Abstract
Background/Objective
The effects of Chikungunya virus (CHIKV) infection on patients with rheumatic diseases have not been extensively studied. Our aim was to compare the clinical course of patients with rheumatoid arthritis and spondyloarthritis, categorized according to the use or not of biologic disease modifying anti-rheumatic drugs (bDMARDs), during and after infection by CHIKV.
Methods
Patients from a northeastern Brazilian city that suffered an epidemic outbreak of Chikungunya fever (CHIK) between Oct 2015 and Jul 2016, on regular follow-up in a longitudinal registry of rheumatic patients (BiobadaBrasil), were invited to participate. Participants underwent a standardized clinical interview and collection of blood sample for serological tests (IgM/IgG) for CHIKV. A positive IgG was considered evidence of previous CHIKV infection.
Results
105 patients (84 with rheumatoid arthritis, 17 with ankylosing spondylitis, and 4 with psoriatic arthritis) were evaluated. Most patients (58, 55.2%) were on therapy with bDMARDs. The overall prevalence of seropositivity for CHIKV was 47.6% (39.7% in patients on bDMARDs and 57.4% in those exclusively on conventional synthetic (cs-) DMARDs (p = 0.070). Among seropositive patients, asymptomatic disease had similar frequency in those treated and not treated with bDMARDs (39.1% versus 33.3%, respectively; p = 0.670). However, patients exclusively on csDMARDs presented significantly higher prevalence of articular symptoms beyond 3 months and switched treatment more often than patients on bDMARDs (p < 0.05 for both comparisons).
Conclusions
Among rheumatic patients with CHIK, those on bDMARDs had shorter persistence of articular symptoms and switched treatment scheme less often than patients exclusively treated with csDMARDs.
Similar content being viewed by others
Background
The Chikungunya virus (CHIKV) was isolated in 1953 and received this name, derived from the African Makonde dialect meaning “that which bends up”, due to the posture acquired by affected patients related to intense musculoskeletal pain in the disease acute phase [1]. Over the following decades, isolated outbreaks of Chikungunya fever (CHIK) occurred in the African continent and major epidemics were observed in Africa (2004) and in the Reunion Islands (2005) [2]. CHIK arrived in Brazil in 2014 and quickly caused the first epidemic in the continent, spreading to most countries in Latin America [1].
The CHIKV infection causes a rapid-onset febrile disease associated with severe musculoskeletal pain due to the arthritogenic character of the virus [2]. Eighty-five percent of cases are symptomatic and the disease-related social impact is generally significant, especially in naive populations. Other symptoms, such as itchy rash, myalgia, fatigue, headache, paresthesia, lower limb edema, and symptoms of the digestive and respiratory tract may also appear in the acute phase of the condition [2]. Chronic musculoskeletal pain is defined as pain during more than 3 months that affects bones, muscles, ligaments, tendons and/or nerves [3]. In CHIK chronic musculoskeletal pain can last longer than 3 months and become long-lasting and persistent. In the first two years after the onset of the CHIK, the prevalence of persistent musculoskeletal pain in näive patients varies from 54 to 79% [4]. The persistence of articular pain symptoms was evaluated in a systematic review, including more than 6500 patients from Reunion Island, Italy, France, Mauritius, India, Sri Lanka, Suriname, Germany, South Africa, Colombia, Singapure and Caribbean. After three months, 43% of patients still have painful symptoms and after 12 months of follow-up, the non-recovery rate was 21% [5]. The origin of pain may be articular (arthralgia and/or arthritis) and/or periarticular (tenosynovitis, fasciitis, and/or compressive nervous syndromes) [4, 6, 7].
Many patients undergoing immunosuppressive treatment for inflammatory rheumatic diseases are also affected by CHIK, and the resulting clinical consequences are not clear. Despite the recognized benefit of these drugs in treating rheumatic diseases, their immunomodulatory and immunosuppressive effect could predispose users to the risk of infection [8]. On the other hand, the use of medications that block the inflammatory process could reduce CHIK-related joint symptoms [9]. Although there was initially a concern about the effects of CHIK in patients using conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) and biological DMARDs (bDMARDs), clinical practice and some reports in the literature demonstrate that there are no major complications in this population [9, 10].
The aim of this study is to compare the clinical course of rheumatic patients, treated with and without bDMARD, during and after the occurrence of a proven, clinically symptomatic infection by CHIKV in the context of an epidemic outbreak.
