy to achieve bidirectional block [20]. The success rate of the CTI ablation was 97.1% that was consistent with other studies [20, 21]. Other LA linear ablations were performed in about 20% of the patients and it was similar to other studies [10, 22]. However, the success rates of LA linear ablations were lower than in a previous paper [23]. We considered the linear ablation was not successful when there was no confirmation of the linear lesion set. Probably, it could make underestimation of the success rate of linear lesion sets in this study. Additional NPVA are often performed in patients with persistent AF and macro-reentrant atrial tachycardia. Still, there is no consensus for the effective ablation strategy for persistent or long-standing persistent AF because previous studies showed controversial results [24, 25]. It is thought that they influenced the utilization of LA linear ablations although the rate of the patients with persistent AF was 43.1% in this study. Non-PV trigger is an important source of AF development but non-PV trigger ablation was not wildly performed in this study. In addition, it was 30% that did not perform AF induction test. In STAR-AF II trial, the authors reported that additional linear ablation or ablation for complex fractionated electrogram (CFAE) did not show the benefit for AF recurrence in the patients with persistent AF [25]. This result is thought to influence the PVI as the initial ablation strategy for persistent AF. Another possible explanation is that it is often difficult to localize the focal trigger source despite support by a 3D mapping system. Also, there is no clear endpoint for focal trigger ablation. The SVC isolation was more frequently performed than other non-PV trigger source ablation, and the success rate was high (91.7%). It is thought that there was a definite anatomical structure and a clear endpoint such as an entrance or exit block. Substrate modifications for CFAE, ganglionated plexus, and focal impulse and rotor mapping were performed in limited numbers. The complexity of the procedures, unclear endpoints, and little evidence for better prognosis could hinder the wide adoption of these technologies.
Rhythm outcome
The rate of AF-free survival at one year was 78.6% that was higher than other studies, although about half of the patients were persistent AF [11, 26]. Long-term ECG monitoring was not mandatory during the follow-up period and it could make less detection of atrial tachyarrhythmias. In addition, the use of AAD after blanking period was at the physician’s discretion in this study. It was different from other clinical trials that strongly discourage the use of AAD after blanking period. Previous studies also reported that the patients with persistent AF showed worse AF-free survival after catheter ablation than the ones with paroxysmal AF and it is consistent with our results [27, 28]. In present study, AF-free survival rate of the patients with redo AF was similar to that of the patients with paroxysmal AF. The rate of maintaining sinus rhythm after multiple procedures was higher than that of de novo ablation [29, 30]. It is thought that recurrence of AF was reduced by performing PV re-isolation, atrial substrate modification or non-PV trigger elimination during redo-ablation. However, it could not be concluded that the aggressive approach to the patients with redo AF is warranted and further randomized trials should be needed to investigate this issue.
Valvular heart disease, LA diameter, persistent AF, PVI alone, and AF termination by non-PV ablation or failed ablation were independent predictors of AF recurrence in this study. Moderate or severe valvular heart diseases and persistent AF are well-known risk factors for AF recurrence after catheter ablation [11]. They cause long-term hemodynamic deterioration, which leads to structural remodeling, and fibrosis of the atrium. Consequently, LA enlargement was developed and it is also a risk factor for AF recurrence after catheter ablation [31]. Our results were consistent with the previous evidence. Interestingly, PVI alone (vs. PVI and additional NPVA) is associated with the increased risk of AF recurrence. There were possible explanations. Impact of additional NPVA on maintaining sinus rhythm after catheter ablation is controversial [25, 32]. However, macro-reentrant AT or non-PV trigger related AF were found in 20–30% of the procedure [33, 34]. In this situation, additional NPVA is needed to restore sinus rhythm. Our result could be thought as a necessity to find and resolve atrial tachyarrhythmias that were not related to PVs. Second, use of the AADs during the follow-up period was more than 60% and that probably affected to the result. Third, the success rate of the linear ablation might be underestimated because we considered the lesion set was incomplete when there was no confirmation of the linear lesion set. Mode of termination was also showed an interesting finding. Termination of AF by PVI had similar prognostic effect compared to sinus rhythm before the first ablation. It could be considered that the PVs were significant AF substrate and other atrial substrates were insufficient to perpetuating AF in both conditions. On the other hand, the fact that AF was terminated by NPVA or failed by any ablation implies that there might be an AF trigger or significant atrial substrates. Meanwhile, there was no difference between the initial sinus rhythm and the termination by cardioversion. It is thought that the timing of DC cardioversion was different for each operator or case.
