Abstract
Background
Pulmonary rehabilitation (PR) has proven to improve the physical and psychosocial function in patients with chronic obstructive pulmonary disease (COPD). However, the gains achieved during pulmonary rehabilitation diminish over time without an effective maintenance strategy. With several factors affecting access to pulmonary rehabilitation, calls for innovative models were made, which saw the emergence of studies exploring telerehabilitation (TR) as an alternative to traditional pulmonary rehabilitation models. Although there are current reviews exploring the effectiveness of telerehabilitation as an alternative for conventional PR, no review has considered telerehabilitation effectiveness in the long term. Hence, this review aims at examining the effectiveness of telerehabilitation following to pulmonary rehabilitation in patients with chronic obstructive pulmonary disease.
Main body
A systematic review of the literature using CINAHL, MEDLINE, SCOPUS, Web of science PEDRO, AMED and EMBASE databases was conducted to assess the effectiveness of telerehabilitation following PR in patients with COPD. Health-related quality of life (HRQoL) and exercise capacity was maintained within 6–12 months of a TR maintenance programme. However, there was no significant increase in HRQoL and exercise capacity between the intervention and control groups in 6–12 months.
Conclusions
This review suggests that a TR maintenance strategy effectively maintains benefits gained and may improve HRQoL and exercise capacity within 6–12 months for patients with COPD. Nonetheless, it is impossible to extrapolate the findings to the general population due to the paucity of included studies. Further high quality randomised controlled trials examining TR in the long-term is required in the future.
Similar content being viewed by others
Background
According to the National Institute for Health and Care Excellence [NICE] 2021, chronic obstructive pulmonary disease (COPD) is an umbrella term for chronic bronchitis and emphysema. Although closely related, they are not synonymous with each other. While chronic bronchitis is characterised by hypersecretion and prolonged cough (Kesimer et al. 2017), emphysema is characterised by structural changes in the extracellular matrix and air space of the terminal bronchiole (Amariei et al. 2019). A predominant feature of COPD is a poorly reversible airway limitation and dyspnoea known to cause a decrease in physical activity (PA), health-related quality of life (HRQoL) and an increase in acute exacerbation (Vestbo et al. 2013; Alqahtani et al. 2020).
Pulmonary rehabilitation (PR) is an evidence-based intervention proven effective in chronic respiratory conditions as it adopts a holistic approach in managing respective conditions (Camp and Cheung 2018) and involves a multi-disciplinary team that focuses on improving both the physical and psychological function of patients with COPD whilst promoting long-term adherence to health-enhancing behaviour, quality of life (QoL) and exercise tolerance improvement (Hill 2006; Spruit et al. 2013; Anastasaki et al. 2019). The various components of PR include but are not limited to exercise training, patient education, dietary changes and behavioural interventions (Camp and Cheung 2018). Additionally, PR promotes self-management strategies to enable individuals to self-manage their conditions effectively (Bolton et al. 2013). An individualised programme tailored to the patient needs, must be administered by a multi-disciplinary team to ensure a successful PR programme.
For an extended period, COPD treatments mostly focused on the pharmacological improvement of airway obstruction (Alqahtani et al. 2020). However, within the last 2 decades, the systemic impact of COPD in the overall health of individuals with the condition has precipitated the development of various non-pharmacological treatments such as pulmonary rehabilitation (PR) to augment the medical management of COPD (Corhay et al. 2014).
Several international guidelines recommend PR for symptomatic patients with COPD when pharmacological interventions alone do not decrease symptoms (Qaseem et al. 2011; Vestbo et al. 2013). Despite the documented benefits of PR, the long-term benefits of PR are short-lived without an effective maintenance strategy (Ries et al. 2003; Bolton et al. 2013). Several studies have explored maintenance strategies such as community PR (Moullec et al. 2008; van Wetering et al. 2010) and home-based PR (Wijkstra et al. 1995; Holland et al. 2013); the effectiveness of these strategies were not well-established in the literature. In the same vein, the American thoracic society and European respiratory society (ATS) acknowledged the urgent need for the research and development of novel models of pulmonary rehabilitation that will provide accessible, evidence-based PR programs for individuals with COPD (Rochester et al. 2015).
Several studies have investigated the delivery of PR while employing telemedicine-based interventions (Holland and Cox 2017; Zanaboni et al. 2017). Telerehabilitation, a subset of telemedicine, has been defined as the alternative way of delivering rehabilitation services using information and communication technologies (Laver et al. 2020). A systematic review by Chan et al. (2016) synthesised evidence on how telemonitoring and TR affected the quality of life (QOL) and exercise capacity of patients with COPD short term. The results show that TR provided similar results with usual care defined as traditional cardiac rehabilitation and PR. More so, the review was not specific to COPD and included patients with cardiovascular conditions. Finally, maintenance of benefits was neither mentioned nor investigated by the authors. A Cochrane review by Cox et al. (2020) explored the effects of TR in chronic respiratory diseases with results showing that TR achieves similar results as a traditional PR programme. The authors noted that 99% of the subject participants were patients with COPD. However, the findings obtained from this review should be treated with caution as a limited number of studies was included in the review and the small number of participants. None of those reviews mentioned above explored TR long-term or as a maintenance strategy following PR. Hence, even though the TR in COPD management is safe and feasible, it is still unclear if the benefits achieved after an outpatient’s PR programme can be maintained after 6–12 months with a TR maintenance programme.
