Abstract
Background
Origanum majorana (O. majorana) is one of the most widely used herbs in Egypt due to its antioxidant, anti-inflammatory, anti-genotoxic, antimutagenic, anticoagulant and beneficial properties. Our study's main goal is to determine how well O. majorana leaf extract can reduce hepatotoxicity and oxidative stress produced by dexamethasone (DXM). Thirty female rats were divided into three groups of ten. Animals in group1 received distilled water daily for eight weeks and served as control. Those in group 2 exposed subcutaneously to 0.1 mg/kg body weight of DXM three times per week for eight weeks and served as the toxic group, while those in group 3 were treated daily and orally with 100 mg/kg of O. majorana aqueous extract + 0.1 mg/kg of DXM three times per week for eight weeks and served as treated group.
Results
Due to DXM treatment, the activities of liver function markers were significantly elevated (P < 0.0001), whereas O. majorana pretreated animals improved or reduced the elevated liver function enzyme activities. Dexamethasone administration considerably enhancing oxidative stress which rose (P < 0.0001) MDA concentration and attenuated the antioxidant defense system by decreasing the activities of GST, GSP, GSR, and CAT significantly in liver homogenate when compared to control animals. The results further demonstrated that pretreatment with O. majorana boosted the antioxidant defenses against the damaging effects of DXM.
Conclusion
It can be said that dexamethasone exposure induced- hepatotoxicity and oxidative stress in rats that repaired by O. majorana aqueous extract which had the ability to reduce the impact of hepatic damage. To evaluate the health benefits and safety of O. majorana in individuals, more clinical research is needed.
Graphical abstract

Similar content being viewed by others
Background
Metabolism is one of the liver main functions as it is responsible not only for protein, lipid and carbohydrate metabolism, but also drug and metabolite transformation and detoxification (Bastway et al. 2008; Rui 2014). Due to the harmful effect of drugs on the vital organs as liver, brain tissue, lung and heart, FDA decided to non-approval and withdrawal of it (Iorga et al. 2017). The liver also sensitive to toxicity and corticosteroids which alter the hepatocellular biological process and homeostasis (Hazra et al. 2008). Synthetic glucocorticoids (GCs) are used widely as anti-inflammatory drug, but it is inefficient in many tumor and auto- immune diseases (Coutinho and Chapman 2011). Although it is still doubtful, GCs used to treat many liver disorders. In spite of the beneficial effects of GCs as anti-inflammatory drug in cholestatic patients, it may attenuate the patient’s defenses against the harmful effects of biliary component buildup. Dexamethasone is a long-acting anti-inflammatory synthetic GC (Courtois et al. 1999; Kubitz et al. 1999; Turncliff et al. 2004). Dexamethasone overdose-induced hyperglycemia, hyperlipidemia, steatosis development, and fatty liver (Hasona et al. 2017; Yin et al. 2017). Dexamethasone damages DNA and causes oxidative stress to have an anti-cancer effect (Motafeghi et al. 2022). Malonaldialdehyde is known as oxidative stress marker increased according to dexamethasone toxicity. Oxidative stress defined as an unbalance between cellular defense mechanism and free radical production (Pascussi et al. 2000).
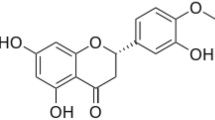
Herbal medicines have been used traditionally since the ancient times for treating many diseases by improving the immunity. It is used also as dietary supplement to promote health (Babich et al. 2020, Pelvan et al. 2022). Origanum majorana L. (O. majorana), an aromatic plant from the Lamiaceae family. O. majorana, which is frequently used as a spice or seasoning, has a variety of pharmacological activities, including hepatoprotective, antibacterial, anti-inflammatory, cardioprotective, anti-platelet, antiulcer, antitumor, gastroprotective, antimetastatic, antiatherosclerosis and antifungal, antiprotozoal and anticholinesterase inhibitory activities (Villalva et al. 2018; Arranz et al. 2019). O. majorana aerial component extracts in water, essential oil, and ethyl acetate have remarkable antioxidant activity (Triantaphyllou et al. 2001; Al-Howiriny et al. 2009; Hussain et al. 2011; Mossa and Nawwar 2011; Erenler et al. 2016). Other sweet O. majorana extracts, such as ethanolic, n-hexane, and hydroalcoholic extracts, have also been said to possess antioxidant effects (Vagi et al. 2005). The antioxidant effect is caused by phenolic compounds, such hydroxycinnamic acid and flavonoids, ursolic acid, carnosic acid, carnosol, rosmarinic acid, and caffeic acid (Triantaphyllou et al. 2001; Heo et al. 2002; Vagi et al. 2005; Hossain et al. 2014). The most frequent flavonoids found in sweet O. majorana are hesperetin, catechin, quercetin, kaempferol, naringenine, eriodictyol, diosmetin, luteolin, and apigenin. Flavonoid glycosides identified in sweet O. majorana include kaempferol-3-O-glucoside, quercetin-3-O-glucoside, narigenin-O-hexoside, and rutin (Al-Howiriny et al. 2009; Kozlowska et al. 2010; Queralt et al. 2015). When compared to the lead acetate-treated group, O. majorana alcoholic, aqueous, and essential oil extracts and essential oil significantly improved kidney and liver histology while lowering serum urea and creatinine levels and serum liver enzyme activities (El-Ashmawy et al. 2005). Cadmium altered lipid peroxidation levels may be successfully enhanced or decreased by O. majorana extract, which has protective and therapeutic properties that lessen the kidney and liver antioxidant activities against toxicities brought on by cadmium (Shati 2011).
