Abstract
Background
Many people with non-specific chronic low back pain (NSCLBP) do not recover with current conventional management. Systematic reviews show multidimensional treatment improves pain better than usual active interventions. It is unclear whether multidimensional physiotherapy improves pain better than usual physiotherapy. This study determines the effectiveness of this treatment to reduce pain and disability and improve quality of life, pain cognitions, and electroencephalographic pattern in individuals with NSCLBP.
Methods
70 eligible participants aged 18 to 50 years with NSCLBP were randomized into either the experimental group (multidimensional physiotherapy) or the active control group (usual physiotherapy). Pain intensity was measured as the primary outcome. Disability, quality of life, pain Catastrophizing, kinesiophobia, fear Avoidance Beliefs, active lumbar range of motion, and brain function were measured as secondary outcomes. The outcomes were measured at pre-treatment, post-treatment, 10, and 22 weeks. Data were analyzed using intention-to-treat approaches.
Results
There were 17 men and 18 women in the experimental group (mean [SD] age, 34.57 [6.98] years) and 18 men and 17 women in the active control group (mean [SD] age, 35.94 [7.51] years). Multidimensional physiotherapy was not more effective than usual physiotherapy at reducing pain intensity at the end of treatment. At the 10 weeks and 22 weeks follow-up, there were statistically significant differences between multidimensional physiotherapy and usual physiotherapy (mean difference at 10 weeks, -1.54; 95% CI, -2.59 to -0.49 and mean difference at 22 weeks, -2.20; 95% CI, − 3.25 to − 1.15). The standardized mean difference and their 95% confidence intervals (Cohen’s d) revealed a large effect of pain at 22 weeks: (Cohen’s d, -0.89; 95% CI (-1.38 to-0.39)). There were no statistically significant differences in secondary outcomes.
Conclusions
In this randomized controlled trial, multidimensional physiotherapy resulted in statistically and clinically significant improvements in pain compared to usual physiotherapy in individuals with NSCLBP at 10 and 22 weeks.
Trial Registration
ClinicalTrials.gov NCT04270422; IRCT IRCT20140810018754N11.
Similar content being viewed by others
Introduction
Non-specific chronic low back pain (NSCLBP) is a common musculoskeletal disorder, leading to a considerable personal, social, and economic burden [1,2,3,4,5]. The effective management of NSCLBP is a major concern for individuals, the economy, and society [6]. While there is a wide range of guideline-based management for NSCLBP, disability and burden have been increasing, leading to persistent, worsening, and recurrent pain [3, 7,8,9,10]. Despite the large volume of clinical research focused on identifying effective treatments for NSCLBP, optimal management remains a point of contention [11]. In recent decades, NSCLBP has been considered a multidimensional experience characterized by physical, psychological, behavioral, lifestyle, and social factors, and effective treatment requires intervention that specifically addresses these factors [11, 12]. This has led to the evolution of multidisciplinary biopsychosocial rehabilitation (MBR) programs [11, 12]. These programs typically involve a combination of physical, psychological, educational, lifestyle, and work-related components delivered by a team of health care professionals from different disciplines [3, 11,12,13,14]. Systematic reviews indicate that MBR programs are more effective than usual care or active physical interventions for reducing pain and disability in people with chronic low back pain11. Nevertheless, there is no evidence to guide the decision-making about the most optimal way, dose, and content to deliver MBR programs for patients with chronic low back pain. Also, given the moderate size of MBR effects and the potentially high monetary and time of intensive intervention, the decision to refer to MBR requires some consideration [11, 12, 15,16,17]. Furthermore, psychological factors involved in NSCLBP are not necessarily mental health disorders that require assessment and management by a mental health provider. For instance, kinesiophobia or catastrophizing are pain-related disorders. They can be within the scope of musculoskeletal clinicians [18]. Hence, we designed a physiotherapy-led intervention called multidimensional physiotherapy that targets physical, psychological, and lifestyle factors.
Up to this point, little is known about the precise central mechanisms of chronic low back pain. Various researchers have identified a relationship between chronic pain and functional changes in electroencephalography (EEG) activity at different frequency bands [19,20,21,22,23,24,25,26,27,28,29,30]. Most studies on the power spectrum of EEG activity at rest have demonstrated that chronic pain displays increased power in frontal and parieto-occipital regions in the theta and alpha frequency bands [31,32,33,34,35,36]. Importantly, these EEG activity changes are suggested to be reversible with successful treatment. Therefore, a treatment addressing both functional changes and inappropriate pain cognitions might result in larger effect sizes and clinically relevant changes [37, 38]. Therefore, brain function analysis for studying central mechanisms involved in chronic low back pain and investigating the central effect of multidimensional physiotherapy could be of great value [29, 30].