Therefore, this review aims to explore the effectiveness of a < 6 months maintenance TR programme following a PR programme.
Main text
Healthcare research informs the decisions and guidelines utilised in clinical practice. However, as the body of evidence grew, it became imperative to have a rigorous and systematic synthesis of available evidence (Aromataris and Pearson 2014). Historically, systematic reviews started showing up in health literature around the 1970s and 1980s with the advent of evidence-based healthcare and have continued to evolve till now (Bastian et al. 2010). Systematic reviews are rudimentary in evidence-based healthcare and provide the highest level in the hierarchy of evidence in research (Aromataris et al. 2015). Hence, a systematic review aims at providing a comprehensive, unbiased synthesis of evidence using transparent methods. It is methodological and utilises predetermined methods that appraise, summarise, and synthesise available primary research (Cajal et al. 2020). In order to maintain the same rigour and standard of primary research being reviewed, a pre-planned set of protocols to be peer-reviewed at the outset is published just like the research proposal (Jones and Evans 2000). According to JBI, this stage is perhaps the most important step as the planning and thoughtfulness put in this process ensures the review is well-defined, rigorous and reduces the risk of bias (Boland et al. 2017; Jordan et al. 2019).
Review question
Is telerehabilitation an effective maintenance strategy following pulmonary rehabilitation for patients with chronic obstructive pulmonary diseases (COPD)? A systematic review.
Methods
This systematic review followed a published protocol (CRD42022364398) and was conducted using the Preferred Reporting Items for Systematic Review and Meta—Analysis (PRISMA) method. A PRISMA checklist is presented in Additional file 1.
Our inclusion criteria were:
-
Studies addressing adults aged > 40 with a diagnosis of COPD, randomised controlled trials (RCT), quasi-experimental studies and cohort studies.
-
Studies with participants who completed > 6-month telerehabilitation maintenance programme following PR and any study that measures the following primary outcomes: exercise capacity and health-related quality of life (HRQoL).
We excluded studies on adults with other chronic respiratory conditions, studies where the participants did not receive PR or received only telemonitoring, all non-English language studies, animal studies, qualitative studies and grey literature.
Information sources
The following databases were searched from inception to 18 October 2022; MEDLINE, EMBASE, PEDro, AMED, Web of Science, CINAHL, JBI, Scopus.
Search strategy
The following keywords were used for the initial search: Telerehabilitation* OR tele-rehabilitation OR Telemedicine OR “remote rehabilitation” OR Telerehab* AND COPD OR “chronic obstructive disease*”. Boolean logic ‘OR’ commands expanded the search, while ‘AND’ commands limited the search. Truncations was used to expand words with varied endings.
A librarian was involved with the search development to improve the search quality. Citation (forward and backwards) chaining ensured maximum capturing of relevant articles. Grey literature were not included. Finally, article authors were contacted when more information is required.
The search strategy developed for each database is provided in Additional file 2.
Study selection
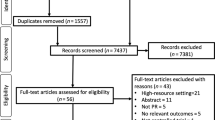
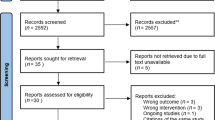
The Preferred Reporting Items for Systematic Reviews and Meta-analyses’ (PRISMA) was utilised. The first stage involved merging selected studies using reference management software such as Endnote to eliminate duplicates. The titles and abstracts were then screened based on the inclusion/exclusion criteria to remove irrelevant articles. This process was carried out by four reviewers. Full-text retrieval of the remaining relevant studies followed suit, after which each study was read in full to ensure it fits the eligibility criteria.
Data extraction
The JBI data extraction form for experimental studies was utilised for this review. It was piloted with two included studies then modified accordingly to extract only data relevant to the review. This enables standardisation of the data extraction tool across all included studies ensuring consistency and accuracy of data extracted. Four authors independently extracted the following data from included studies: (see Additional file 3 for the completed data extraction form).
-
Participants: settings, population, gender, sample size and groups
-
Baseline characteristics: age, sex, BMI, FEV1 (L) FEV1 (%) FVC (L) FVC (%) FEV1/FVC
-
Intervention and comparison groups: IG & CG (n = 94) 8 weeks ± 4 days, IG (n = 46) 12 months, CG (n = 48) 12 months
-
Clinical outcomes measures: Exercise capacity, Quality of life (QoL).
Methodological quality assessment
Four independent reviewers used a validated critical appraisal tool to ensure that the highest quality of evidence is included in the review. The Physiotherapy Evidence-based database (PEDro) scale was utilised. Only studies that met all the essential criteria set out by the four reviewers proceeded to the next stage.
Data synthesis
Data were synthesised narratively due to the heterogeneity of the outcome measures of interest.
Result
Five thousand nine hundred seventy-four articles were found during the search process, with 2640 duplicates removed. Following that, a title screening process of the remaining 3424 articles produced 250 articles, further filtered out by abstract screening. Back chaining of the reference lists did not reproduce any new studies meeting the inclusion criteria. Finally, 27 studies were read in full, and six articles were carried through to the critical appraisal stage. A modified PRISMA flow diagram illustrating the filtration process is shown in Fig. 1.