Limitation
There are several limitations in this study. There was no mandatory recommendation of ablation and follow-up strategy. The definition of acute success may be different depending on the operators. Nonuniform follow-up methodology also influenced collecting recurrence data as asymptomatic or short, intermittent atrial tachyarrhythmia episodes may have been ignored. Second, there was limited data on AF cryoablation. It has been available in Korea since 2018, and it was not widely adopted when the study enrollment was active.
Conclusions
Catheter ablation for AF is an effective and safe treatment modality in Korean real-world practice. Additional NPVA was associated with better rhythm outcome in the patients with persistent AF, not in the ones with paroxysmal AF. Valvular heart disease, persistent AF, PVI alone, need of NPVA for terminating AF, and failed ablation are independent risk factors for AF recurrence after catheter ablation. Those were consistent in the previous studies. Further investigations are needed to discover optimal strategy of catheter ablation for AF.
Availability of data and materials
The data that support the findings of this study are available from Korean Heart Rhythm Society but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Korean Heart Rhythm Society.
References
Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Trends in the incidence and prevalence of atrial fibrillation and estimated thromboembolic risk using the CHA2DS2-VASc score in the entire Korean population. Int J Cardiol. 2017;236:226–31.
Lee H, Kim TH, Baek YS, Uhm JS, Pak HN, Lee MH, et al. The trends of atrial fibrillation-related hospital visit and cost, treatment pattern and mortality in Korea: 10-year nationwide sample cohort data. Korean Circ J. 2017;47(1):56–64.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498.
Raatikainen MJ, Hakalahti A, Uusimaa P, Nielsen JC, Johannessen A, Hindricks G, et al. Radiofrequency catheter ablation maintains its efficacy better than antiarrhythmic medication in patients with paroxysmal atrial fibrillation: on-treatment analysis of the randomized controlled MANTRA-PAF trial. Int J Cardiol. 2015;198:108–14.
Blomstrom-Lundqvist C, Gizurarson S, Schwieler J, Jensen SM, Bergfeldt L, Kenneback G, et al. Effect of catheter ablation vs antiarrhythmic medication on quality of life in patients with atrial fibrillation: the CAPTAF randomized clinical trial. JAMA. 2019;321(11):1059–68.
Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, et al. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA. 2019;321(13):1275–85.
Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA. 2019;321(13):1261–74.
Lee E, Lee SR, Choi EK, Han KD, Cha MJ, Lip GYH, et al. Temporal trends of catheter ablation for patients with atrial fibrillation: a Korean nationwide population-based study. J Cardiovasc Electrophysiol. 2020;31(10):2616–25.
Kim YG, Shim J, Kim DH, Choi JI, Park SW, Pak HN, et al. Characteristics of atrial fibrillation patients suffering atrioesophageal fistula after radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2018;29(10):1343–51.
Park JW, Yu HT, Kim TH, Uhm JS, Kim JY, Joung B, et al. Trends and outcome of catheter ablation of atrial fibrillation over 9 years—focus on empirical extra-pulmonary vein ablation. Circ J. 2019;83(2):304–12.
Sultan A, Luker J, Andresen D, Kuck KH, Hoffmann E, Brachmann J, et al. Predictors of atrial fibrillation recurrence after catheter ablation: data from the German ablation registry. Sci Rep. 2017;7(1):16678.
Kim H, Kim TH, Cha MJ, Lee JM, Park J, Park JK, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) registry. Korean Circ J. 2017;47(6):877–87.
Yu HT, Kim IS, Kim TH, Uhm JS, Kim JY, Joung B, et al. Persistent atrial fibrillation over 3 years is associated with higher recurrence after catheter ablation. J Cardiovasc Electrophysiol. 2020;31(2):457–64.
Holmqvist F, Guan N, Zhu Z, Kowey PR, Allen LA, Fonarow GC, et al. Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation—results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Am Heart J. 2015;169(5):647-54 e2.
Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110(4):364–7.
Macle L, Khairy P, Weerasooriya R, Novak P, Verma A, Willems S, et al. Adenosine-guided pulmonary vein isolation for the treatment of paroxysmal atrial fibrillation: an international, multicentre, randomised superiority trial. Lancet. 2015;386(9994):672–9.
