Abstract
Background
Partial aorta detachment is a rare and fatal complication of mechanical chest compression.
Case presentation
The paper describes a patient in cardiac arrest who died despite receiving CPR using mechanical chest compression. After death, an autopsy showed the presence of a partial rupture of the aortic wall in the intra-pericardial section.
Discussion
In the discussion, for this case, we propose to deepen our knowledge of post-resuscitation complications, which may help to understand the need to maintain the recommended parameters of chest compressions, respond more confidently to changes in the patient's condition during CPR, to interpret the results of bedside examinations better, and to understand the autopsy results better. In our opinion, the best method of diagnosing internal injuries, which we provide with Point-of-Care (POCUS) ultrasound, allows for therapeutic interventions that maximize the chances of spontaneous circulation. Education and skill development are also indispensable aspects of CPR. Particular attention should be paid to the same quality of chest compressions performed.
Conclusions
As conclusions drawn from the analysis of this case, we propose paying particular attention to the difficulty of explaining changes in the patient's condition during CPR, the widespread use of POCUS, and considering the use of compressions performed by staff in situations where it is possible and safe.
Similar content being viewed by others
Background
Effective chest compressions are the most crucial during cardiopulmonary resuscitation (CPR) and should be provided to all patients with cardiac arrest. Its quality impacts patient prognosis (European Resuscitation Council Guidelines 2021). Even technically executed, chest compressions may cause iatrogenic injuries to the airways, chest, and abdomen. The most common injuries are rib (13–97%) and sternal fractures (1–43%) (Hoke and Chamberlain 2004). Broken bones can secondarily damage internal organs, significantly reducing return of spontaneous circulation (ROSC) and even leading to death (Sokolove et al. 2002). Peri- or post-resuscitation recognition of iatrogenic injury allows implementation of dedicated treatment procedures and maximizes the chances of long-term spontaneous circulation.
We report a patient with severe, rare, and fatal CPR complications and discuss diagnosing, treating, and interpreting peri-resuscitation injuries. During CPR performed by the bystander, EMS, and ED team, partial detachment of the heart from the aorta and bleeding into the left pleural cavity occurred. The diagnosis was confirmed postmortem in the autopsy.
Increasing knowledge of peri-resuscitation (resuscitation-related) complications will help understand the need to maintain recommended chest compression parameters (European Resuscitation Council Guidelines 2021), respond more confidently to changes in patient status during CPR, better interpret bedside findings, and better understand autopsy findings.
Case presentation
A 53-year-old male with a sudden loss of consciousness. Witnesses called EMS and performed CPR for 5 min until EMS arrived. After the arrival of EMS (“S” type ambulance—with a physician), PEA cardiac arrest was diagnosed. Manual chest compressions were continued, the patient was intubated and mechanically ventilated, and epinephrine was administered every 3–5 min (8 mg total). Due to the lack of effect and the young age of the patient, after 20 min, he was transported to the hospital. Manual CPR was performed during transportation and continued in the Emergency Department (ED) for 30 min. In the hospital, point-of-care ultrasound (POCUS) was performed by a physician without interruption of cardiopulmonary resuscitation. POCUS showed no spontaneous contractility of the heart, a trace of fluid in the pericardial sac, and no liquid in the peritoneal cavity. Rhythm conversion from PEA to asystole was observed, and death was declared. The chest was compressed in total for approximately 55 min. Mechanical chest compression devices were not used. The patient had a postmortem examination.
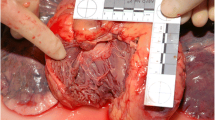
The autopsy showed: skin abrasions of the chest, multiple fractures of all left ribs, right ribs II–VI, sternal fracture, 1.5 cm laceration of the pericardial sac, partial aortic detachment from the valve with uneven edges for a 2-cm length without aneurysmal changes and 3.600 ml of blood in the left pleural cavity. The cause of death was massive internal bleeding from the heart's severed arterial and venous vessels with concomitant macroscopic and microscopic features of myocardial ischemia. External injuries were not fatal, and internal injuries were considered iatrogenic.