Based on the above-described voids, this randomized controlled trial investigated whether multidimensional physiotherapy is superior to usual physiotherapy in reducing pain and improving functionality, and pain cognitions in people with NSCLBP. Also, we are assessing changes in EEG patterns following multidimensional physiotherapy.
Methods
Study design and setting
This study was a 22-week, outcome assessor-blind, randomized, controlled, parallel trial from April 2020 to February 2022. The study protocol has been published previously [39] (Additional file 1). The ethical committee of the Iran University of Medical Sciences (IUMS) approved this study (IR.IUMS.REC.1398.1041). Participants signed a reviewed and approved informed consent document. We followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.
Participants
We sought to recruit participants from hospitals, advertisements, and social media in Tehran, Iran. All participants were examined by a specialist for eligibility. Inclusion criteria were as follows: 18–50 years old; having permanent or intermittent local pain between L1 and gluteal fold for three months or more and a Numeric Rating Scale (NRS) score of 3–7/10 in the last week; the Oswestry Disability Index (ODI) score of 20–60; the Tampa Scale for Kinesiophobia (TSK) score > 37; elementary level of education and native Persian speaking. The exclusion criteria were having a specific medical diagnosis (such as fracture, canal stenosis), rheumatoid disease, fibromyalgia, neuropathy, progressive neurological disease, headache, dizziness, nausea, epilepsy, migraines, and mental disorders; having a history of lumbar surgery in the past three years; Beck’s Anxiety Inventory score > 26; Beck’s Depression Inventory-II score > 29; participating in other therapies during the present research and pregnancy. Then they participated in an initial screening interview to provide an overview of the study. Informed written consent was obtained from all participants before the baseline examination. After completing baseline examinations, individuals who agreed to participate in the study were assigned to either the experimental or active control group. A total of 246 patients with NSCLBP presented to participate in the present study, and researchers excluded 176 participants based on exclusion criteria.
Randomization and blinding
After performing a baseline assessment, participants were randomly assigned (1:1) to an experimental or active control group. A computer-generated randomization sequence was performed using a stratified permuted block allocation (block size of 4). The stratification factor was gender. The outcome assessor who evaluated the outcome of the study was blind to the allocation of the groups. An analyzer independent of the research team and blinded to participant assignment monitored and analyzed the study data. In addition, the person who assigned participants was instructed not to disclose the status of the assignment to patients at any time. Details of the study protocols have been previously published.
Outcome measures
The primary outcome was pain, assessed by NRS at baseline, after six weeks of treatment, and after 10 and 22 weeks of follow-up. The NRS uses an 11-point scale to measure pain intensity [40].
The secondary outcomes included pain cognitions, disability, quality of life, active lumbar forward flexion, and brain function. Brain function was measured using the EEG power spectra analysis. EEG was recorded (bandwidth is 0-0.70 Hz, the pass filter is 0.05–60 Hz, and the sampling rate is 512 Hz) with a 64-channel amplifier (EB Neuro, Italy). The cap with 19 Ag–AgCl electrodes (impedance below 20 KOhm) was positioned according to the international 10–20 system at Fp1, Fp2, F7, F3, Fz, F4, F8, T3, C3, Cz, C4, T4, T5, P3, Pz, P4, T6, O1, O2. We placed references and ground electrodes on the mastoid processes (A1 and A2) and the Fpz region. EEG signals were recorded under two conditions: three minutes of an eyes-open resting state and 20 s of active lumbar forward flexion. The absolute and relative (percentage of total EEG power) EEG power spectra analyses of the following frequency domains were calculated: delta (1–3.8 Hz), theta (4.0–7.8 Hz), alpha (8.0–13.8 Hz), beta (14.0–34.8 Hz), and gamma (35–50 Hz).
The following questionnaires were used to assess pain cognitions: The Pain Catastrophizing Scale [41]; the Tampa Scale for Kinesiophobia [42]; and the Fear Avoidance Beliefs Questionnaire [43]; Quality of life and disability were measured using the 36 Health Status Survey (SF-36) [44] and the Oswestry Disability Index Questionnaire [45].