Efremidis M, Letsas KP, Lioni L, Vlachos K, Georgopoulos S, Saplaouras A, et al. Adenosine-guided pulmonary vein antral isolation for paroxysmal atrial fibrillation: a randomized study. J Cardiovasc Electrophysiol. 2016;27(11):1288–92.
Arentz T, Macle L, Kalusche D, Hocini M, Jais P, Shah D, et al. “Dormant” pulmonary vein conduction revealed by adenosine after ostial radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2004;15(9):1041–7.
Tritto M, De Ponti R, Salerno-Uriarte JA, Spadacini G, Marazzi R, Moretti P, et al. Adenosine restores atrio-venous conduction after apparently successful ostial isolation of the pulmonary veins. Eur Heart J. 2004;25(23):2155–63.
Perez FJ, Schubert CM, Parvez B, Pathak V, Ellenbogen KA, Wood MA. Long-term outcomes after catheter ablation of cavo-tricuspid isthmus dependent atrial flutter: a meta-analysis. Circ Arrhythm Electrophysiol. 2009;2(4):393–401.
Kim SH, Oh YS, Choi Y, Hwang Y, Kim JY, Kim TS, et al. Long-term efficacy of prophylactic cavotricuspid isthmus ablation during atrial fibrillation ablation in patients without typical atrial flutter: a prospective, multicentre, randomized trial. Korean Circ J. 2021;51(1):58–64.
Inoue K, Murakawa Y, Nogami A, Shoda M, Naito S, Kumagai K, et al. Current status of catheter ablation of atrial fibrillation in Japan: summary of the 4th survey of the Japanese Catheter Ablation Registry of Atrial Fibrillation (J-CARAF). J Cardiol. 2016;68(1):83–8.
Betts TR, Jones M, Wong KC, Qureshi N, Rajappan K, Bashir Y. Feasibility of mitral isthmus and left atrial roof linear lesions using an 8 mm tip cryoablation catheter. J Cardiovasc Electrophysiol. 2013;24(7):775–80.
Knecht S, Hocini M, Wright M, Lellouche N, O’Neill MD, Matsuo S, et al. Left atrial linear lesions are required for successful treatment of persistent atrial fibrillation. Eur Heart J. 2008;29(19):2359–66.
Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372(19):1812–22.
Kuck KH, Brugada J, Furnkranz A, Metzner A, Ouyang F, Chun KR, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374(23):2235–45.
Arbelo E, Brugada J, Hindricks G, Maggioni AP, Tavazzi L, Vardas P, et al. The atrial fibrillation ablation pilot study: a European Survey on Methodology and results of catheter ablation for atrial fibrillation conducted by the European Heart Rhythm Association. Eur Heart J. 2014;35(22):1466–78.
Vasamreddy CR, Lickfett L, Jayam VK, Nasir K, Bradley DJ, Eldadah Z, et al. Predictors of recurrence following catheter ablation of atrial fibrillation using an irrigated-tip ablation catheter. J Cardiovasc Electrophysiol. 2004;15(6):692–7.
Rostock T, Salukhe TV, Steven D, Drewitz I, Hoffmann BA, Bock K, et al. Long-term single- and multiple-procedure outcome and predictors of success after catheter ablation for persistent atrial fibrillation. Heart Rhythm. 2011;8(9):1391–7.
Shah S, Barakat AF, Saliba WI, Abdur Rehman K, Tarakji KG, Rickard J, et al. Recurrent atrial fibrillation after initial long-term ablation success: electrophysiological findings and outcomes of repeat ablation procedures. Circ Arrhythm Electrophysiol. 2018;11(4):e005785.
Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D, et al. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace. 2018;20(1):33–42.
Yu HT, Shim J, Park J, Kim IS, Kim TH, Uhm JS, et al. Pulmonary vein isolation alone versus additional linear ablation in patients with persistent atrial fibrillation converted to paroxysmal type with antiarrhythmic drug therapy: a multicenter, prospective, randomized study. Circ Arrhythm Electrophysiol. 2017;10(6):e004915.
Chugh A, Oral H, Lemola K, Hall B, Cheung P, Good E, et al. Prevalence, mechanisms, and clinical significance of macroreentrant atrial tachycardia during and following left atrial ablation for atrial fibrillation. Heart Rhythm. 2005;2(5):464–71.
Deisenhofer I, Estner H, Zrenner B, Schreieck J, Weyerbrock S, Hessling G, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: incidence, electrophysiological characteristics, and results of radiofrequency ablation. Europace. 2006;8(8):573–82.