Therefore, the current study's designed to study O. majorana protective role against hepatotoxicity and other harmful effects during dexamethasone treatment by boosting the immune system through the antioxidant defense mechanism, consequently attenuating oxidative stress and restoring the hepatocellular biomarkers toward normal in albino rats.
Methods
Study animals
30 female Wistar rats from the Giza, Egypt-based from Ophthalmology Research Center animal house, weighing between 120 and 150 g were used in the study. They were kept for 14 days under observation in conventional cages with access to food and cool, room-temperature water. The regular 12:12 h light–dark cycles were likewise maintained for them. The National Institutes of Health (NIH) and Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) criteria for the handling and use of experimental animals were followed in all animal operations. All experiments were performed in line with the ethical guidelines approved by the Medical Research Ethics Committee of the National Research Centre, El Dokki, Egypt of Experimental Animals (No. 20286).
Chemicals
In Egyptian Tec Pharmaeutical industries, dexamethasone was purchased from Sigma—S. A. E.
Plant materials
The Sekem Co. provided the Egyptian sweet O. majorana leaves for the medicinal plant (Cairo, Egypt). An ecologist (Dr. Kaled Elsayed, assistant professor) from the Plant Biotechnology, Botany Department, Faculty of Science, Beni- Suef University, Egypt, identified the plant material used in the current study and deposited a voucher specimen in a public herbarium.
Origanum majorana L. aqueous extract preparation
Ramadan et al. (2012) technique states that to make O. majorana leaf aqueous extract, 100 mg/kg of body weight of the herb was dissolved in 0.5 ml of boiling distilled water (equal to three cups of O. majorana tea, respectively), covered and allowed to stand for 10 min at room temperature. The extract was then filtered and administered to the animals immediately.
Doses and treatment
To include an increase in the frequency of hepatotoxicity and oxidative stress, dexamethasone (DXM) was previously reported in mammalian systems (Feng et al. 2013). Subcutaneously and for eight weeks (three doses weekly), 0.1 mg/kg DXM dose was dissolved in sterilized water. In our study O. majorana dose were adjusted to 100 mg/kg b.wt. for 8 weeks (Ramadan et al. 2012).
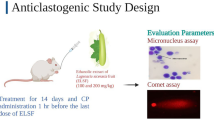
Study design
Three groups (ten animals each) were divided into three groups (Fig. 1):
-
1.
Group 1: Rats received distilled water daily for eight weeks and served as control.
-
2.
Group 2: Rats received DXM subcutaneously three doses weekly (0.1 mg per kilogram of body weight) for eight weeks (Feng et al. 2013) and served as toxic group.
-
3.
Group 3: Rats received subcutaneously 0.1 mg/kg. b. wt. of dexamethasone three times per week together with 100 mg/kg body weight O. majorana aqueous extract (orally) for eight weeks (Ramadan et al. 2012) and served as treated group.
Sampling
In the morning, at the end of the experiment and under light ether anesthesia. Animals were sacrificed by cervical decapitation; 5 ml of blood were collected from the jugular vein (Lucas et al. 2004), then centrifuged for 15 minutes to separate serum and kept frozen at −20 °C for biochemical analyses.
Liver marker enzymes
Regarding Rosalki et al. (1993), serum alkaline phosphatase (ALP) was kinetically estimated. Lactate dehydrogenase (LDH) kit was bought from Stanbio Laboratories in Texas, USA, and estimated using the Buhl and Jackson (1978) method. Reitman and Frankel (1957) methods were used to measure serum alanine transferase (ALT) and aspartate aminotransferase (AST) activity using kits supplied from Biodiagnostic (Egypt).