Methods
This is a retrospective study nested in a cohort of patients participating in the Brazilian Registry of Adverse Events of Biological Therapies in Rheumatic Diseases (BiobadaBrasil). BiobadaBrasil is a registry-based longitudinal study of adult patients with active rheumatic diseases starting their first bDMARD or targeted synthetic (ts-) DMARD or a new csDMARD (without previous use of b- or tsDMARDs). Recruitment of patients to BiobadaBrasil started in January 2009 [11]. For the present study, we selected patients recruited in Rheumatology centers located in Recife, a northeastern state capital in Brazil that underwent an epidemic outbreak of CHIK between October 2015 and July 2016 [12]. The inclusion criterion was enrollment in BiobadaBrasil before October 2015 and the patients should be regularly attended in one of the two public hospitals where the study was held. In the BiobadaBrasil protocol, the patients included should be on bDMARD, tsDMARD or csDMARD treatment since their entry in the cohort and must be on stable current therapy. In case of suspension of bDMARD for more than 30 days after the missed application of bDMARDs, the patient is excluded from BiobadaBrasil study.
The exclusion criterion was denial to undergo the study procedures (blood collection or fulfilling the standard study protocol). Written informed consent was obtained from each subject and all experimental procedures were approved by the local ethics committee (certificate of ethical approval [CAAE] number 54275516.9.1001.5208).
Patients were invited by telephone to participate in this study, and data were collected between July 2017 and July 2018. Each subject was evaluated and examined in a single visit by a rheumatologist who recorded clinical and demographic features following a standardized questionnaire. The questionnaire asked specifically about symptoms suggestive of CHIKV infection occurring between October 2015 and July 2016 and the rheumatic drugs used in that time. This questionnaire was created by the investigators and has not been previously validated or submitted in a pilot study. At that moment, following the recommendation of the Brazilian Health Ministry, the diagnosis of CHIK was retrospectively made based in the combination of acute fever (> 38.5 ℃) with intense joint pain/arthritis of acute onset (high sensitivity and positive predictive value when residing at or visiting outbreak areas) or laboratorial evidence of CHIKV infection [13]. Information regarding the rheumatic disease, use of anti-rheumatic drugs, duration of symptoms suggestive of CHIK after the acute infection (if present), changes in treatment, comorbidities and possible complications were also collected by interview and through review of medical records. Switch of treatment was defined as the necessity to initiate or change the therapeutic scheme of DMARDs because of high disease activity. The intensity or worsening of joint symptoms related to CHIKV infection was assessed and defined by the Likert scale in five categories (grade of worsening of articular symptoms after the acute phase: none, mild, moderate, severe, or very severe) [14]. The definition of disease remission was made based on medical records and the patient`s opinion regarding their disease activity status. For the present analysis, confirmed cases of CHIK were those who presented a positive IgG test for CHIKV; these patients were classified as symptomatic or asymptomatic according to clinical history.
At the day of the interview, a sample of peripheral venous blood was collected (8 mL) into an anticoagulant-free vacuum tube; serum was extracted after centrifugation at 3000 rpm for 10 minutes and then stored at – 80 ℃. After collection of all study samples, serological tests for IgM and IgG for CHIK using the enzyme-linked immunosorbent assay (ELISA) method (IgM: Euroimmun, Luebeck, Germany, code EI 293a-9601 M; IgG: Euroimmun, Luebeck, Germany, code EI 293a-9601 G) was performed at LINAT/NUPIT (Laboratório de Imunomodulação e Novas Abordagens Terapêuticas-Núcleo de Pesquisa em Inovação Terapêutica; Laboratory of Immunomodulation and New Therapeutic Approaches / Therapeutic Innovation Research Center) at Universidade Federal de Pernambuco (UFPE). All tests were analyzed in a single run; optical density of each well was determined at 450 nm on a microplate reader (ELx808, BioTek, USA). Positive dosages of IgG were considered to be indicative of previous CHIKV infection, regardless of the history of CHIK symptoms.
Statistical analyses were made using the program SPSS for Windows, version 20.0. The results are expressed as numbers and percentages for categorical variables, while continuous variables were presented as means ± standard deviation (SD) or median and interquartile range (IQR). The association between categorical variables was tested using Pearson’s chi-square test or Fisher’s exact test. Stratified analysis was performed using the Mantel–Haenszel formula. Between group comparisons involving non-normal quantitative variables were performed using the Mann–Whitney test. P values less than or equal to 0.05 were considered statistically significant; all presented P values are 2-tailed.
Results
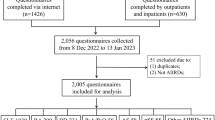
At the time of data collection, there were 122 patients being followed-up in BiobadaBrasil in the city of Recife. The flow chart of patients inclusion is demonstrated in Fig. 1.
