Abstract
Background
Splenic artery aneurysms are rare and usually asymptomatic, with a high risk of mortality once they get ruptured. This is a rare case of a spontaneous splenic artery aneurysm rupture in a high-risk patient for surgery. Endovascular treatment was the only option to save patient’s life.
Case presentation
We report a 70-year-old woman with multiple comorbidities, presenting to the emergency department with signs of shock: confusion, pallor, tachycardia, and hypotension. Computed tomography shows an active bleeding from a splenic artery aneurysm rupture. The patient was successfully submitted to emergent arterial embolization of the splenic artery aneurysm.
Conclusions
Endovascular treatment is a less aggressive approach and should be considered in high-risk patients for surgical intervention. Rupture of a splenic aneurysm is a rare condition with high mortality rate and should be considered as a differential diagnosis in a patient with abdominal pain and hemodynamic instability.
Similar content being viewed by others
Background
Splenic artery aneurysm (SAA) is a rare pathology with an approximate prevalence of 1% within the general population and typically present in the sixth or seventh decade of life (Anand et al. 2022; Abdulrahman et al. 2014). It is the third most common arterial aneurysms, only exceeded by aneurysms in the abdominal aorta and iliac arteries. Diameters can range from 0.6 to 30 cm (Hosseinzadeh et al. 2022), and it is four times more common in females (Al-Habbal et al. 2010).
The pathogenesis is not fully understood, but identified risk factors encompass fibromuscular dysplasia, collagen vascular diseases, female gender, a history of multiple pregnancies, and portal hypertension (Al-Habbal et al. 2010). Typically asymptomatic, only 20% of them have symptoms such as abdominal pain and most are diagnosed incidentally (Abdulrahman et al. 2014). However, when rupture, they can precipitate a catastrophic presentation marked by intraperitoneal hemorrhage and hypovolemic shock, carrying a high mortality rate (25–75%) (Anand et al. 2022; Pararas et al. 2020).
A rare presentation occurs with the double-rupture phenomena. The first hemorrhage is contained by the lesser omental sac, leading to temporary tamponade, and the patient remains stable with minimal clinical symptoms. After 6–96 h, the blood overflows into the peritoneal cavity through the foramen of Winslow with resultant severe shock (Al-Habbal et al. 2010).
We described an unusual case of a rupture of a splenic artery aneurysm with active bleeding, manifesting as a retroperitoneal hematoma and hemorrhagic shock. Given the patient's high surgical risk profile, an endovascular approach was deemed optimal and was executed successfully.
Case presentation
A 70-year-old female, with a medical history comprising dementia, diabetes, hypertension, and heart disease, presented to the emergency department exhibiting symptoms of prostration, asthenia, and palpitations escalating over a two-day period. No antecedent history of blood loss or trauma was reported.
On admission, the patient presented with signs of shock: confusion, pallor, tachycardia (heart rate of 110–140 beats/min), and hypotension (blood pressure of 75/40 mmHg).
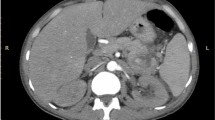
The laboratory work-up showed anemia 3.30 g/dL, INR 1.4, necessitating immediate massive transfusion. Arterial phase abdominal CT imaging revealed a voluminous retroperitoneal hematoma measuring 90 × 136 mm, disclosing active bleeding from a ruptured splenic artery aneurysm (Fig. 1).
Given the patient’s comorbidities and hemodynamic instability, a collaborative discussion involving surgical, anesthesiology, and intensive care teams concluded that the patient was a high-risk candidate for surgical intervention. Consequently, an emergent endovascular arterial embolization of the splenic artery aneurysm was pursued. The procedure concluded without complications, and the patient was transferred to the ICU for overall support, where she remained for 5 days. Afterward she was moved to the general ward to complement surveillance and was discharge from the hospital after several days, stable and without the need for invasive procedures.
There were no complications after one year of follow-up.
Discussion
SAA, initially described in 1770 by Beaussier in autopsies, gained recognition for preoperative diagnosis in 1920 by Hoegler, followed by the first documented surgical intervention in 1940 (Al-Habbal et al. 2010). Approximately 80% of SAA cases remain asymptomatic, typically incidentally discovered during imaging investigations (Al-Habbal et al. 2010). Manifestations, if present, tend to be nonspecific, often involving epigastric and left-upper quadrant abdominal pain (Pararas et al. 2020).