Acknowledgements
Full list of KARA investigators’ name (alphabetical order) and affiliation.
Jinhee Ahn1, Min-Soo Ahn2, Yong-Soo Baek3, Myung-Jin Cha4, Tae-Joon Cha5, Eue-Keun Choi4, Hyung-Oh Choi6, Jong-Il Choi7, Kwang Jin Chun8, Hye Bin Gwag9, Seongwook Han10, Youmi Hwang11, Dae Woo Hyun12, Eun-Sun Jin13, Ki-Woon Kang14, Dae-Hyeok Kim3, Dae-Kyung Kim15, Dongmin Kim16, Ji-Hoon Kim11, Jin-Bae Kim17, Minsu Kim18, Sung-Hwan Kim19, Yoo Ri Kim20, Young-Hoon Kim7, Jum-Suk Ko21, Jae-Jin Kwak22, Euijae Lee23, Sanghee Lee24, So-Ryoung Lee4, Sung Ho Lee25, Young Soo Lee26, Gi-Byung Nam27, Jun Namgung22, Il-Young Oh28, Seil Oh4, Yong-Seog Oh19, Young Keun On29, Hui-Nam Pak30, Hwan-Cheol Park31, Hyoung-Seob Park10, Hyung Wook Park32, Sang Weon Park23, Ye Min Park33, Young-Ah Park15, Kyoung-Suk Rhee34, Jaemin Shim7, Dong-Gu Shin35, In-Geol Song36, Jung-Hoon Sung37, Pil-Sung Yang37.
1Department of Internal Medicine, Pusan National University Hospital, Pusan National University College of Medicine, Busan, Korea; 2Department of Internal Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea; 3Department of Internal Medicine, Inha University Hospital, Inha University College of Medicine, Incheon, Korea; 4Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea; 5Department of Internal Medicine, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea; 6Department of Internal Medicine, Soonchunhyang University Hospital Bucheon, Soonchunhyang University College of Medicine, Bucheon, Korea; 7Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea; 8Division of Cardiology, Kangnam Sacred Heart Hospital, Hallym University Medical Center, Seoul, Korea; 9Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea; 10Department of Internal Medicine, Keimyung University Dongsan Medical Center, Keimyung University College of Medicine, Daegu, Korea; 11Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea; 12Department of Internal Medicine, Andong General Hospital, Andong, Korea; 13Cardiovascular Center, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea; 14Department of Internal Medicine, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea; 15Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea; 16Department of Internal Medicine, Dankook University Hospital, Dankook University School of Medicine, Cheonan, Korea; 17Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea; 18Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Republic of Korea; 19Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea; 20Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea; 21Department of Internal Medicine, Wonkwang University Hospital, Wonkwang University School of Medicine, Iksan, Korea; 22Department of Internal Medicine, Vision 21 Cardiac & Vascular Center, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea; 23Department of Cardiology, Bucheon Sejong Hospital, Bucheon, Korea; 24Department of Internal Medicine, Pohang Semyeong Christianity Hospital, Pohang, Korea; 25Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea; 26Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea, 27Heart Institute, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea; 28Cardiovascular Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea; 29Department of Internal Medicine, Heart Vascular and Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 30Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea; 31Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea; 32Department of Cardiology, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea; 33Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea; 34Department of Internal Medicine, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea; 35Department of Internal Medicine, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea; 36Heart center, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea; 37Department of Cardiology, CHA Bundang Medical Center, CHA University. Seongnam, Korea.
Funding
This nationwide registry study was supported by a grant from the Korean Heart Rhythm Society 2017.
Author information
Authors and Affiliations
Consortia
Contributions
SO contributed to the conception, design, acquisition and analysis of data and critical revision of the manuscript. EL and HSP contributed to the interpretation of data for the work and drafting of the manuscript. HSP, SH, GBN, JIC, HNP, IYO, DGS, YKO, SWP, YHK, and SO contributed to the design, acquisition and analysis of data for the work. All authors approved the final version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study protocol was approved by the Institutional Review Board of the Seoul National University and each participating center.
Consent for publication
Not applicable.
Competing interests
There are no competing interests for this study in all authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, E., Park, HS., Han, S. et al. Catheter ablation of atrial fibrillation in Korea: results from the Korean Heart Rhythm Society Ablation Registry for Atrial Fibrillation (KARA). Int J Arrhythm 22, 20 (2021). https://doi.org/10.1186/s42444-021-00047-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-021-00047-7