Study group interventions
Participants in each group received 12 treatment sessions delivered twice weekly for 6 weeks from their trained independent physiotherapists. The treatment in each session lasted equally long in the two groups.
Experimental group intervention
Participants in the experimental group received multidimensional physiotherapy. This treatment included psychoeducation, graded exposure, postural correction and electrotherapy as a passive warm-up. In this study, we performed twelve 30-minute psychoeducation sessions based on cognitive behavioral therapy (CBT). Each session was conducted using the question-and-answer method. The physiotherapist first provided the desired content, then posed a question regarding the covered topic to ensure the patients’ attendance and active involvement in each session. At the end of each session, the patient was given a task to do at home and present in the next session. Out of the 12 sessions, three were dedicated to educating the patient on pain neurophysiology and achieving therapeutic goals. The contents of these sections were designed based on a summary of the book Explain Pain [46]. The other sessions consisted of anxiety management, interpersonal conflict management, problem-solving training, coping strategy training, pain flare-ups management, medication abuse management, enhancing the ability to cope with labeling and stigma, empowering one to create a daily sleep routine, and training relaxation techniques [47]. Each topic is discussed in one session. Table 1 shows the details of psychoeducation treatment in the experimental group. Participants also received recommendations for postural correction, and gradual initiation of movements and activities that are feared. We asked participants to repeat the practice of each session at home once a day. Electrotherapy, including 20 min of transcutaneous electrical nerve stimulation (TENS) at 100 Hz frequency in the lumbar region with a hot pack and ultrasound with a frequency of 1 MHz and intensity of 1.2 W/cm2, was performed on the paravertebral muscle for 5 min.
Active control group intervention
Participants in the active control group received usual physiotherapy including traditional back school education (three sessions), general trunk exercises, and electrotherapy as a passive warm-up. Back school education covered basic anatomy and biomechanics of the spine, common causes of spinal pain, nociceptive pain processing, and ergonomic counseling based on the inherent postural strain associated with various postures and daily activities (including standing, sitting, and lifting). As such, the education sessions prepared the patients for a symptom-contingent, biomedical approach to daily activity and exercise therapy. In session four, general exercise therapy was started with a specific emphasis on treating dysfunctional muscles and joints. Different therapeutic goals were pursued (microcirculation, mobility, endurance, strength of the abdominal and paraspinal muscles) depending on what emerges from the clinical reasoning as the most dominant peripheral dysfunction. The progressive exercise program mainly entailed an increase in exercise intensity, and an evolution towards functional activities and more physically demanding tasks while keeping the spine in physiologically neutral positions to minimize strain imposed upon the spinal structures. All exercises were performed in a symptom-contingent way (Additional file 3). They also received electrotherapy, the same as the experimental group.
Training of the physiotherapists and treatment fidelity
The two independent physiotherapists provided interventions in each group. The physiotherapist who conducted treatment in the active control group had ten-year experience in musculoskeletal treatment. The specific training for CBT-based psychoeducation was developed to enhance the standardization. The training involved (1) participating in learning sessions and interactive classes with an expert psychologic in the field of psychoeducation on pain, as well as clinical workshops where the management of NSCLBP as a multidimensional disorder was discussed (2) assessing and treating actual patients with NSCLBP (3) assessing and treating patients with NSCLBP in front of an expert.
A fidelity evaluation was conducted in which the physiotherapists were observed while assessing and treating actual patients from the study. For each participant, session-by-session documentation of treatment content was recorded by the physiotherapists. Regular training, supervision, and feedback were provided to the physiotherapists throughout the study to facilitate the successful delivery of both treatments. Physiotherapists provided demographic details and information about their training at each session. For qualitative evaluation, some sessions of both intervention groups were observed and audio recorded.
Sample size calculation
The sample size was calculated using G*Power software 3.1.9.4 (Düsseldorf, Germany) based on the effects on pain in the pilot study (partial η2 = 0.04, α = 0.025, power = 0.95) and accounted for F tests and 10% loss to follow-up after 22 weeks, resulting in a total sample size of 70 individuals [48].