The description of the clinical and demographic features of these patients, divided according to serologic and clinical status, is found in Table 1. Most patients were women, non-Caucasians, and rheumatoid arthritis (RA) was the most frequent rheumatic disease. Thirty-eight patients reported symptoms compatible with CHIK (four of them with negative IgG sorology). The overall seroprevalence of CHIKV IgG was 47.6%; this prevalence tended to be higher in patients exclusively on csDMARD (27/47, 57.4%) than in patients on bDMARD (23/58, 39.7%; p = 0.070). The prevalence of positive IgM for CHIKV was 16.5% (17/103) patients tested (19.6% in patients exclusively on csDMARDs versus 13.8% in patients on bDMARDs).
Of note among patients with IgG positive for CHIKV, the proportion of patients with asymptomatic infection was not significantly different between patients treated and not treated with bDMARDs (9/23, 39.1% versus 9/27, 33.3%, respectively; p = 0.670). Additionally for symptomatic patients, there was no significant difference in acute phase symptoms between these two groups of patients (Table 2). The bDMARDs used in CHIKV IgG-positive patients were anti-TNF (11 patients, 78,6%) and 1 patient using abatacept, 1 using rituximab and 1 in tocilizumab therapy. After CHIK onset, the intensity of worsening of joint symptoms related to infection was not significantly different between users and non-users of bDMARDs (p = 0.412). Regarding the time to recovering from persistent musculoskeletal symptoms in the CHIKV IgG-positive group, more patients using bDMARD recovered within 3 months compared to the csDMARD-only group (p = 0.017; see Table 2). Additionally, the bDMARD group switched treatment (added or switched DMARD) less frequently after CHIKV infection (p = 0.025). The proportion of patients in disease remission before CHIK was numerically higher in patients on biologics (10/14, 71.4% versus 8/18, 44.4%, in patients exclusively on csDMARDs). Nonetheless, stratification for disease remission did not change importantly the association of use of bDMARDs with lower persistence of musculoskeletal symptoms (Mantel Haenszel test, p = 0.014) and less treatment switch (p = 0.038). There were also no significant changes in these results when stratifying according to the csDMARDs being used (methotrexate, leflunomide or antimalarials; data not shown).
Most patients received either corticosteroids or had the dose increased during the period of CHIK articular symptoms, but interestingly there was no significant difference regarding changes in corticosteroid scheme between patients treated and not treated with bDMARDs (Table 2). No clinical major complications related to CHIK were observed in any of the groups.
In an exploratory analysis, we tested the hypothesis that positive IgM serology could be associated with persistence of symptoms for more than 3 months or more frequent switch of DMARDs among symptomatic patients. However, no statistically significant difference was observed in these tests (p = 0.782 and p = 0.865, respectively).
Discussion
In our study, the use of bDMARD was associated with a shorter period of articular symptoms after Chikungunya fever infections as compared with patients using exclusively csDMARDs. However, we did not observe a statistically significant difference in the maximum severity of articular symptoms between these groups.Further we also did not observe a significant difference in the prevalence of positive IgG for CHIKV according to the use or not of biological agents, however seropositivity tended to be more prevalent among patients exclusively on csDMARDs (57.4%) comparing with patients on biologics (39.7%). It is possible that the use of bDMARDs may blunt the serologic response to CHIKV. Interestingly, we observed a higher prevalence of positive serology than previously reported in the general population (27%) and in rheumatic patients on treatment with biologics (25%) in the city of Recife in 2016–17 [9]. This observation may possibly reflect the now endemic nature of the disease, with more individuals becoming seropositive over time. As a matter of fact, the overall prevalence of seropositivity for CHIKV in our sample was numerically higher than that observed in the general healthy population in Reunion Islands (38.2%, 2005–6) [15], Ethiopia (43.6%, 2018) [16], and Zambia (36.9%, 2016) [17].
The CHIK symptoms are very typical and include fever and an intense and abrupt onset of joint pain [2], and cases occur generally in the context of an epidemiological outbreak. In the course of RA, ankylosing spondylitis (AS) and psoriatic arthritis (PsoA), disease flares are usually not accompanied by fever and joint symptoms usually occur in the same joints previously afflicted. In our study, CHIK-related symptoms were reported to affect joints unusually affected by the rheumatic disease (e.g., lumbar or dorsal pain was reported by 57.1% of RA patients). As in other studies [9, 10, 18], we did not find more severe symptoms or post-infectious complications of CHIK in patients using biological therapies. However, as our study is a survey of surviving patients, the results must be interpreted cautiously due to the possibility of selection bias.