In this case, manual chest compressions resulted in a flail chest (multiple bilateral rib and sternal fractures) with a subtotal detachment of the aorta from the heart with pericardial disruption and hemorrhage into the left pleural cavity. The severity of the injuries related to the autopsy report is evidenced by the deposition of bleeding present in the walls of the aorta. These current blood infiltrations described in the intercostal muscles and thoracic vessels correspond to their position relative to the force acting on the anterior chest wall and correlate with how chest compressions are performed. It is important to remember that described injuries were caused by a forceful blow (possibly pressure) from a rigid or flexible instrument, maybe human hands. The microscopic examination of the aortic wall did not reveal any pathology that could weaken the vessel wall.
Discussion
Numerous peri-resuscitation injuries have been described, including aortic injuries (Waqar et al. 2022). However, with the development of CPR standards, serious injuries are decreasing. The extensive injuries in the related case led the authors to review the literature and search for causes of cardiac arrest and iatrogenic complications during CPR.
Postmortem
Post-mortem examination must be complemented by a review of the deceased’s medical history, which can assist in avoiding misinterpretation of the autopsy findings. In the described case, an uncommon CPR complication occurred. If past medical history and circumstances of death were unknown, one could erroneously interpret the autopsy findings. It is known that aortic injury may occur in 34% of passengers in lethal car crashes (Szeremeta et al. 2007). The goal of correctly interpreting injuries and lesions dates back to forensic medicine. Thus, cooperation between clinicians and forensic specialists is instrumental in correctly interpreting the autopsy findings, requiring interdisciplinary medical knowledge and a broader view of the findings (Ambade et al. 2021).
Ultrasonography
We reviewed recent evidence on Point-of-Care Ultrasound (POCUS) in both pre-hospital and emergency departments. Advantages of POCUS include being non-invasive, not requiring transporting the patient outside ED, and not mandating require interruption of chest compressions. The use of Point-of-Care Ultrasound POCUS provides the opportunity to identify peri-resuscitation injuries and prompt treatment interventions that maximize the chances of survival (Bendinelli et al. 2012). Studies have shown POCUS to be positive in up to 29% of cases (Konesky and Guo 2018). According to many authors, POCUS has a rapid learning curve and should be used obligatorily in emergencies such as the acute abdomen, sudden cardiac arrest, and acute obstetric conditions in the ED and the pre-hospital (Arnold and Jonas 2020).
Transesophageal Echocardiography (TEE) could be considered to increase the effectiveness of peri-resuscitation ultrasound diagnoses. Some authors have proposed its inclusion in diagnostic algorithms in SCA (sudden cardiac arrest) (Dissection of the thoracic aorta following cardiopulmonary resuscitation Article in Critical ultrasound journal 2011). Transesophageal Echocardiography TEE is reliable and has a high sensitivity (97%). Critical therapeutic decisions can be made for the patient based on positive results (Kim et al. 2021).
Post-resuscitation care
Peri-resuscitation injuries should also be considered in patients who present with hemodynamic instability and rapidly deteriorate after successful resuscitation during post-resuscitation care. Heart, lungs, and aorta injuries can be treated during CPR by performing an emergency thoracotomy, switching to open cardiac compressions, and surgically managing injuries. This could be has been considered in the described case (Liu et al. 2022). The authors suggest performing the first ultrasound assessment as early as possible during resuscitation and repeating it systematically to differentiate peri- and pre-resuscitation injuries.
Education/quality monitoring
Education and skills development are an indispensable aspect of CPR. It is essential to pay particular attention to the exceptional quality of the chest compressions delivered. Increasing their depth results in more frequent iatrogenic peri-resuscitation injuries (Hellevuo et al. 2013). Studies also show a significant role of the incorrect position of the hands on the chest (Natsuaki et al. 2010); too much force applied leads to more frequent fractures of the ribs and sternum, which leads to secondary Injuries to thoracic organs and vessels (Usawasuraiin et al. 2022). It is recommended to use devices that monitor the quality of chest compressions (Gugelmin-Almeida et al. 2021).
The authors suggest increasing the training in simulated settings addressing the technical aspects of chest compressions, emphasizing their effectiveness and safety (Toft et al. 2022) and the enormous potential benefits. This is, especially important in light of current guidelines that suggest manual chest compressions over mechanical chest compression devices (European Resuscitation Council Guideline 2021).
Mechanical compressions
Through further training and improvement of their skills, the resuscitation practitioner can provide more effective, precise resuscitation and thus reduce the risk of iatrogenic peri-resuscitation complications. Of note, the injuries and subsequent deaths described in this case are reported with mechanical devices, e.g. LUCAS©, Cardiopump© (Alexander et al. 2021). Studies indicate that peri-resuscitation complications—both related to soft tissue and bony injuries—are far more familiar with mechanical devices than with manual compression (Friberg et al. 2019; Ram et al. 2018).