Hepatic antioxidant enzymes analyses and oxidative stress
Each animal’s liver was quickly sampled after dissection and cleaned in saline solution. 0.5 g of liver tissue was homogenized in 5 ml of saline solution using a Teflon tissue homogenizer. Measurements of antioxidant enzymes were performed using the clear supernatant. For the estimation of reduced glutathione (GSH) and lipid peroxidation (MDA) using Ohkawa et al. (1979) approach and Beutler et al. (1963). According to Paglia and Valentine (1967), the activity of the enzyme glutathione peroxidase (GPx) was estimated. The GST activity was measured using a technique developed by Habig et al. (1974). Glutathione reductase (GR) and catalase (CAT) activity were evaluated using the techniques developed by Goldberg and Spooner (1983) and Aebi (1984), respectively.
Histopathological study
Liver specimens were cleaned in saline solution and then kept in 10% formalin solution in accordance with the Banchroft et al. (1996) technique. Paraffin wax was used to compare the morphologies of liver tissues. After dehydration, 5- µm thick liver slices were deposited with hematoxylin and eosin (H& E).
Statistical analysis
Using graph Pad Prism 5 software, analyzed data were presented as mean ± SEM (San Diego, Calif., USA). Remarkable data were considered when P < 0.05. The statistical comparisons were made by ANOVA (one-way analysis of variance) according to Tukeye Kramer methods, post-hoc analysis.
Results
O. majorana alleviate Serum Liver Function Related Parameters in DXM treated rats
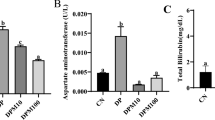
Table 1 illustrates liver damage which obviously appeared as a significant elevated activities (P < 0.0001) of circulating enzymes in serum (ALT, AST, ALP and LDH) after DXM treatment. Conversely, O. majorana pretreated animals successfully improved liver function markers which restored and/ or reduced these enzyme activities to normal level (Figs. 1, 2, 3, 4).
O. majorana prevents DXM-induced oxidative stress in rats
Table 2 clarifies that O. majorana pretreated group augmented the antioxidant defense system which elevated obviously (P < 0.0001) GSH level, CAT, GST, GPx plus GR activities in liver homogenate. In addition to that, O. majorana pretreatment suppressing oxidative stress by lowering lipid peroxidation (LPO) in comparison with DXM administered animals. When compared to the normal control group, DXM impaired the antioxidant defense system and decreased the activities of GSH, CAT, GST, GPx& GR. Also, DXM treated rats boosted the oxidative stress which raised LPO level remarkably (P < 0.0001) in liver homogenate when compared with the control levels (Figs. 5, 6, 7, 8, 9, 10, 11).
Histological study
Figure 12 demonstrates rat liver in normal control group that have no pathological variations. But, fatty change was detected all over the hepatocytes in the hepatic parenchyma (Fig. 12B) associated with dilatation in the central vein as well as the portal vein in dexamethasone treated group. O. majorana pretreated group showed edema and newly formed bile ductules in the portal area (Fig. 12C).
A Normal control rat liver transverse section presenting a central vein (CV), hepatic cords (h) and sinusoids in between. x 400. B In the hepatic parenchyma fatty change was detected all over the hepatocytes associated with the central and the portal veins dilatation in dexamethasone treated group. x 400 C Hepatocytes of O. majorana pretreated group showing edema (o) and newly formed bile ductules in the portal area. x 400
Discussion
The present work showed the hepatic damage in dexamethasone treated animals that was elicited by the elevated serum circulating enzymes (ALT, AST, ALP& LDH) activities obviously which ameliorated by O. marjorana pretreatment. These findings are in agreement with Hasona and Morsi (2019) who found that dexamethasone caused hepatotoxicity which elevated liver function activities significantly (ALT, AST& ALP). Increased liver marker enzymes were found in the serum of rats exposed to dexamethasone (Hasona et al. 2017). These enzymes' activities are sensitive indicators of hepatic damage and are directly correlated with the severity of the damage (Bastway et al. 2008). Generally, increased liver marker activities may reflect hepatocellular and bile canalicular destruction (Ha et al. 2001; Ahmed et al. 2014).