There are few studies evaluating changes in articular symptoms caused by CHIKV infection in rheumatic patients using bDMARDs, although no previous study could adequately compare these patients with those exclusively on csDMARDs. Bautista-Vargas et al. followed 6 RA patients who had CHIK [18], 3 of them using a bDMARD (etanercept). No patient developed extra-articular manifestations, but all of them increased the usual dose of corticosteroids and 4 patients needed to switch or initiate biological therapy or jak inhibitor within 6 months due to worsening arthritis [18]. de Brito et al. (2016–17, Recife) also evaluated serology (IgG) for CHIKV in 186 patients with autoimmune inflammatory diseases (RA, AS or PsoA) on treatment with bDMARDs, and compared this group with 56 healthy people living in the same household as the patients [9]. There were 32 confirmed cases of CHIK (positive serology plus symptoms) among patients and 14 among controls. Persistence of musculoskeletal symptoms for more than 3 months post-CHIK occurred in 64% of controls and in only 28% of patients using bDMARDs (p = 0.021), especially anti-TNF agents [9]. Another study by Rosario et al. described 53 cases of CHIK in RA patients on biological therapy (monotherapy or in association with csDMARDs) [10]. In these patients, polyarthralgia occurred in 96.2% and arthritis was present in 47%; however, there was no difference in symptoms when this group was compared to patients with CHIK without concomitant rheumatic disease [10]. Patients were followed-up over 10 months and, during this period, therapy with csDMARD or bDMARD did not need to be modified in any patient and no complications occurred [10], corroborating data from our study on more favorable post-CHIK evolution in users of bDMARDs. In our study, articular symptoms during CHIKV infection were not significantly different in patients regardless of the use of bDMARDs. However, patients on biologics experienced faster recovery from joint symptoms and fewer treatment switches, even after stratification for possible confounding factors.
Although we found 16.5% of IgM positive serology for CHIKV in our sample (collected approximately one year after a reported CHIK fever episode), we found no association between positive IgM and longer duration of joint symptoms or any other symptom. Other studies have found similar results. A cohort study in Reunion Islands, evaluating healthy subjects after acute Chikungunya infection, demonstrated that 39.7% of the individuals maintained a positive result for IgM antibodies after 18 months with no association with persistent joint symptoms [19]. Other studies have also demonstrated persistence of positive serum IgM in 17% to 19% [20, 21] of healthy subjects for up to 12 months; however, the clinical relevance of this finding could not be determined.
Of note, this is the first study to compare the symptoms and clinical course of CHIK between rheumatic patients treated and not treated with biological therapy. The main limitation of our study is the retrospective design, possibly leading to recall bias, in which some participants might not have remembered some symptoms. On the other hand, all patients are prospectively followed up long before the CHIK outbreak and drug changes and serious adverse events are systematically monitored by the investigation center and the study's central coordination, limiting the possibility of bias. The number of confirmed cases of CHIKV infection (n = 32) was small, and our study may be underpowered for some analysis. Few patients received non-anti-TNF biologics, and so separate analysis according to class of bDMARD was not possible.
Conclusions
In conclusion, the data from our study suggest that the use of bDMARDs is associated with faster recovery from joint symptoms and lower risk of treatment switch among rheumatic patients infected with CHIKV.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CHIKV:
-
Chikungunya virus
- CHIK:
-
Chikungunya fever
- csDMARDs:
-
Conventional synthetic disease-modifying anti-rheumatic drugs
- bDMARDs:
-
Biological disease-modifying anti-rheumatic drugs
- tsDMARD:
-
Targeted synthetic disease-modifying anti-rheumatic drugs
- ELISA:
-
Enzyme-linked immunosorbent assay
- UFPE:
-
Universidade Federal de Pernambuco
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- RA:
-
Rheumatoid arthritis
- AS:
-
Ankylosing spondylitis
- PsoA:
-
Psoriatic arthritis
References
Lopes Marques CD, Ranzolin A, Cavalcanti NG, et al. Arboviruses related with chronic musculoskeletal symptoms. Best Pract Res Clin Rheumatol. 2020;34(4): 101502.
Weaver SC, Lecuit M. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med. 2015;372(13):1231–9.
El-Tallawy SN, Nalamasu R, Salem GI, et al. Management of musculoskeletal pain: an update with emphasis on chronic musculoskeletal pain. Pain Ther. 2021;10(1):181–209.
Runowska M, Majewski D, Niklas K, et al. Chikungunya virus: a rheumatologist’s perspective. Clin Exp Rheumatol. 2018;36(3):494–501.
Paixão ES, Rodrigues LC, Costa MCN, et al. Chikungunya chronic disease: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2018;112(7):301–16.