Statistical analysis
Stata 14.2 (StataCorp LLC; College Station, TX, USA) and SPSS (version 22) were used to analyze all data. We performed an intention-to-treat analysis for participants who dropped out of the study at follow-up. Continuous and categorical baseline variables were summarized using mean (standard deviation), median (interquartile range), and frequency (percentages) to determine descriptive statistics. A mixed model ANOVA/ANCOVA was used to determine the time effect, group effect, and time × group interaction effect between groups, using the Bonferroni post hoc method and adjusting for differences in patients’ characteristics at baseline where appropriate were done. The assumption of homogeneity and sphericity were checked by Levene’s and Mauchly’s tests respectively. When the assumption of sphericity is violated, Greenhouse-Geisser corrections are used. Similar analyses examined the treatment effect for all secondary outcomes. Subgroup analyses were planned for the pain catastrophizing variable (mild, moderate, and severe pain catastrophizing). We also calculated the effect size (Cohen’s d) for each pairwise comparison, using the pooled SD of baseline scores, where 0.2 was considered a small effect, 0.5 a moderate effect, and 0.8 a large effect [49]. Statistical significance was indicated at p ≤ 0:05 (2-sided), and the confidence interval was set at 95%. The statistician was blinded to group allocation.
Deviations from the registered trial protocol
We made some deviations from our protocol. In calculating the follow-up period of one and four months, we considered the end of the treatment period, which was finally corrected 10- and 22 weeks after randomization. In the design phase of the trial, we designed a three-blind study, but in the pilot study, it was not possible to implement the first phase of blinding, so we conducted the study as an outcome assessor blind study.
Results
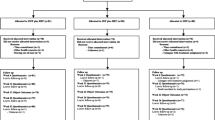
A total of 70 people with NSCLBP (mean [SD] age, 35.26 [7.23] years; age range, 22–50 years) were included in the present trial and received either experimental group (mean [SD] age, 34.57 [6.98] years; 18 [51%] women and 17 [49%] men) or active control group (mean [SD] age, 35.94 [7.51] years; 17 [49%] women and 18 [51%] men). Figure 1 shows the flow of participants through the trial. The baseline characteristics of these participants are presented in Table 2. As shown in Table 2, the two groups had similar demographic (except for body weight) and clinical characteristics (except for PCS, FABQ) at baseline. Sixty-two of the 70 participants completed all treatment sessions and 22 weeks of follow-up.
Primary outcome
The results indicated that the primary outcome, pain, has a significant main effect of time and treatment × time interaction effects. Post hoc tests revealed that the experimental group experienced greater pain improvement in comparison to the active control group. The mean [SD] pain intensity decreased from 5.03 [0.92] at baseline to 1.74 [1.74] at 10 weeks and 1.66 [2.00] at 22 weeks in the experimental group. The mean [SD] pain intensity in the active control group decreased from 5.09 [0.95] at baseline to 3.29 [2.01] at 10 weeks and 3.86 [2.35] at 22 weeks (Fig. 2). The mean between-group difference [MD] and 95% confidence intervals (95% CI) was (MD, 1.54; 95% CI, -2.59 to -0.49) in 10 weeks follow up and (MD, 2.20; 95% CI, -3.25 to -1.15) in 22 weeks follow up. Standardize mean between-group difference and their 95% CI (Cohen’s d, 95% CI) showed a medium effect (Cohen’s d, -0.62; 95% CI ( -1.10 to -0.14)) in 10 weeks and a large effect (Cohen’s d, -0.89; 95% CI (-1.38 to -0.39)) in 22 weeks follow up of treatment group on pain intensity (Tables 3 and 4).
Secondary outcomes
There were an inconclusive (medium effect size; statistically significant) effect for absolute power of alpha frequency in frontal (Cohen’s d, -0.59; 95% CI (-1.03 to -0.79)) and central (Cohen’s d, -0.70; 95% CI (-1.18 to -0.21)) region in active lumbar forward flexion. Also, there were an inconclusive and statistically significant effect for relative power of alpha frequency in the frontal (Cohen’s d, -0.82; 95% CI (-1.31 to -0.33)), parietal (Cohen’s d, -0.70; 95% CI (-1.19 to -0.22)), temporal (Cohen’s d, -0.72; 95% CI (0.25 to 1.21)), and occipital (Cohen’s d, -1.04; 95% CI (-1.53 to -0.53)) regions, and gamma frequency in the central (Cohen’s d, -0.93; 95% CI (-1.42 to -0.43)), and temporal (Cohen’s d, -0.68; 95% CI (-1.16 to -0.19)) regions in the open-eye resting position. For other EEG outcomes, there were no statistically significant differences at any of the time points (Additional file 2).