In the existing results, DXM also attenuated the immune system by increasing lipid peroxidation level remarkably and reducing the antioxidant defense markers significantly (GSH, GST, CAT, GPx & GR) and consequently confirmed by pathological disorders including fatty change all over the hepatocytes in the hepatic parenchyma, associated with dilatation in the central vein as well as the portal vein. O. marjorana boosted the immune system which enhanced the antioxidant defense system (elevated GSH, GST, CAT, GPx& GR) and attenuated the oxidative stress (reduced LPO). The current results are in agreement with Kamanli et al. (2004) who stated that corticosteroid therapy for liver damage causes increased liver function enzymes. DXM, which produces cell membrane oxidative damage leading to fatty liver alteration, may be responsible for increased inflammatory cell infiltration in the portal area, which is accompanied with liver injury. DXM-induced inflammatory cells infiltration, severe hepatocyte degeneration and necrosis (Safaei et al. 2012). Dexamethasone can severely altered hepatocytes function in long-term administered with high-dose as it is metabolized mainly in the hepatocytes via cytochrome P450 3A (Pascussi et al. 2001). Consequently, dexamethasone attenuates hepatocyte regeneration capacity after reducing hepatocyte proliferation activity which affected liver stored lipids and glycogen, subsequently leading to degeneration of glycogen and lipid in hepatocytes. Dexamethasone decreasing proliferation of liver cells to a lesser extent and apoptosis (Kimura et al. 2011). Concerning oxidative stress, the existing data coincided with Hasona et al. (2017) who stated that the principal cause of dexamethasone-induced liver injury is oxidative stress caused by the excessive production of free radicals. Dexamethasone significantly lowered the actions of entire antioxidant capacity as well as superoxide dismutase, resulting in oxidative stress by raising the volumes of peroxide hydrogen plus malondialdehyde (Miguel 2010). After exposure to dexamethasone, malondialdehyde levels in the plasma, liver and kidney were significantly elevated, indicating enhanced peroxidation and a breakdown of the antioxidant defense systems. The major cause of oxidative stress due to dexamethasone-induced liver injury is the free radicals excessive production (Airaodion et al. 2020).
Plants contain abundant phytochemicals with antioxidant which attenuated in vitro the agents of the oxidative stress (Iuchi et al. 2003). Antioxidants assist in preventing oxidation, which can harm cells and speed up aging. Antioxidants could improve immune response and lower the risk of cancer, heart disease, and infections. Foods include antioxidants in the form of vitamins, minerals, and other substances (Valko 2007). Increased MDA concentrations have been shown to decrease in the presence of antioxidants and phytochemicals (Airaodion et al. 2019a, b, c, d; Megwas et al. 2021). O. marjorana rich in flavonoids as quercetin, apigenin, naringenine, catechin, kaempferol, luteolin, eriodictyol, diosmetin, and hesperetin (Mossa et al. 2013, Villalva et al., 2018). Hydroxycinnamic acids and flavonoids, the watery extract of sweet O. majorana phenolic compounds have a significant ability in lipid oxidation slowing down (Triantaphyllou et al. 2001; El-Ashmawy et al. 2005). Ursolic acid from O. majorana decreased micromolar Abeta chance to enhanced oxidative cellular death (Heo et al. 2002). Quercetin and naringenine restored the liver function toward normal. Also, they offer protective effect on hepatocellular membrane against modifications or injury induced by diethylnitrosamine and acetylaminofluorene. These flavonoids might maintain hepatocytes by stabilizing membrane integral structures and thus prevent the release of these enzymes (Chen 2010; El-Denshary et al. 2015). The natural antioxidants protected the body from the dangerous chemicals known as free radicals (Devi et al. 2016). By the creation of reactive oxygen species, oxidative stress leads to the production of free radicals such as superoxide anions (O2−), hydrogen peroxide (H2O2), hydroxyl radicals (OH−), nitric oxide (NO), and organic hydroperoxide [(ROOH) (ROS)] (Aly and Duk 2016; Devi et al. 2016). The most prevalent soluble antioxidant, glutathione is present in all cell compartments (Airaodion et al. 2019a, b, c, d). Liver glutathione production and antioxidant defense are essential for effective detoxification procedures in response to metabolic stressors (Chen et al. 2020). In addition to playing a significant role in the metabolism of xenobiotics, glutathione directly quenches ROS such lipid peroxides. Glutathione plays a crucial function in the metabolism of xenobiotics and directly suppresses ROS such lipid peroxides (Ogbuagu et al. 2019). Glutathione detoxifies hydrogen peroxide and lipid peroxide by providing hydrogen peroxide an electron, converting it to water and oxygen, and protecting macromolecules from oxidation, such as lipids (Airaodion et al. 2019a, b, c, d). It is interesting to note that the biological system has been set up with natural enzymatic antioxidants like catalase, superoxide dismutase, and glutathione reductase to counteract the harmful effects of free radicals (Singh and Jambunathan 2017). Superoxide dismutase, catalase and glutathione-s-transferase maintaining the balance between ROS and antioxidant enzymes. Dismutation of superoxide anion (O2−) to H2O2 and O2 catalyzes by SOD. CAT catalyzes the decomposition of H2O2 to water because H2O2 is still harmful to cells and this mechanism is the important to avoid harm by oxidative stress (Al-Badr 2011). LPO had a significant effect to damage the cell membrane through altering its normal function (Fig. 13). An excess of reactive oxygen species was the source of an increase in oxidative stress (ROS). Consequently ROS have implicated in a number of disease processes, as liver injury, aging, diabetes, heart disease and cancer (Bokov et al. 2004, Giordano 2005, Mossa 2004, Mansour and Mossa 2010, Pelvana et al. 2022). Extreme doses of dexamethasone may increase the generation of free radicals, especially ROS. Free radicals cause cells to become more susceptible to apoptosis, mitochondrial malfunction, and permeability, which lower cellular energy production (Sato et al. 2010; Feng and Tang 2014).