Sissoko D, Malvy D, Ezzedine K, et al. Post-epidemic chikungunya disease on Reunion Island: course of rheumatic manifestations and associated factors over a 15-month period. PLoS Negl Trop Dis. 2009;3(3): e389.
Schilte C, Staikowsky F, Staikovsky F, et al. Chikungunya virus-associated long-term arthralgia: a 36-month prospective longitudinal study. PLoS Negl Trop Dis. 2013;7(3): e2137.
Fernández-Ruiz M, Meije Y, Manuel O, et al. ESCMID study group for infections in compromised hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (Introduction). Clin Microbiol Infect. 2018;24(Suppl 2):S2–9.
de Brito CAA, Marques CDL, França RFO, et al. Reduced duration of postchikungunya musculoskeletal pain in rheumatological patients treated with biologicals. J Trop Med. 2020;2020:2071325.
Rosario V, Munoz-Louis R, Valdez T, et al. Chikungunya infection in the general population and in patients with rheumatoid arthritis on biological therapy. Clin Rheumatol. 2015;34(7):1285–7.
Titton DC, Silveira IG, Louzada-Junior P, et al. Brazilian biologic registry: biobadabrasil implementation process and preliminary results. Rev Bras Reumatol. 2011;51(2):152–60.
Ministério da Saúde do Brasil. Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a Semana Epidemiológica 52, 2016. 2017. Available at: https://antigo.saude.gov.br/images/pdf/2017/fevereiro/05/2017_002-Dengue%20SE52_corrigido.pdf
Marques CDL, Duarte ALBP, Ranzolin A, et al. Recommendations of the Brazilian society of rheumatology for diagnosis and treatment of Chikungunya fever part 1 - diagnosis and special situations. Rev Bras Reumatol Engl Ed. 2017;57(Suppl 2):421–37.
Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;140:1–55.
Gérardin P, Guernier V, Perrau J, et al. Estimating chikungunya prevalence in La Réunion Island outbreak by serosurveys: two methods for two critical times of the epidemic. BMC Infect Dis. 2008;8:99.
Endale A, Michlmayr D, Abegaz WE, et al. Community-based sero-prevalence of chikungunya and yellow fever in the South Omo Valley of Southern Ethiopia. PLoS Negl Trop Dis. 2020;14(9): e0008549.
Chisenga CC, Bosomprah S, Musukuma K, et al. Sero-prevalence of arthropod-borne viral infections among Lukanga swamp residents in Zambia. PLoS ONE. 2020;15(7): e0235322.
Bautista-Vargas M, Puerta-Sarmiento G, Cañas CA. Characteristics of Chikungunya virus infection in patients with established rheumatoid arthritis. Clin Rheumatol. 2020;39(12):3639–42.
Borgherini G, Poubeau P, Jossaume A, et al. Persistent arthralgia associated with chikungunya virus: a study of 88 adult patients on reunion island. Clin Infect Dis. 2008;47(4):469–75.
Chelluboina S, Robin S, Aswathyraj S, et al. Persistence of antibody response in chikungunya. Virusdisease. 2019;30(3):469–73.
Pierro A, Rossini G, Gaibani P, et al. Persistence of anti-chikungunya virus-specific antibodies in a cohort of patients followed from the acute phase of infection after the 2007 outbreak in Italy. New Microbes New Infect. 2015;7:23–5.
Acknowledgements
Not applicable
Funding
This study was supported by grants from the Brazilian Society of Rheumatology.
Author information
Authors and Affiliations
Contributions
AR was responsible for submitting ethic procedures, collecting and prepare the data, literature review and write the article; CM helped to write the article; LR collected data, helped to write the article and revised the English grammar; AD helped to write the article; HL collected the clinic data of patients; LM collected the clinic data of patients; AA performed the blood collection and serologic test procedures; PO performed the blood collection and serologic test procedures; MR supervised the serologic test procedures; MP supervised the serologic test procedures; MB analyzed and interpreted the data and was a major contributor in the writing the manuscript; IL helped to write the article. All authors read and approved by the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from each subject and all experimental procedures were approved by the Universidade Federal de Pernambuco ethics committee (certificate of ethical approval [CAAE] number 54275516.9.1001.5208).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. There is no relevant information to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ranzolin, A., Marques, C.D.L., da Rocha Junior, L.F. et al. Treatment with biological therapy is associated with faster recovery and lower frequency of treatment switch among rheumatic patients with Chikungunya fever. Adv Rheumatol 62, 44 (2022). https://doi.org/10.1186/s42358-022-00273-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-022-00273-0