Study characteristics
A summary of the interventions reported across the included studies is presented in Table 1. All the included studies were RCTs. Two studies were undertaken in Spain, while one was carried out in Greece, with the final study in Australia. This limits the generalisability of the studies as a greater proportion of studies was undertaken in Europe. Even one of the studies excluded during the critical appraisal stage was undertaken in Europe–Netherlands (Vorrink et al. 2016) with the study by Li et al. (2018) carried out in China. There was no variation in the population as all the participants were clinically stable which meant they did not have any acute exacerbations with COPD severity of II–IV based on the GOLD classification, correlating with recommendations by various international guidelines when offering patients with COPD PR (GOLD 2022; NICE 2022). The age range shows the lowest age range included was 18 years, with the highest being 85 years and a mean age of 51.5 years. Studies have shown that most patients present with COPD symptoms at an average age of 40 years (Izquierdo et al. 2021; Soriano et al. 2021). In addition, only about 2.8% of the COPD population are aged about 18–30 years (de Marco et al. 2007), with most of them presenting with α-1 antitrypsin deficiency (GOLD 2022).
All the included studies showed a significant difference in the percentage of men to women, with men making up a higher percentage of the population. All the participants were either current smokers intending to quit or ex-smokers, correlating with various studies that smoking is a major risk factor of COPD (Laniado-Laborín 2009; Halpin et al. 2019; Salvi et al. 2020). Only Galdiz et al. (2020) had participants who were non-smokers, but then evidence estimates 20% of the population with COPD has never smoked (Lamprecht et al. 2011). Although most of the participants were smokers, there appears to be a smoking cessation trend, with two studies showing a majority of the participants who have quit smoking (Vasilopoulou et al. 2017; Jimenez-Reguera 2020), reflecting on international recommendations about the influence of smoking cessation on COPD (British thoracic society [BTS] 2022; NICE 2020; GOLD 2022).
TR was delivered through two different forms by the included studies. A web-based platform installed on a mobile device was utilised by Galdiz et al. (2020), Vasilopoulou et al. (2017) and Jimenez-Reguera et al. (2020), while Wootton et al. (2018) utilised phone calls only to deliver TR. None of the interventions involved real-time remote telemonitoring except Vasilopoulou et al. (2017), where the participants were equipped with a multimodal device for spirometry and oxygen saturation measurement. All the other participants had to input data collected manually onto a web platform or in a diary, as in the case of Wootton et al. (2018).
Only Jimenez-Reguera et al. (2020) had the participants engaging in the TR maintenance programme at a higher frequency than the initial PR programme, similar to the frequency of several maintenance programmes (Ries et al. 2003; Bernocchi et al. 2018; Spencer and McKeough 2019). Galdiz et al. (2020) and Wootton et al. (2017) had the intervention group engaging at a frequency that is equivalent to the frequency of the initial PR programme, while Vasilopoulou et al. (2017) did not state the frequency as the participants engaged in the TR programme. A recent systematic review by Malaguti et al. (2021) found that the duration of a maintenance PR programme ranges from 4 weeks to 36 months. As shown in Table 1, all the included studies engaged in a TR maintenance programme for a 12-months duration except from Jimenez-Raguera et al. (2020), where participants underwent a 10-month TR maintenance programme. Physiotherapists oversaw the TR maintenance programme except in the study by Vasilopoulou et al. (2017), where the authors did not specify but noted healthcare professionals delivered the TR programme.
Study Outcomes
The primary outcomes predetermined during the planning stage were exercise capacity and HRQoL. Table 1 shows all four included studies measured all the pre-set outcomes. However, there is a variation in the outcome measures for HRQoL as multiple outcome measures were used to measure one outcome. However, this is not unusual for conditions such as COPD, where an individual’s health status cannot be quantified adequately with a single outcome measure (Vestbo et al. 2013; Vickerstaff et al. 2021). HRQoL and QoL are often used interchangeably. However, QoL is a broad term that covers all aspects of human life. On the other hand, HRQoL is focused on the effect of the diseases and intervention on the QoL of the individual (Lin et al. 2013). The outcomes for HRQoL employed by the studies were SGRQ, CRQ, and CAT, proven valid and reliable (Reda et al. 2010; Ringbaek et al. 2012; Gupta et al. 2014). Furthermore, they represent the outcome measures used in COPD research to assess QOL (Ringbaek et al. 2012). Two of the studies used both SGRQ and CAT to assess HRQoL (Vasilopoulou et al. 2017; Jimenez-Reguera et al. 2020), Galdiz et al. (2020) used both CRQ and CAT, while Wootton et al. (2018) used SGRQ and CRQ. In addition, Galdiz et al. (2020) and Jimenez-Reguera et al. (2020) assessed QoL with the SP-36 and EuroQOL-5D tools, respectively.
Exercise capacity was assessed with the 6MWT only except Wootton et al. (2018) that employed two more outcome measures, ISWT and ESWT; therefore, little variability exists between the outcome measures for exercise capacity. Although the 6MWT may not be advantageous for individuals with better exercise tolerance, it is a valid and reliable outcome measure of functional capacity in cardiopulmonary patients (Ghofraniha et al. 2015).
Reported biases
Some degree of limitation exists in the methodology of synthesis in terms of bias. For instance, the theoretical model was subjective as its best, the selection and grouping of the components of the study were equally subjective to an extent.