Sternum fractures are as high as 81–93% and rib fractures 81–86% (Ram et al. 2018) with Cardiopump©. For LUCAS©, up to 79% of patients suffer a rib fracture, compared with 65% for manual compressions. Sternal fracture estimates are similar (Friberg et al. 2019). Furthermore, the PaRAMeDic study of 4471 patients showed no improvement in 30-day survival in patients treated with LUCAS©—in addition, 3-month survival without neurological damage was lower in this group (Ram et al. 2018).
We hypothesize that the latter may be due to the inability of machines to "adjust" to the patient's chest compliance and the inability to control the force and depth of compressions consistently. It is also important to remember that the duration of the CPR is a risk factor for iatrogenic injuries—and the European Resuscitation Council Guidelines 2021 that mechanical devices should only be used as a reasonable alternative to high-quality manual compressions. One such justification may be staff fatigue, a threat to their safety, or the need to transport the patient resulting in an increased duration of resuscitation (European Resuscitation Council Guidelines 2021).
Conclusions
The described case is not isolated. Peri-resuscitation injuries, including severe ones, occur frequently. The Department of Forensic Medicine in autopsy materials have identified numerous peri-resuscitation iatrogenic injuries, but so far, no such case has been encountered. The authors speculate that the manner and quality of chest compressions was the most critical factor, including hand placement, depth of compressions, and keeping the hands on the chest between contractions. Iatrogenic injuries occur more frequently with mechanical chest compression devices (Sokolove et al. 2002). Regardless, the resuscitator should pay attention to CPR-related injuries in the differential diagnosis of reversible causes of cardiac arrest, assisted by Point-of-Care Ultrasound or Transesophageal Echocardiography. For deteriorating, persistently unstable, or unresponsive patients, the presence of iatrogenic injuries should be considered, leading to possible treatment and increasing the chances of return of spontaneous circulation. Despite ideal resuscitation conditions, iatrogenic complications are presently inevitable. Any physician working with a resuscitated patient (including a forensic physician) should be aware of it.
Availability of data and materials
All data despite case data are public. The presented case comes from anonymized materials of Forensic Medicine Department of Poznan University of Medical Sciences.
Abbreviations
- CPR:
-
Cardiopulmonary resuscitation
- POCUS:
-
Point-of-care ultrasound
- ROSC:
-
Return of spontaneous circulation
- EMS:
-
Emergency medicine service
- ED:
-
Emergency Department
- PEA:
-
Pulseless electrical activity
- TEE:
-
Transesophageal echocardiography
- SCA:
-
Sudden cardiac arrest
- e.g.:
-
For example
References
Alexander E, Katharina T, Verena F, Jürgen G, Maximilian N, Calvin K, Andreas S, Wolfgang S, Harald H, Dominik R (2021) Comparison of different mechanical chest compression devices in the alpine rescue setting: a randomized triple crossover experiment. Scand J Trauma Resusc Emerg Med 29(1):84. https://doi.org/10.1186/s13049-021-00899-x
Ambade VN, Sirsat Kunal B, Manu S (2021) Pattern of injuries in different types of victims of road traffic accident in central India: a comparative study. J Forensic Sci Res 5:007–011
Arnold MJ, Jonas CE et al (2020) Point-of-care ultrasonography. Am Fam Phys 101(5):275–285
Bendinelli C, Easton R, Parr M (2012) Focused assessment with sonography for trauma (FAST) after successful cardiopulmonary resuscitation. Resuscitation 83:e17
Dissection of the thoracic aorta following cardiopulmonary resuscitation Article in Critical ultrasound journal (2011). https://doi.org/10.1007/s13089-011-0056-5
European Resuscitation Council Guidelines 2021: Adult advanced life support