Conclusions
Overall, the hepatotoxic effect of dexamethasone appeared clearly either by liver function markers elevation or antioxidant defense system attenuation as well as liver histological alterations. Origanum majorana L. (O. majorana) aqueous extract boosted the immune system, attenuated the oxidative stress and consequently protect the liver from the damaging effects induced by dexamethasone. To apply O. majorana as an important therapeutic strategy requires attention to assess its safety as well as benefits.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- DXM:
-
Dexamethasone
- GCs:
-
Glucocorticoids
- Cd:
-
Cadmium
- b.wt.:
-
Body weight
- ALP:
-
Alkaline phosphatase
- LDH:
-
Lactate dehydrogenase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- GSH:
-
Reduced glutathione
- MDA or LPO:
-
Lipid peroxidation
- GPx:
-
Glutathione peroxidase
- GST:
-
Glutathione-s-transferase
- GR:
-
Glutathione reductase
- CAT:
-
Catalase
- H& E:
-
Hematoxylin and eosin
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- SE:
-
Standard error
References
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Ahmed OM et al (2014) Preventive effect of Spirulina versicolor and Enteromorpha flexuosa ethanolic extracts against diethylnitrosamine/benzo (a) pyreneinduced hepatocarcinogenecity in rats. J Int Acad Res Multidiscipl 6(2):633–650
Airaodion AI, Akinmolayan JD, Ogbuagu EO, Esonu CE, Ogbuagu U (2019a) Preventive and therapeutic activities of methanolic extract of Talinum triangulare leaves against ethanol-induced oxidative stress in Wistar rats. Int J Bio-Sci Bio-Technol 11(7):85–96
Airaodion AI, Ogbuagu EO, Ekenjoku JA, Ogbuagu U, Airaodion EO (2019b) Therapeutic effect of methanolic extract of Telfairia occidentalis leaves against acute ethanol-induced oxidative stress in Wistar rats. Int J Bio-Sci Bio-Technol 11(7):179–189
Airaodion AI, Ogbuagu EO, Ewa O, Ogbuagu U, Awosanya OO, Adekale OA (2019c) Ameliorative efficacy of phytochemical content of Corchorus olitorius leaves against acute ethanol-induced oxidative stress in Wistar rats. Asian J Biochem Genet Mol Biol 2(2):1–10
Airaodion AI, Ogbuagu U, Ekenjoku JA, Ogbuagu EO, Airaodion EO, Okoroukwu VN (2019d) Hepato-protective efficiency of ethanol leaf extract of Moringa oleifera against hydrocarbon exposure. Int J Adv Herbal Alternat Med 3(1):32–41
Airaodion AI, Olawoyin DS, Alabi OJ, Atiba FA, Ogbuagu EO (2020) Air freshener induced oxidative stress and its adverse effects on immunity. Int J Health Saf Environ 6(05):579–587
Al-Badr NA (2011) Effect of thyme powder extract and oil on carbon tetrachloride-induced liver injury. J Am Sci 7:221–227
Al-Howiriny T, Alsheikh A, Alqasoumi S et al (2009) Protective effect of Origanum majorana L. ‘O. majorana’ on various models of gastric mucosal injury in rats. Am J Chin Med 37:531–545
Aly FI, Duk JA (2016) Hand book of legumes of world economic importance, vol 198. Plenum Press, New York, pp 14–25
Arranz E, Villalva MA, Guri E, Hernández O, Jaime L, Reglero G (2019) Corredig protein matrices ensure safe and functional delivery of rosmarinic acid from O. majorana (Origanum majorana) extracts. J Sci Food Agric 99:2629–2635
Babich O, Sukhikh S, Prosekov A, Asyakina L, Ivanova S (2020) Medicinal plants to strengthen immunity during a pandemic. Pharmaceuticals 13(10):313. https://doi.org/10.3390/ph13100313
Banchroft JD, Stevens A, Turner DR (1996) Theory and Practic of Histologixal Techniques, 4th edn. Churchil Livingstone, New York, London, San Francisco, Tokyo
Bastway M, Hasona N, Selemain H (2008) Protective effects of extract from dates (Phoenix dactylifera L.) and ascorbic acid on thioacetamide-induced hepatotoxicity in rats. Iran J Pharm Res 7(3):193–201