Due to the time constraint associated with this review, it was impossible to double the data extraction stage. The paucity of the included studies greatly affects the generalisability; therefore, the findings obtained in this review will not inform clinical practice. Rather, it will identify gaps and make recommendations for future research. Ongoing studies on the subject area show current research is ongoing on TR as an alternative to PR, especially with the pandemic and the need for social distancing. Although research into better technology to improve TR is currently underway, TR is still in its early stage of implementation in clinical practice worldwide (Alexander 2020).
Discussion
There is currently an abundance of studies relating to TR as an alternative to PR in the short term; however, its long-term effectiveness as a maintenance strategy has not fully been explored.
A robust search strategy was formulated with the guidance of the subject librarian, as recommended by the Cochrane Handbook (Higgins et al. 2019). Following the formulation of the search strategy, a comprehensive search of key databases was carried out by the reviewer. The search process reproduced 3934 articles after deduplication. However, only six studies were included in the review. Initially, a substantial amount of evidence on TR in the long-term was found; however, on close inspection, it was discovered that some were duplicates while others did not meet the inclusion criteria as set out in the review protocol. Subsequently, following critical appraisal, four studies were taken to the data extraction and synthesis stage. Coincidentally, all the included studies were RCTs; however, the heterogeneity of the study outcome measures, and the paucity of the included studies precipitated narrative synthesis rather than meta-analysis for data synthesis.
This systematic review identified, included, and evaluated four studies on the effectiveness of a > 6 months TR maintenance programme as a maintenance strategy following PR. Although the studies show that intervention effectively preserved the benefits gained following PR, there is limited evidence of its superiority to other PR maintenance programmes (hospital-based maintenance and no care). In the same vein, the results of the included studies showed that there were no improvements across the outcomes assessed (HRQoL and exercise capacity) between groups over 6–12 months.
A systematic review by Imamura et al. (2020) found a medium-frequency maintenance programme, as seen in Wootton et al. (2018), where the participants were advised to engage in the intervention 2–3 times per week effective in maintaining exercise capacity but not HRQoL. The outcome measures utilised to assess exercise capacity were the 6MWT and the incremental shuttle walking test (ISWT), while the SGRQ assessed HRQOL. Although the variability displayed in the frequency of the included studies' maintenance programmes is similar to that seen in other studies (Beauchamp et al. 2013; Malaguti et al. 2021), it is difficult to determine the optimal frequency of maintenance programmes. Several studies have implicated individual perception of self, social/environmental factors, acute exacerbations, intrinsic motivation, structure/delivery of maintenance programmes as some of the determinants of long-term adherence (McAuley et al. 2007; O’Donoghue et al. 2018; Puggina et al. 2018). As witnessed in this current review, Wootton et al. (2018) had the IG receiving motivational sessions and health coaching, possibly explaining why the IG saw a lower drop-out rate while still maintaining benefits gained from baseline to the twelfth month. Maintenance programmes should not be a one size fits all. As seen with most of the included studies where the intervention was tailored to patient’s needs, it is important they are adapted to individual circumstances, considering environmental, socioeconomic, and individual health factors (Bogerd et al. 2011; McNamara et al. 2013). In contrast, this may pose a major challenge in determining the optimal frequency of a maintenance programme.
TR can be delivered asynchronously (delayed), synchronously (real-time) or with a combination of the two delivery modes (Hill and Breslin 2016). A scoping review by Morimoto et al. (2022) evaluating the theoretical approach and functional features of web platforms for TR in chronic diseases found web platforms to be more effective in delivering asynchronous correspondence than synchronous correspondence. A major reason for this is the ability of web platforms to display and unify multiple information available to all stakeholders, thereby decreasing the hurdle of participating in one's rehabilitation or a need for a different system as seen in real-time technology (Kloek et al. 2017; Cox and Holland 2019). However, this deviates from recent advancements in technology where telemonitoring systems are increasingly utilised to collect real-time health-related data (Lundell et al. 2015; Bourbeau and Farias 2018). As seen with several studies that utilised a web platform, it appears an asynchronous communication is better suited to improving adherence and promoting self-management than synchronous communication (Tabak et al. 2014; Zanaboni et al. 2016). Self-monitoring is known as one of the factors leading to improved maintenance (Busby et al. 2014). Hence, it may benefit studies to utilise self-monitoring devices such as wrist-worn activity trackers.
Similarly, recent studies have highlighted its role in optimising self-management, motivation and behavioural tracking amongst various age groups (Puri et al. 2017; Ellingson et al. 2019; Liao et al. 2020). In support, several qualitative studies have also shown patients’ participation in the daily registration of their symptoms and PA sessions provided them control over their health and increased their drive to engage in their sessions (Dinesen et al. 2011; Hoaas et al. 2016).
Limitations
Several limitations were associated with this present review. Although the reviewers carried out a comprehensive search of various databases, the time constraint made it impossible to search grey literature, possibly leading to publication bias. The search restriction to only English language studies possibly introduced a language bias. In addition, to ensure reproducibility and reliability of findings, only a few studies were selected following the application of the inclusion and exclusion criteria, consequently reducing the number of studies reviewed and, as such, reducing the generalisability of findings.
Albeit the hierarchy of evidence of the included studies, RCT, none of the study participants was blinded to the intervention; similarly, only one study blinded the assessors, subsequently predisposing the review to selection bias, performance bias, and detection bias. Noteworthy, given the nature of the intervention, it was impossible to blind the participants and therapist as with many other physiotherapy interventions. Despite recommendations from Cochrane and JBI, the reviewer was unable to double the data extraction and data synthesis stage secondary to associated time constraints and feasibility, increasing the risk of substantial errors (Stephenson et al. 2020).