Rupture, reported in 3 to 10% of all splenic aneurysms, can induce a dramatic hypotensive shock with a notable mortality rate (Pararas et al. 2020; Berceli 2005). Rupture risk correlates with factors such as aneurysm size, pregnancy, cirrhosis, and liver transplantation, with an aneurysm exceeding 2 cm in diameter considered predisposed to rupture (Anand et al. 2022; Berceli 2005). This patient only has female sex as a risk factor.
Elective treatment is indicated for all symptomatic splenic artery aneurysms, regardless of their dimensions (Akbulut and Otan 2015). Treatment is also recommended for lesions ≥ 2 cm, growing aneurysms, all pregnant or fertile woman, patients with portal hypertension or candidates for liver transplantation (Kaszynski and Hasiura 1999).
When rupture, endovascular treatment emerges as a less aggressive yet effective approach, particularly in high-risk patients unsuitable for surgical management (Abbas et al. 2002; Papadomichelakis et al. 2014). The successful management of this case underscores the imperative nature of prompt diagnosis and intervention to avert life-threatening outcomes.
Conclusions
Splenic aneurysms are a rare condition, and most of the times are asymptomatic but have a high risk of mortality when ruptures.
This clinical instance serves as a testament to the criticality of immediate diagnosis and treatment in salvaging a patient's life, especially in scenarios where conventional surgical interventions pose substantial risks to individuals with multiple comorbidities.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SAA:
-
Splenic artery aneurysm
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- Fig.:
-
Figure
References
Abbas MA et al (2002) Splenic artery aneurysms: two decades experience at Mayo Clinic. Ann Vasc Surg 16(4):442–449. https://doi.org/10.1007/s10016-001-0207-4
Abdulrahman A, Shabkah A, Hassanain M, Aljiffry M (2014) Ruptured spontaneous splenic artery aneurysm: a case report and review of the literature. Int J Surg Case Rep 5(10):754–757. https://doi.org/10.1016/j.ijscr.2014.08.021
Akbulut S, Otan E (2015) Management of giant splenic artery aneurysm. Medicine 94(27):e1016. https://doi.org/10.1097/MD.0000000000001016
Al-Habbal Y, Christophi C, Muralidharan V (2010) Aneurysms of the splenic artery: a review. Surgeon 8(4):223–231. https://doi.org/10.1016/j.surge.2009.11.011
Anand A, Khurana S, Ateriya N, Sunil Kumar Sharma GA (2022) Sudden death due to non-traumatic rupture of splenic artery aneurysm. Med Leg J 90(2):76–78. https://doi.org/10.1177/00258172211018339
Berceli SA (2005) Hepatic and splenic artery aneurysms. Semin Vasc Surg 18(4):196–201. https://doi.org/10.1053/j.semvascsurg.2005.09.005
Hosseinzadeh A, Shahriarirad R, Asgharzadeh Majdazar V, Moeini Farsani M, Tadayon SMK (2022) Spontaneous rupture of a large splenic artery aneurysm in a 59-year-old male patient with pemphigus vulgaris: a case report. J Med Case Rep 16(1):1–5. https://doi.org/10.1186/s13256-022-03618-x
Kaszynski M, Hasiura R (1999) Splenic artery aneurysm: case report. Med Sci Monit 5(6):1213–1215. https://doi.org/10.5402/2011/383450
Papadomichelakis A, Anyfantakis D, Kastanakis M, Karona P, Bobolakis E (2014) Rupture of a splenic artery aneurysm in a previously healthy 53-year-old male. J Med Life 7(2):69–70
Pararas N, Rajendiran S, Taha I, Powar RR, Holguera C, Tadros E (2020) Spontaneous rupture of a huge splenic artery aneurysm: a case report. Am J Case Rep 25(21):e919956. https://doi.org/10.12659/AJCR.919956
Acknowledgements
Not applicable.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent to publish obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carvalho, M., Mendes, J., Macedo-Oliveira, C. et al. Endovascular treatment of splenic artery aneurysm rupture: case report. Bull Natl Res Cent 48, 9 (2024). https://doi.org/10.1186/s42269-024-01165-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-024-01165-7