Multidimensional physiotherapy was not more effective than usual physiotherapy (no statistically significant differences) in other secondary outcomes (Tables 3 and 4). The comparison between the full model and the reduced model ANOVA/ANCOVA to assess the effect of the baseline, and demographic characteristics of pain catastrophizing, fear-avoidance beliefs, and body weight on the intervention effect showed that the result of the primary outcome was not affected by the potential confounder of the participants’ body weight or differences of pain catastrophizing and fear avoidance believes at baseline. Subgroup analysis on pain catastrophizing (mild_PCS (n = 26), moderate_PCS (n = 35), severe_PCS (n = 9)) showed a very large effect of treatment in mild (Glass’Δ: -1.44; 95%CI (-2.36 to -0.47)) and moderate (Glass’Δ: -1.41; 95%CI (-2.26 to -0.54)) catastrophizing and a low effect in severe catastrophizing (Glass’Δ: -0.25; 95%CI (-1.40 to -1.80)).
Discussion
This randomized controlled trial aimed to evaluate the efficacy of multidimensional physiotherapy compared to usual physiotherapy in people with NSCLBP. The results provided evidence that multidimensional physiotherapy improves pain in people with NSCLBP. The effect on pain was of clinical importance [50] (large effect size and three points of improvement in pain) and lasted for medium-term follow-up.
Primary outcome: pain
The results showed that both physiotherapy treatments improved the pain intensity in individuals with NSCLBP. The multidimensional physiotherapy was not more effective than usual physiotherapy at the end of the six-week treatment but the effects emerged during the follow-up period. We found a meaningful, large, and acceptable power effect on pain reduction in the experimental group. Moreover, the number needed to treat (NNT) was three, which means three participants would need to be treated with multidimensional physiotherapy instead of usual physiotherapy for one of them to benefit from reduced pain (large effect). Potential hypotheses for this result could be the biopsychosocial content of multidimensional physiotherapy, which affects modifiable psychological dimensions of pain rather than focusing specifically on signs and symptoms associated with the NSCLBP [51,52,53]. The psychoeducation about chronic pain revealed the role of beliefs, emotions, and behavior in coping strategies with NSCLBP. In multidimensional physiotherapy, there was a clear focus on self-management of NSCLBP to enable patients to develop an adaptive response pattern and deal with pain in daily life. People with chronic pain have a selective attentional bias toward their pain, and the difficulty to disengage from it can be driven by pain-related cognitions and emotions. When a physiotherapist provides psychoeducation, graded activity, and lifestyle modifications, participants better learn to put pain into proper perspective, feel empowered to control their pain, and be physically active [48, 51,52,53,54,55]. It is worth noting that psychoeducation based on the biopsychosocial approach had a sustained improvement in pain reduction in the experimental group over time rather than a substantial improvement in the short term. Although our study results provided valuable insights into the efficacy of multidimensional physiotherapy, it’s crucial to exercise prudence when generalizing the results. It’s important to acknowledge the constraint of the limited sample size in this study. Consequently, future research should address this limitation and provide a more holistic comprehension of the subject matter.
The significant pain improvement obtained in the present study for multidimensional physiotherapy was consistent with that reported in previous systematic reviews [16]. There have been studies on physiotherapy-based treatments with behavioral and cognitive components. Classification Based-Cognitive Functional Therapy (CB-CFT) is an example. CB-CFT provides individualized, pathoanatomical, neurophysiological, psychosocial, physical, and lifestyle treatment for low back pain [56]. O’Keeffe M et al. found no significant between-group differences in pain intensity at either six months or 12 months of CFT treatment compared with the group-based exercise and education intervention in 206 adults with CLBP [5]. Vibe-Fersum K. et al. found significant between-group differences in pain intensity at 12 months in favor of CFT compared with manual therapy and exercise but no significant between-group differences at three years of follow-up [57, 58].
Secondary outcomes: brain function and pain cognitions
According to studies, there is a general trend toward increased power at EEG frequencies, mainly in theta and alpha frequencies, in different types of chronic pain at rest in various brain regions, including frontal, parietal, occipital, sensorimotor, and somatosensory [31, 59].