Implication to clinical practice
The findings of this review suggest TR is effective in maintaining HRQoL and exercise capacity following PR for > 6 months. No adverse effects were reported for the use of intervention; however, there is no evidence that a > 6 months maintenance TR programme will improve HRQoL and exercise capacity. It appears the number of weeks the initial PR programme affected had a relationship with how long the benefit gained were maintained irrespective of a TR programme. For instance, it appears a 10-week PR appears to maintain benefits gained better than a 6-week PR programme in the long term (Steel et al. 2011; Cox et al. 2020).
It was observed that none of the studies included was carried out in the UK; the lack of research in the area of interest has affected the decisions such as policy changes, resource allocation and patient-related outcomes and so on. An audit statement released by the National Asthma and Chronic Obstructive Pulmonary Diseases Audit Programme [NACAP] shows that only about 1.3% of patients referred for PR are home-based- home visits or via TR (Singh et al. 2020). The majority of the intervention is delivered via home visits, with 40% by telephone calls and 2.3% by use of technology-based PR (videoconferencing) and 1.7% of other digital communication. Although the relevant NICE programmes mentioned maintenance, details about maintenance strategies were non-existent (NICE 2022).
In Greece, Vasilopoulou et al. (2017) reported very few PR services were available, with maintenance programmes completely non-existent. Furthermore, TR is more cost-effective than centre-based rehabilitation (Haesum et al. 2012; Frederix et al. 2020), with no adverse effect on delivering maintenance rehabilitative services via that route. The intervention also provides more options for clinicians when providing patient-centred care as it is imperative that care is tailored to individual patients' needs. Finally, the pandemic has opened an opportunity to explore future changes, not only making TR accessible but easily requested by patients. Hence, healthcare systems and stakeholders worldwide should consider re-evaluating and implementing this innovative service for long-term maintenance programmes.
Future research
Recently, there has been a surge in the number of studies on the effectiveness of TR as an alternative to traditional models of PR short term; however, its long-term efficacy as a maintenance strategy is yet to be determined. Hence, there is a need for large and good quality multicentre RCTs on the long-term effectiveness of TR as increased effect size reduces associated bias. It is also important to explore the determinants and factors affecting a TR maintenance programme. This review highlights the need for more research into what constitutes an effective maintenance programme as it appears older studies on maintenance focused only on exercises for maintenance. Meanwhile, recent studies show exercises alone is not an effective maintenance strategy based on the nature of the condition.
There is a need for more homogenous studies on the TR maintenance programmes to standardise various patient groups based on the international classification of COPD (GOLD classification). It is possible that adapting evidence-based, individualised maintenance programmes for various treatment groups may be the way to go in the future. Following the COVID-19 pandemic, it appears people have become more familiarised with the use of online platforms coupled with the improvement of internet services. TR may become the first line of request for patients in COPD management. Finally, with recent advances in technology, further research on how to improve the TR experience and encourage self-management may improve the delivery of rehabilitative services.
Conclusions
This review explored the effectiveness of a > 6 months TR as a maintenance strategy following PR. The possible impact on two outcomes (HRQoL and exercise capacity) was equally evaluated. The findings reveal a need for further research as the paucity of the included studies and the fact that the study was limited to mostly Europe and Australia limit the generalisability of the study findings.
Availability of data and materials
All data analysed during this study are included in this article and its additional file.
Abbreviations
- SGRQ:
-
Saint George’s respiratory questionnaire
- CRQ:
-
Chronic respiratory questionnaire
- BMI:
-
Body mass index
- FEV:
-
Forced expiratory volume
- FVC:
-
Forced vital capacity
- ISWT:
-
Increment shuttle walking test
References
Alexander M (2020) It’s corona calling: time for telerehabilitation! J Frailty Sarcopenia Falls 5:4–86
Alqahtani JS et al (2020) Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS ONE 15(5):e0233147
Amariei DE, Dodia N, Deepak J, Hines SE, Galvin JR, Atamas SP, Todd NW (2019) Combined pulmonary fibrosis and emphysema: pulmonary function testing and a pathophysiology perspective. Medicina 55(9):580
Anastasaki M et al (2019) Establishing a pulmonary rehabilitation programme in primary care in Greece: a FRESH AIR implementation study. Chron Respir Dis. https://doi.org/10.1177/1479973119882939
Aromataris E, Pearson A (2014) SYSTEMATIC REVIEWS, Step by step: the systematic review: an overview. Am J Nurs 114(3):53–58