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Bokov A, Chaudhuri A, Richardson A (2004) The role of oxidative damage and stress in aging. Mech Ageing Dev 125(10–11):811–826
Buhl SN, Jackson KY (1978) Optimal conditions and comparison of lactate dehydrogenase catalysis of the lactate-to-pyruvate and pyruvateto-lactate reactions in human serum at 25, 30, and 37 degrees C. Clin Chem 24:828–831
Chen X (2010) Protective effects of quercetin on liver injury induced by ethanol. Pharmacogn Mag 6(22):135
Chen HC, Yip T, Lee JK, Juliani J, Sernia C, Hill AF, Lavidis NA, Spiers JG (2020) Restraint stress alters expression of glucocorticoid bioavailability mediators, suppresses NRF2, and promotes oxidative stress in liver tissue. Antioxidant 9(853):1–20
Courtois A, Payen L, Guillouzo A, Fardel O (1999) Up-regulation of multidrug resistance-associated protein 2 (MRP2) expression in rat hepatocytes by dexamethasone. FEBS Lett 459:381–385
Coutinho AE, Chapman KE (2011) The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 335:2–13
Devi KB, Vijaya KR, Sultana R (2016) Quality nutrition through African yam bean: a review. Health 2:133–144
El-Ashmawy M, El-Nahas AF, Salama OM (2005) Protective effect of volatile oil, alcoholic and aqueous extracts of Origanum majorana on lead acetate toxicity in mice. Basic Clin Pharmacol Toxicol 97(4):238–243
El-Denshary ES et al (2015) Possible synergistic effect and antioxidant properties of chitosan nanoparticles and quercetin against carbon tetrachloride-induce hepatotoxicity in rats. Soft Nanosci Lett 5(2):36
Erenler R, Sen O, Aksit H et al (2016) Isolation and identification of chemical constituents from Origanum majorana and investigation of antiproliferative and antioxidant activities. J Sci Food Agric 96:822–836
Feng YL, Tang XL (2014) Effect of glucocorticoid-induced oxidative stress on the expression of Cbfa1. Chem Biol Interact 207:26–31
Feng R, Feng L, Yuan Z, Wang D, Wang F, Tan B et al (2013) Icariin protects against glucocorticoid-induced osteoporosis in vitro and prevents glucocorticoid-induced osteocyte apoptosis in vivo. Cell Biochem Biophys 67:189–197
Giordano FJ (2005) Oxygen, oxidative stress, hypoxia, and heart failure. J Clin Investig 115(3):500–508
Goldberg DM, Spooner RJ (1983) Assay of glutathione reductase. In: Bergmayer HU (ed) Methods in enzymology. Academic Press, New York, pp 258–265
Ha WS et al (2001) Study on mechanism of multistep hepatotumorigenesis in rat: development of hepatotumorigenesis. J Vet Sci 2(1):53–58
Habig WH, Pabst MJ, Jakoby WB (1974) Glutathione S-transferases. The first enzymatic step in mercapturic acid formation. J Biol Chem 249:7130–7139
Hasona N, Morsi A (2019) Grape seed extract alleviates dexamethasone induced hyperlipidemia, lipid peroxidation, and hematological alteration in rats. Indian J Clin Biochem 34(2):213–218. https://doi.org/10.1007/s12291-018-0736-z
Hasona NA, Alrashidi AA, Aldugieman TZ, Alshdokhi AM, Ahmed MQ (2017) Vitis vinifera extract ameliorate hepatic and renal dysfunction induced by dexamethasone in albino rats. Toxics 5(2):11
Hazra A, Pyszczynski NA, DuBois DC, Almon RR, Jusko WJ (2008) Pharm Res 25:769–780
Heo HJ, Cho HY, Hong B, Kim HK, Heo TR, Kim EK, Kim SK, Kim CJ, Shin DH (2002) Ursolic acid of Origanum majorana L. reduces Abeta-induced oxidative injury. Mol Cells 13(1):5–11
Hossain MB, Camphuis G, Aguilo-Aguayo I et al (2014) Antioxidant activity guided separation of major polyphenols of O. majorana (Origanum majorana L.) using flash chromatography and their identification by liquid chromatography coupled with electrospray ionization tandem mass spectrometry. J Sep Sci 37:3205–3213
Hussain AI, Anwar F, Rasheed Sh et al (2011) Composition, antioxidant and chemotherapeutic properties of the essential oils from two Origanum species growing in Pakistan. Rev Bras Farmacogn 21(6):943–952. https://doi.org/10.1590/S0102-695X2011005000165