Based on the previous research [37, 59], an effective treatment may reduce the power of EEG at different frequency bands. Our findings showed a decrease in alpha frequency relative power in lumbar forward flexion in all electrode locations after treatment, as we expected. This outcome indicates that intervention led to a change in brain function in favor of decreased power, especially in alpha frequency. As far as we know, this is the first randomized controlled trial study to record EEG in lumbar forward flexion. Our data is in contrast with Schmidt et al., who couldn’t show any changes in EEG findings after Mindfulness-based Stress Reduction (MBSR) treatment in people with chronic back pain [60]. Wang et al. showed that the overall EEG spectral power after the CBT group was lower than that of the control group, especially in the theta and beta frequency bands during the treatment period58. The result of the study didn’t show any meaningful differences in the relative power of EEG frequency in active lumbar flexion between both groups.
Regarding other secondary outcomes, the results showed the non-considerable effect of multidimensional physiotherapy (Table 4). Although our hypothesis was greater improvement in pain-related psychological factors, disability and quality of life, and active lumbar flexion in the experimental group, the result didn’t show a considerable effect on these outcomes. Multidimensional physiotherapy is no better at reducing fear-avoidance beliefs, kinesiophobia, pain catastrophizing, disability, quality of life, and active lumbar flexion than usual physiotherapy (Additional file 2).
Clinical implications
This exploratory randomized controlled trial showed multidimensional physiotherapy produced greater improvement in pain (large effect size and clinically important result) compared to usual physiotherapy in people with NSCLBP. Providing multidimensional treatment by a trained physiotherapist can be cost-effective and time-effective for patients and healthcare providers. These findings provide crucial information for clinical decision-making, optimization of health care services, and a basis for future research.
Limitations
This study has some limitations. First, because of the exploratory content of the study, the sample size consisted mainly of people aged between 18 and 50 years with moderate pain, moderate to severe disability (20 < ODI < 60), and also TSK ≥ 37, which indicates there is kinesiophobia. Therefore, our results may not generalize to adults with NSCLBP over 50 years, people with more severe pain, more or less disability and kinesiophobia, and those with anxiety or depression. Second, because this study included people with NSCLBP, other populations require study to see if these results can be generalized to a broad population with chronic pain. Third, this study was a medium-term follow-up. Future research should be designed by long-term follow-up. Fifth, because of a wide range of CI, our main result of pain was inconclusive; therefore, we recommended repeating the study with a large sample size.
Data availability
Study data can be made available upon reasonable request to the principal investigator.
Abbreviations
- NSCLBP:
-
Non-specific chronic low back pain
- NRS:
-
Numeric Rating Scale
- CNS:
-
Central nervous system
- EEG:
-
Electroencephalography
- ROM:
-
Range of Motion
- ODI:
-
Oswestry Disability Index
- TSK:
-
Tampa Scale for Kinesiophobia
- SF-36:
-
36 Health Status Survey
- PCS:
-
Pain Catastrophizing Scale
- FABQ:
-
Fear Avoidance Beliefs Questionnaire
- CBT:
-
Cognitive behavioral therapy
- MBR:
-
Multidisciplinary biopsychosocial rehabilitation
- CI:
-
Confidence Interval
- SD:
-
Standard Deviation
References
Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–47.
Hartvigsen J, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67.
Foster NE, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–83.
Buchbinder R, et al. Low back pain: a call for action. Lancet. 2018;391(10137):2384–8.
O’Keeffe M, et al. Cognitive functional therapy compared with a group-based exercise and education intervention for chronic low back pain: a multicentre randomised controlled trial (RCT). Br J Sports Med. 2020;54(13):782–9.
O’Sullivan PB, et al. Cognitive functional therapy: an integrated behavioral approach for the targeted management of disabling low back pain. Phys Ther. 2018;98(5):408–23.
Kovacs FM, et al. Non-specific low back pain in primary care in the Spanish National Health Service: a prospective study on clinical outcomes and determinants of management. BMC Health Serv Res. 2006;6:57.
Richmond H, et al. The effectiveness of cognitive behavioural treatment for non-specific low back Pain: a systematic review and Meta-analysis. PLoS ONE. 2015;10(8):e0134192.
Delitto A, et al. Low back pain. J Orthop Sports Phys Ther. 2012;42(4):A1–57.
Mas RR, et al. Effectiveness of a multidisciplinary BIOPSYCHOSOCIAL intervention for non-specific SUBACUTE low back pain in a working population: a cluster randomized clinical trial. BMC Health Serv Res. 2019;19(1):962.