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P (2015) Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement 13(3):132–140
Bastian H, Glasziou P, Chalmers I (2010) Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med 7(9):e1000326
Beauchamp MK, Evans R, Janaudis-Ferreira T, Goldstein RS, Brooks D (2013) Systematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPD. Chest 144:1124–1133. https://doi.org/10.1378/chest.12-2421
Bernocchi P et al (2018) Home-based telerehabilitation in older patients with chronic obstructive pulmonary disease and heart failure: a randomised controlled trial. Age Ageing 47(1):82–88. https://doi.org/10.1093/ageing/afx146
Bogerd SP et al (2011) Preliminary results of pulmonary rehabilitation in interstitial lung diseases: a randomised controlled trial. Eur Respir Soc 38(Suppl. 55):1451
Boland A, Cherry G and Dickson R (2017) Doing a systematic review: a student's guide
Bolton CE et al (2013) British Thoracic Society guideline on pulmonary rehabilitation in adults: accredited by NICE. Thorax 68(Suppl 2):ii1–ii30
Bourbeau J, Farias R (2018) Making sense of telemedicine in the management of COPD. Eur Respir Soc 51(5):1800851
British Thoracic Society (2022) Smoking cessation (BTS). Available at: https://brit.thoracic.org.uk [Accessed: August 2022]
Busby AK, Reese RL, Simon SR (2014) Pulmonary rehabilitation maintenance interventions: a systematic review. Am J Health Behav 38:321–330. https://doi.org/10.5993/ajhb.38.3.1
Cajal B, Jiménez R, Gervilla E, Montaño JJ (2020) Doing a systematic review in health sciences. Clin Health 31(2):77–83
Camp PG, Cheung W (2018) Are we delivering optimal pulmonary rehabilitation? The importance of quality indicators in evaluating clinical practice. Phys Ther 98(7):541–548. https://doi.org/10.1093/ptj/pzy046
Chan C, Yamabayashi C, Syed N, Kirkham A, Camp PG (2016) Exercise telemonitoring and telerehabilitation compared with traditional cardiac and pulmonary rehabilitation: a systematic review and meta-analysis. Physiother Can 68:242–251. https://doi.org/10.3138/ptc.2015-33
Corhay JL, Dang DN, Van Cauwenberge H, Louis R (2014) Pulmonary rehabilitation and COPD: providing patients a good environment for optimizing therapy. Int J Chron Obstruct Pulmon Dis 9:27–39. https://doi.org/10.2147/COPD.S52012
Cox NS, Holland AE (2019) Current perspectives of physical activity in cystic fibrosis. Expert Rev Respir Med 13:13–22. https://doi.org/10.1080/17476348.2019.1552833
Cox N et al (2020) Telerehabilitation for chronic respiratory disease: a cochrane systematic review. Respirology 25:42. https://doi.org/10.1111/resp.13777
de Marco R et al (2007) Incidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegm. Am J Respir Crit Care Med 175(1):32–39. https://doi.org/10.1164/rccm.200603-381OC
Dinesen B, Grann O, Nielsen C, Hejlesen O, Toft E (eds) (2011) Telerehabilitation across sectors: the experiences of chronic obstructive pulmonary disease (COPD) patients and healthcare professionals. In: 2nd international conference on wireless communication, vehicular technology, information theory and aerospace & electronic systems technology (Wireless VITAE). IEEE
Ellingson LD et al (2019) Evaluating motivational interviewing and habit formation to enhance the effect of activity trackers on healthy adults’ activity levels: randomized intervention. JMIR mHealth uHealth 7:e10988
Frederix I et al (2020) Effect of comprehensive cardiac telerehabilitation on one-year cardiovascular rehospitalization rate, medical costs and quality of life: a cost-effectiveness analysis. Eur J Prev Cardiol 23:674–682. https://doi.org/10.1177/2047487315602257
Galdiz JB et al (2020) Telerehabilitation programme as a maintenance strategy for COPD patients. Arch Bronconeumol 57:195–204. https://doi.org/10.1016/j.arbres.2020.03.034
Ghofraniha L, Dalir Sani Z, Vakilian F, Khajedalooyi M, Arabshahi ZJ (2015) The six-minute walk test (6MWT) for the evaluation of pulmonary diseases. J Cardio-Thoracic Med 3:284–287
Global Initiative for Chronic Obstructive Diseases (2022) GOLD reports. https://goldcopd.org/2022-gold-reports/. Accessed: December 2021
Gupta N, Pinto LM, Morogan A, Bourbeau J (2014) The COPD assessment test: a systematic review. Eur Respir J 44(4):873–884
Haesum LKE et al (2012) Cost-utility analysis of a telerehabilitation program: a case study of COPD patients. Telemed E-Health 18(9):688–692. https://doi.org/10.1089/tmj.2011.0250
Halpin D et al (2019) The GOLD Summit on chronic obstructive pulmonary disease in low-and middle-income countries. Int J Tuberc Lung Dis 23(11):1131–1141
Hernandes NA, Wouters E, Meijer K, Annegarn J, Pitta F, Spruit M (2011) Reproducibility of 6-minute walking test in patients with COPD. Eur Respir J 38(2):261–267
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, London
Hill NS (2006) Pulmonary rehabilitation. Proc Am Thorac Soc 3(1):66–74
Hill AJ, Breslin HM (2016) Refining an asynchronous telerehabilitation platform for speech-language pathology: engaging end-users in the process. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2016.00640
Hoaas H, Andreassen HK, Lien LA, Hjalmarsen A, Zanaboni P (2016) Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study eHealth/telehealth/mobile health systems. BMC Med Inform Decis Mak. https://doi.org/10.1186/s12911-016-0264-9