Iorga A, Dara L, Kaplowitz N (2017) Drug-induced liver injury: cascade of events leading to cell death, apoptosis or necrosis. Int J Mol Sci 18:1018
Iuchi TM, Akaike T, Mitsui Y, Ohshima Y, Shintani H, Azuma, et al (2003) Glucocorticoid excess induces superoxide production in vascular endothelial cells and elicits vascular endothelial dysfunction. Circ Res 92:81–87
Kamanli A, Naziroglu M, Aydilek N, Hacievliyagil G (2004) Plasma lipid peroxidation and antioxidant levels in patients with rheumatoid arthritis. Cell Biochem Funct 22:53–57
Kimura M, Moteki H, Ogihara M (2011) Inhibitory effects of dexamethasone on hepatocyte growth factor-induced DNA synthesis and proliferation in primary cultures of adult rat hepatocytes. J Pharmacol Sci 115:390–398
Kozlowska M, Laudy AE, Starosciak BJ (2010) Antimicrobial and antiprotozoal effect of sweet O. majorana (Origanum majorana L.). Acta Sci Pol Hortorum Cultus 9:133–141
Kubitz R, Wettstein M, Warskulat U, HaÈussinger D (1999) Regulation of the multidrug resistance protein 2 in the rat liver by lipopolysaccharide and dexamethasone. Gastroenterology 116:401–410
Lucas RL, Lentz KD, Hale AS (2004) Collection and preparation of blood products. Clin Tech Small Anim Pract 19(2):55–62
Mansour SA, Mossa ATH (2010) Oxidative damage, biochemical and histopathological alterations in rats exposed to chlorpyrifos and the antioxidant role of zinc. Pestic Biochem Physiol 96(1):14–23
Megwas AU, Njoku OC, Akunne PN, Oladosu NO, Airaodion AI (2021) Ameliorative potential of bambara nuts against acute ethanol-induced oxidative stress in Wistar rats. Int J HealthSaf Environ 7(02):789–800
Miguel MG (2010) Review: antioxidant activity of medicinal and aromatic plants. Rev Flavour Fragr J 25:291–312
Mossa AT, Nawwar GA (2011) Free radical scavenging and antiacetylcholinesterase activities of Origanum majorana L. essential oil. Hum Exp Toxicol 30:1501–1513
Mossa AT, Refaie AA, Ramadan A, Bouajila J (2013) Amelioration of prallethrin-induced oxidative stress and hepatotoxicity in rat by the administration of Origanum majorana essential oil. Biomed Res Int 2013:859085. https://doi.org/10.1155/2013/859085
Mossa AH (2004) Genotoxicity of pesticides [Ph.D. thesis], Pesticide chemistry and toxicology, faculty of agriculture, Damanhour, Alexandria University
Motafeghi F, Mortazavi P, Ghassemi-Barghi N, Zahedi M, Shokrzadeh M (2022) Dexamethasone as an anti-cancer or hepatotoxic. Toxicol Mech Methods. https://doi.org/10.1080/15376516.2022.2105183
Ogbuagu EO, Airaodion AI, Ogbuagu U, Airaodion EO (2019) Prophylactic propensity of methanolic extract of Vernonia amygdalina leaves against acute ethanol-induced oxidative stress in Wistar rats. Int J Bio-Sci Bio-Technol 11(7):37–46
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med 70:158–169
Pascussi JM, Gerbal-Chaloin S, Fabre JM, Maurel P, Vilarem MJ (2000) Dexamethasone enhances constitutive androstane receptor expression in human hepatocytes: consequences on cytochrome P450 gene regulation. Mol Pharmacol 58:1441–1450
Pascussi JM, Drocourt L, Gerbal-Chaloin S, Fabre JM, Maurel P, Vilarem MJ (2001) Dual effect of dexamethasone on CYP3A4 gene expression in human hepatocytes. Sequential role of glucocorticoid receptor and pregnane X receptor. Eur J Biochem 268:6346–6358
Pelvan E, Karaoğlu Ö, Fırat EÖ, Kalyon KB, Ros E, Alasalvar C (2022) Immunomodulatory effects of selected medicinal herbs and their essential oils: a comprehensive review. J Funct Foods 94:105108
Queralt VA, Regueiro J, Rinaldi Alvarenga JF et al (2015) Characterization of the phenolic and antioxidant profiles of selected culinary herbs and spices: caraway, turmeric, dill, O. majorana and nutmeg. Food Sci Technol 35(1):189–195. https://doi.org/10.1590/1678-457X.6580