Friberg N, Schmidbauer S, Walther C, Englund E (2019) Skeletal and soft tissue injuries after manual and mechanical chest compressions. Eur Heart J Qual Care Clin Outcomes 5(3):259–265. https://doi.org/10.1093/ehjqcco/qcy062
Gugelmin-Almeida D, Tobase L, Polastri TF, Peres HHC, Timerman S (2021) Do automated real-time feedback devices improve CPR quality? A systematic review of literature. Resusc plus 27(6):1108. https://doi.org/10.1016/j.resplu.2021.100108
Hellevuo H, Sainio M, Nevalainen R et al (2013) Deeper chest compression—more complications for cardiac arrest patients? Resuscitation 84:760–765
Hoke RS, Chamberlain D (2004) Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation 63:327–338
Kim YW, Jung WJ, Cha KC, Roh YI, Kim YS, Kim OH, Cha YS, Kim H, Lee KH, Hwang SO (2021) Diagnosis of aortic dissection by transesophageal echocardiography during cardiopulmonary resuscitation. Am J Emerg Med 39:92–95. https://doi.org/10.1016/j.ajem.2020.01.026
Konesky KL, Guo WA (2018) Revisiting traumatic cardiac arrest: should CPR be initiated? Eur J Trauma Emerg Surg 44(6):903–908. https://doi.org/10.1007/s00068-017-0875-6
Liu A, Nguyen J, Ehrlich H, Bisbee C, Santiesteban L, Santos R, McKenney M, Elkbuli A (2022) Emergency resuscitative thoracotomy for civilian thoracic trauma in the field and emergency department settings: a systematic review and meta-analysis. J Surg Res 273:44–55. https://doi.org/10.1016/j.jss.2021.11.012
Natsuaki M, Yamasaki A, Morishige N, Nishimi M, Okabe M, Yamamoto Y (2010) Right ventricular rupture induced by cardiopulmonary resuscitation. J Cardiol Cases 1(1):e42–e44
Ram P, Menezes RG, Sirinvaravong N, Luis SA, Hussain SA, Madadin M, Lasrado S, Eiger G (2018) Breaking your heart-A review on CPR-related injuries. Am J Emerg Med 36(5):838–842. https://doi.org/10.1016/j.ajem.2017.12.063
Sokolove PE, Willis-Shore J, Panacek EA (2002) Exsanguination due to right ventricular rupture during closed-chest cardiopulmonary resuscitation. J Emerg Med 23:161–164
Szeremeta M, Dopierała T, Janica J, Niemcunowicz-Janica A, Załuski J, Ptaszyńska-Sarosiek I, Okłota M, Stepniewski W (2007) Analiza porównawcza ofiar wypadków komunikacyjnych w swietle materiału sekcyjnego Zakładu Medycyny Sadowej w Białymstoku w latach 1970–1986 oraz 1987–2006 [Comparative analysis of traffic accident fatalities in autopsy material of 1970–1986 and 1987–2006 collected at the Departament of Forensic Medicine Medical University of Białystok]. Ann Acad Med Stetin 53(Suppl 2):76–9. Polish. PMID: 20146417
Toft LEB, Richie J, Wright JM, Amraotkar A, Katrapati P, Fulmer S, Dainty KN, Chugh SS, Halperin H (2022) A new era of lay rescuer CPR training: an interactive approach for engaging high schoolers. J Am Coll Cardiol 80(23):2251–2253. https://doi.org/10.1016/j.jacc.2022.09.040
Usawasuraiin P, Wittayachamnankul B, Chenthanakij B, Euathrongchit J, Phinyo P, Tangsuwanaruk T (2022) Optimal landmark for chest compressions during cardiopulmonary resuscitation derived from a chest computed tomography in arms-down position. J Cardiovasc Dev Dis 9(4):100. https://doi.org/10.3390/jcdd9040100
Waqar A, Rajput F, Rachwan RJ, Abi-Saab T, Gimelli G (2022) LUCAS compression device-related severe injuries in a series of patients presenting with outside hospital cardiac arrest. J Cardiol Cases 26(6):432–435. https://doi.org/10.1016/j.jccase.2022.09.006
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BB and MS contributed to Conceptualization; MS, BB, KDK contributed to investigation; MS contributed to resources; MS, BB, KDK contributed to writing—original draft preparation, MS, KDK, BB contributed to writing—review and editing; ZŻ., CŻ contributed to supervison; ZŻ contributed to project administration. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szemień, M., Burchardt, B., Dolińska-Kaczmarek, K. et al. Partial detachment of the aorta: a fatal complication of CPR chest compressions. Bull Natl Res Cent 47, 57 (2023). https://doi.org/10.1186/s42269-023-01023-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-023-01023-y