Holland AE, Cox NS (2017) Telerehabilitation for COPD: could pulmonary rehabilitation deliver on its promise? Wiley Online Library, London
Holland AE et al (2013) Benefits and costs of home-based pulmonary rehabilitation in chronic obstructive pulmonary disease-a multi-centre randomised controlled equivalence trial. BMC Pulm Med 13(1):1–7
Imamura S, Inagaki T, Terada J, Nagashima K, Katsura H and Tatsumi K (2020) Long-term efficacy of pulmonary rehabilitation with home-based or low frequent maintenance programs in patients with chronic obstructive pulmonary disease: a meta-analysis. Ann Palliat Med 9(5):2606–2615
Izquierdo JL et al (2021) Clinical management of COPD in a real-world setting. A big data analysis. Archivos De Bronconeumología (engl Ed) 57(2):94–100
Jimenez-Reguera B et al (2020) Development and preliminary evaluation of the effects of an mHealth web-based platform (HappyAir) on adherence to a maintenance program after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: randomized controlled trial. JMIR mHealth uHealth 8(7):e18465. https://doi.org/10.2196/18465
Jones T, Evans D (2000) Conducting a systematic review. Aust Crit Care 13(2):66–71
Jordan Z, Lockwood C, Munn Z, Aromataris E (2019) The updated Joanna Briggs Institute model of evidence-based healthcare. JBI Evid Implement 17(1):58–71. https://doi.org/10.1097/xeb.0000000000000155
Kesimer M et al (2017) Airway mucin concentration as a marker of chronic bronchitis. N Engl J Med 377(10):911–922. https://doi.org/10.1056/NEJMoa1701632
Kloek C, Bossen D, Bakker DHD, Veenhof C, Dekker J (2017) Blended interventions to change behavior in patients with chronic somatic disorders: systematic review. J Med Internet Res. https://doi.org/10.2196/jmir.8108
Lamprecht B et al (2011) COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 139(4):752–763. https://doi.org/10.1378/chest.10-1253
Laniado-Laborín R (2009) Smoking and chronic obstructive pulmonary disease (COPD). Parallel epidemics of the 21st century. Int J Environ Res Public Health 6(1):209–224
Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C (2020) Telerehabilitation services for stroke. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010255.pub3
Li Y, Feng J, Jia W, Qian H (2018) A new pulmonary rehabilitation maintenance strategy through home-visiting and phone contact in COPD. Patient Prefer Adherence 12:97–104. https://doi.org/10.2147/PPA.S150679
Liao J, Xiao H-Y, Li X-Q, Sun S-H, Liu S-X, Yang Y-J, Xu D (2020) A social group-based information-motivation-behavior skill intervention to promote acceptability and adoption of wearable activity trackers among middle-aged and older adults: cluster randomized controlled trial. JMIR mHealth uHealth 8(4):e14969. https://doi.org/10.2196/14969
Lin X-J, Lin IM, Fan S-Y (2013) Methodological issues in measuring health-related quality of life. Tzu Chi Med J 25(1):8–12. https://doi.org/10.1016/j.tcmj.2012.09.002
Lundell S, Holmner Å, Rehn B, Nyberg A, Wadell K (2015) Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Respir Med 109(1):11–26
Malaguti C, Dal Corso S, Janjua S, Holland AE (2021) Supervised maintenance programmes following pulmonary rehabilitation compared to usual care for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD013569.pub2
McAuley E, Morris KS, Motl RW, Hu L, Konopack JF and Elavsky S (2007) Long-term follow-up of physical activity behavior in older adults. Health Psychol 26(3):375
McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA (2013) Water-based exercise in COPD with physical comorbidities: a randomised controlled trial. Eur Respir J 41(6):1284–1291
Morimoto Y, Takahashi T, Sawa R, Saltoh M, Morisawa T, Kagiyama N, Kasai T, Dinesen B, Hollingdal M, Refsgaard J, Daida H (2022) Web portals for patients with chronic diseases: scoping Review of the functional features and theoretical frameworks of telerehabilitation platforms. J Med Internet Res 24(1):e27759
Moullec G, Ninot G, Varray A, Desplan J, Hayot M, Prefaut C (2008) An innovative maintenance follow-up program after a first inpatient pulmonary rehabilitation. Respir Med 102(4):556–566
National Institute for Health and Care Excellence (2020) Tobacco Preventing uptake, promoting quitting, and treating dependence reports (NICE guidelines). Avaialable at: https://www.brit.thoracic.org.uk/quality-improvement/clinical-resources/smoking-ecessation/. [Accessed: June 2022]
National Institute for Health and Care Excellence (2022) Tobacco Preventing uptake, promoting quitting, and treating dependence reports (NICE guidelines). Avaialable at: https://www.brit.thoracic.org.uk/quality-improvement/clinical-resources/smoking-ecessation/. [Accessed: August 2022]
O’Donoghue G et al (2018) Socio-economic determinants of physical activity across the life course: A "DEterminants of DIet and Physical ACtivity" (DEDIPAC) umbrella literature review. PloS one 13(1):e0190737
Puggina A et al (2018) Policy determinants of physical activity across the life course: a ‘DEDIPAC’ umbrella systematic literature review. Eur J Public Health 28(1):105–118
Puri A, Kim B, Nguyen O, Stolee P, Tung J, Lee J (2017) User acceptance of wrist-worn activity trackers among community-dwelling older adults: mixed method study. JMIR mHealth uHealth 5(11):e8211
Qaseem A et al (2011) Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med 155(3):179–191. https://doi.org/10.7326/0003-4819-155-3-201108020-00008