Ramadan G, El-Beih NM, Zahra MM (2012) Egyptian sweet O. majorana leaves protect against genotoxicity, immunosuppression and other complications induced by cyclophosphamide in albino rats. Br J Nutr 108:1059–1068
Reitman A, Frankel SA (1957) Colorimetric method for the determination serum glutamic oxaloacetic and glutamic pyruvic transaminases. Am J Clin Pathol 28:56–63
Rosalki SB, Foo AY, Burlina A, Prellwitz W, Stieber P, Neumeier D et al (1993) Multicenter evaluation of Iso-ALP test kit for measurement of bone alkaline phosphatase activity in serum and plasma. Clin Chem 39:648–652
Rui L (2014) Energy metabolism in the liver. Compr Physiol 4(1):177–197
Safaei N, Shomali T, Taherianfard M (2012) Niacin ameliorates lipid disturbances due to glucocorticoid administration in rats. Iran J Basic Med Sci 15(4):997–1002
Sato H, Takahashi T, Sumitani K, Takatsu H, Urano S (2010) Glucocorticoid generates ROS to induce oxidative injury in the hippocampus, leading to impairment of cognitive function of rats. J Clin Biochem Nutr 47:224–232
Shati AA (2011) Effects of Origanum majorana L. on cadmium induced hepatotoxicity and nephrotoxicity in albino rats. Saudi Med J 32(8):797–805
Singh H, Jambunathan S (2017) Evaluation of the hypoglycemic effect of Sphenostylis stenocarpa (seeds) in mice. Indian Journal 36:10–23
Triantaphyllou K, Blekas G, Boskou D (2001) Antioxidative properties of water extracts obtained from herbs of the species Lamiaceae. Int J Food Sci Nutr 52(4):313–317
Turncliff RZ, Meier PJ, Brouwer KL (2004) Effect of dexamethasone treatment on the expression and function of transport proteins in sandwich-cultured rat hepatocytes. Drug Metab Dispos 32:834–839
Vagi E, Rapavi E, Hadolin M et al (2005) Phenolic and triterpenoid antioxidants from Origanum majorana L. herb and extracts obtained with different solvents. J Agric Food Chem 53:17–21
Valko M (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39:44–84. https://doi.org/10.1016/j.biocel.2006.07.001
Villalva M, Jaime L, Aguado E, Nieto JA, Reglero G, Santoyo S (2018) Anti-inflammatory and antioxidant activities from the basolateral fraction of caco-2 cells exposed to a rosmarinic acid enriched extract. J Agric Food Chem 66:1167–1174
Yin G, Cao L, Du J, Jia R, Kitazawa T, Kubota A et al (2017) Dexamethasone-induced hepatomegaly and steatosis in larval zebrafish. J Toxicol Sci 42(4):455–459
Acknowledgements
Not applicable.
Funding
The authors did not receive any funding to carry out the study.
Author information
Authors and Affiliations
Contributions
In this study WH and HA have conceived and planned the experiments. WH and HA carried out the experiments. HA analyzed the data. HA and WH discussed the results. HA prepared, edited, reviewed and finalized the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The National Institutes of Health (NIH) and Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) criteria for the handling and use of experimental animals were followed in all animal operations. All experiments were performed in line with the ethical guidelines approved by the Medical Research Ethics Committee of the National Research Centre, El Dokki, Egypt of Experimental Animals (No. 20286).
Consent for publication
Not applicable.
Competing interests
The authors do not declare any conflict of interest about this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abou- Seif, H.S., Hozayen, W.G. Origanum majorana L. extract alleviates dexamethasone-induced hepatotoxicity, oxidative stress and pathological alterations in vivo. Bull Natl Res Cent 47, 39 (2023). https://doi.org/10.1186/s42269-023-01012-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-023-01012-1