Kamper SJ, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444.
Casey MB, et al. Multidisciplinary-based Rehabilitation (MBR) compared with active physical interventions for Pain and disability in adults with Chronic Pain: a systematic review and Meta-analysis. Clin J Pain. 2020;36(11):874–86.
National Guideline C. National Institute for Health and Care Excellence: Guidelines, in Low Back Pain and Sciatica in Over 16s: Assessment and Management. 2016, National Institute for Health and Care Excellence (NICE) Copyright © NICE, 2016.: London.
Qaseem A, et al. Noninvasive treatments for Acute, Subacute, and chronic low back Pain: a clinical practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30.
Schmidt AM, et al. The effect of an integrated multidisciplinary rehabilitation programme for patients with chronic low back pain: long-term follow up of a randomised controlled trial. Clin Rehabil. 2021;35(2):232–41.
Salathé CR, Efficacy T, et al. Clinical utility, and cost-effectiveness of Multidisciplinary Biopsychosocial Rehabilitation Treatments for Persistent Low Back Pain: a systematic review. Global Spine J. 2018;8(8):872–86.
Wade DT. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil. 2020;34(5):571–83.
O’Sullivan P. It’s time for change with the management of non-specific chronic low back pain. Br J Sports Med. 2012;46(4):224–7.
Flor H. Cortical reorganisation and chronic pain: implications for rehabilitation. J Rehabil Med. 2003;41(Suppl):66–72.
Lotze M, Moseley GL. Role of distorted body image in pain. Curr Rheumatol Rep. 2007;9(6):488–96.
Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–30.
Moseley LG. I can’t find it! Distorted body image and tactile dysfunction in patients with chronic back pain. Pain. 2008;140(1):239–43.
Wand BM, O’Connell NE. Chronic non-specific low back pain - sub-groups or a single mechanism? BMC Musculoskelet Disord. 2008;9:11.
Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1(3):182–9.
MacIver K, et al. Phantom limb pain, cortical reorganization and the therapeutic effect of mental imagery. Brain. 2008;131(Pt 8):2181–91.
Dubin AE, Patapoutian A. Nociceptors: the sensors of the pain pathway. J Clin Invest. 2010;120(11):3760–72.
Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55(3):377–91.
Roy M, et al. Cerebral and spinal modulation of pain by emotions. Proc Natl Acad Sci U S A. 2009;106(49):20900–5.
Kregel J, et al. Structural and functional brain abnormalities in chronic low back pain: a systematic review☆. In seminars in arthritis and rheumatism. Elsevier; 2015.
Davis KD, Moayedi M. Central mechanisms of pain revealed through functional and structural MRI. J Neuroimmune Pharmacol. 2013;8(3):518–34.
Pinheiro ES, et al. Electroencephalographic patterns in Chronic Pain: a systematic review of the literature. PLoS ONE. 2016;11(2):e0149085.
Apkarian AV, et al. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9(4):463–84.
Sarnthein J, Jeanmonod D. High thalamocortical theta coherence in patients with neurogenic pain. NeuroImage. 2008;39(4):1910–7.
Schulz E, et al. Prefrontal Gamma Oscillations Encode Tonic Pain in humans. Cereb Cortex. 2015;25(11):4407–14.
Baumgarten TJ, et al. Beta peak frequencies at Rest correlate with endogenous GABA+/Cr concentrations in Sensorimotor Cortex Areas. PLoS ONE. 2016;11(6):e0156829.
Feng L et al. Low Back Pain Assessment Based on Alpha Oscillation Changes in Spontaneous Electroencephalogram (EEG). Neural Plast, 2021. 2021: p. 8537437.
Sarnthein J, et al. Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain. 2006;129(Pt 1):55–64.
Schmidt S, et al. Pain ratings, psychological functioning and quantitative EEG in a controlled study of chronic back pain patients. PLoS ONE. 2012;7(3):e31138.
Bemani S, et al. Efficacy of a multidimensional versus usual care physiotherapy on pain and electroencephalography (EEG) spectrum in chronic nonspecific low back pain: study protocol for a randomized controlled trial. Trials. 2021;22(1):679.
Farrar JT, et al. Validity, reliability, and clinical importance of change in a 0–10 numeric rating scale measure of spasticity: a post hoc analysis of a randomized, double-blind, placebo-controlled trial. Clin Ther. 2008;30(5):974–85.