Reda AA, Kotz D, Kocks JW, Wesseling G, van Schayck CP (2010) Reliability and validity of the clinical COPD questionniare and chronic respiratory questionnaire. Respir Med 104(11):1675–1682
Ries AL, Kaplan RM, Myers R, Prewitt LM (2003) Maintenance after pulmonary rehabilitation in chronic lung disease: a randomized trial. Am J Respir Crit Care Med 167(6):880–888
Ringbaek T, Martinez G, Lange P (2012) A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD: J Chron Obstruct Pulmon Dis 9(1):12–15. https://doi.org/10.3109/15412555.2011.630248
Rochester CL et al (2015) An official American Thoracic Society/European Respiratory Society policy statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med 192(11):1373–1386
Salvi SS et al (2020) Phenotypic comparison between smoking and non-smoking chronic obstructive pulmonary disease. Respir Res 21(1):1–12
Singh S et al (2020) National Asthma and Chronic Obstructive Pulmonary Disease Audit Programme (NACAP). Pulmonary rehabilitation clinical audit 2019. Clinical audit of pulmonary rehabilitation services in England, Scotland and Wales. Patients assessed between 1 June and 17 October. Data analysis and methodology report. London
Soriano JB et al (2021) Prevalence and determinants of COPD in Spain: EPISCAN II. Arch Bronconeumol 57(1):61–69. https://doi.org/10.1016/j.arbres.2020.07.024
Spencer LM, McKeough ZJ (2019) Maintaining the benefits following pulmonary rehabilitation: achievable or not? Respirology 24(9):909–915. https://doi.org/10.1111/resp.13518
Spruit MA et al (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 188(8):e13–e64
Steel K, Cox D, Garry H (2011) Therapeutic videoconferencing interventions for the treatment of long-term conditions. J Telemed Telecare 17(3):109–117. https://doi.org/10.1258/jtt.2010.100318
Stephenson M et al (2020) Chapter 12: systematic reviews of measurement properties. In: Aromataris E, Munn Z (eds) JBI manual for evidence synthesis. JBI, Adelaide. https://doi.org/10.46658/JBIMES-20-13
Tabak M, Vollenbroek-Hutten MMR, van der Valk P, van der Palen J, Hermens HJ (2014) A telerehabilitation intervention for patients with Chronic Obstructive Pulmonary Disease: a randomized controlled pilot trial. Clin Rehabil 28(6):582–591. https://doi.org/10.1177/0269215513512495
van Wetering CR, Hoogendoorn M, Mol SJ, Rutten-vanMolken MP, Schols AM (2010) Short- and long-term efficacy of a community-based COPD management programme in less advanced COPD: a randomized control trial. Thorax 65(1):7–13. https://doi.org/10.1136/thx.2009.118620
Vasilopoulou M et al (2017) Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J 49:1602129. https://doi.org/10.1183/13993003.02129-2016
Vestbo J et al (2013) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187:347–365. https://doi.org/10.1164/rccm.201204-0596PP
Vickerstaff V, Ambler G, Omar RZ (2021) A comparison of methods for analysing multiple outcome measures in randomised controlled trials using a simulation study. Biom J 63:599–615. https://doi.org/10.1002/bimj.201900040
Vorrink SNW, Kort HSM, Troosters T, Zanen P and Lammers JW (2016) Efficacy of an mHealth intervention to stimulate physical activity in COPD patients after pulmonary rehabilitation. Eur Respir J 48(4):1019–1029. https://doi.org/10.1183/13993003.00083-2016
Wijkstra PJ, Ten Vergert EM, van Altena R, et al (1995) Long term benefits of rehabilitation at home on quality of life and exercise tolerance in patients with chronic obstructive pulmonary disease. Thorax 50:824-828
Wootton SL, Hill K, Alison JA, Ng LWC, Jenkins S, Eastwood PR, Hillman DR, Jenkins C, Spencer L, Cecins N, Straker L, Mckeough ZJ (2017) Effects of ground-based walking training on daily physical activity in people with COPD: a randomised controlled trial. Respir Med 132:139–145
Wootton SL et al (2018) Effect on health-related quality of life of ongoing feedback during a 12-month maintenance walking programme in patients with COPD: a randomized controlled trial. Respirology 23:60–67. https://doi.org/10.1111/resp.13128
Zanaboni P, Dinesen B, Hjalmarsen A, Hoaas H, Holland AE, Oliveira CC, Wootton R (2016) Long-term integrated telerehabilitation of COPD patients: a multicentre randomised controlled trial (iTrain). BMC Pulm Med 16(1):1–9. https://doi.org/10.1186/s12890-016-0288-z
Zanaboni P, Hoaas H, Aarøen Lien L, Hjalmarsen A, Wootton R (2017) Long-term exercise maintenance in COPD via telerehabilitation: a two-year pilot study. J Telemed Telecare 23:74–82
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
UD, MNA, UCH, and EPN worked on methodology and literature search. UD worked on conceptualisation. MNA, AIK, OUM, and CMC worked on final approval. ECA worked on composition of manuscript. BA supervised the process and gave expert advice. All authors have read and approved the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA Checklist.
Additional file 2.
Search strategy.
Additional file 3.
Data extraction form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uche-Okoye, D., Ajemba, M.N., Amy, B. et al. Is telerehabilitation an effective maintenance strategy for patients with chronic obstructive pulmonary diseases: a systematic review. Bull Natl Res Cent 47, 13 (2023). https://doi.org/10.1186/s42269-023-00980-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-023-00980-8