Raeissadat SA, Sadeghi S, A.J.J.B.A.S R, Montazeri. Validation of the pain catastrophizing scale (PCS) in Iran. 2013. 3(9): p. 376–80.
Abedi M, et al. Translation and validation of the Persian version of the STarT Back Screening Tool in patients with nonspecific low back pain. Man Ther. 2015;20(6):850–4.
Rostami M, et al. Validation of the Persian version of the fear avoidance belief questionnaire in patients with low back pain. J Back Musculoskelet Rehabil. 2014;27(2):213–21.
Montazeri A, et al. The short Form Health Survey (SF-36): translation and validation study of the iranian version. Qual Life Res. 2005;14(3):875–82.
Mousavi SJ, et al. The Oswestry Disability Index, the Roland-Morris disability questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the iranian versions. Spine (Phila Pa 1976). 2006;31(14):E454–9.
Butler DS, Moseley GL. Explain Pain 2nd Edn. Noigroup publications; 2013.
Carlson M. CBT for chronic pain and psychological well-being: a skills training manual integrating DBT, ACT, behavioral activation and motivational interviewing. John Wiley & Sons; 2014.
Malfliet A, et al. Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: a randomized clinical trial. JAMA Neurol. 2018;75(7):808–17.
Ostelo RW, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33(1):90–4.
Kraemer HC, et al. Measures of clinical significance. J Am Acad Child Adolesc Psychiatry. 2003;42(12):1524–9.
Vibe Fersum K, et al. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: a randomized controlled trial. Eur J Pain. 2013;17(6):916–28.
Sveinsdottir V, Eriksen HR, Reme SE. Assessing the role of cognitive behavioral therapy in the management of chronic nonspecific back pain. J pain Res. 2012;5:371.
Semrau J, et al. Long-term effects of interprofessional biopsychosocial rehabilitation for adults with chronic non-specific low back pain: a multicentre, quasi-experimental study. PLoS ONE. 2015;10(3):e0118609.
Semrau J, et al. Effects of behavioural exercise therapy on the effectiveness of multidisciplinary rehabilitation for chronic non-specific low back pain: a randomised controlled trial. BMC Musculoskelet Disord. 2021;22(1):500.
Matheve T, Bogaerts K, Timmermans A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: a randomized controlled trial. J Neuroeng Rehabil. 2020;17(1):55.
Foster NE, et al. Stratified models of care. Best Pract Res Clin Rheumatol. 2013;27(5):649–61.
Vibe Fersum K, et al. Efficacy of classification-based cognitive functional therapy in patients with non‐specific chronic low back pain: a randomized controlled trial. Eur J Pain. 2013;17(6):916–28.
Vibe Fersum K, et al. Cognitive functional therapy in patients with non-specific chronic low back pain-a randomized controlled trial 3-year follow-up. Eur J Pain. 2019;23(8):1416–24.
Wang J, et al. Cognitive behavioral therapy eases orthodontic pain: EEG states and functional connectivity analysis. Oral Dis. 2015;21(5):572–82.
Schmidt S, et al. Mindfulness-based stress reduction (MBSR) as treatment for Chronic Back Pain - an Observational Study with Assessment of Thalamocortical Dysrhythmia. Forsch Komplementmed. 2015;22(5):298–303.
Acknowledgements
Not applicable.
Funding
This study did not receive financial resources.
Author information
Authors and Affiliations
Contributions
Access to data and data analysis: Ms Bemani and Dr Sarrafzadeh had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; Concept and design: Bemani, Sarrafzadeh, Zarei, Talebian; Acquisition, analysis, or interpretation of data: Bemani, Salehi; Drafting of the manuscript: Bemani, Noorizadeh; Critical revision of the manuscript for important intellectual content: Sarrafzadeh, Salehi; Statistical analysis: Bemani, Keshtkar; Administrative, technical, or material support: All authors; Supervision: Sarrafzadeh, Noorizadeh. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of the Iran University of Medical Sciences (IUMS) approved this study (IR.IUMS.REC.1398.1041) and all participants gave their informed consent before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bemani, S., Sarrafzadeh, J., Dehkordi, S.N. et al. Effect of multidimensional physiotherapy on non-specific chronic low back pain: a randomized controlled trial. Adv Rheumatol 63, 57 (2023). https://doi.org/10.1186/s42358-023-00329-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-023-00329-9