Abstract
Background
Supraclavicular block is a common technique for analgesia for upper limb surgeries. Because of short duration of analgesia with bupivacaine alone various additive have been used to prolong the action of bupivacaine. We conducted a prospective, randomized, double blind controlled trial. All patients were assessed for onset and duration of sensory and motor block, and postoperative pain relief.
The present study was aimed to evaluate the efficacy of intravenous dexamethasone with supraclavicular block for prolongation of analgesia in patients posted for upper limb surgeries.
Results
Fifty patients belonging to American Society of Anesthesiologist physical status I–II were divided into two groups (25 in each). A mixture of bupivacaine 0.5% (15 ml) + lignocaine-adrenaline 1.5% (15 ml) were given in both the groups by ultrasound guided supraclavicular block and 2 ml of IV normal saline in group C and 2 ml (8 mg) of IV dexamethasone in group D were given. The mean onset time of sensory and motor block was 8.68 ± 1.81 min and 11.12 ± 1.58 min in group D and 11 ± 2.34 min and 13.2 ± 1.65 min in group C respectively. The duration of sensory and motor block in group D (843.6 ± 62.56 and 576.8 ± 70.40) min were prolonged than to group C (281.28 ± 22.42 and 204.2 ± 12.96) min where P < 0.0001.The duration of analgesia in group D was (895.6 ± 43.98 min) as compared to group C (324.4 ± 27.36 min). At the end of 4 h, the difference of the mean VAS score was statistically significant in both the groups (P < 0.05). There was no statistically significant difference in heart rate and systolic blood pressure in both the groups.
Conclusions
Intravenous dexamethasone significantly prolong the duration of analgesia in supraclavicular block without the side effects.
Similar content being viewed by others
Background
Supraclavicular block is an inexpensive technique and provides a safe as well as better intraoperative and postoperative analgesia (Pathak et al. 2012; Golwala et al. 2009; Talukdar et al. 2013). Supraclavicular brachial plexus block is widely used peripheral neural blocks for upper extremity, for anesthesia, and perioperative pain management (Murphy 2000).
Due to short duration of action of local anesthetics alone, various additives are used to prolong the duration of block (Wakhlo et al. 2009). Various studies had used perineural and intravenous dexamethasone for prolongation of analgesia in supraclavicular block (Mathew et al. 2019; Dhanger et al. 2016).
Dexamethasone reduces the prostaglandin production responsible for inflammation and pain via inhibiting synthesis of cyclooxygenase-2 in the peripheral tissues and central nervous system (Hong et al. 2010).
We evaluated the postoperative analgesia, intraoperative hemodynamic changes and any side effects by using intravenous dexamethasone in supraclavicular block in patients undergoing upper limb surgery.
Methods
After obtaining the Institutional Ethical Committee approval [Reference number 29/2019, dated 11/3/2019] and written informed valid consent, this prospective and experimental study was conducted in the orthopedic operation theater in our institute, between 1st April 2019 and 30th April 2020.
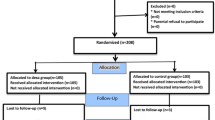
Consort flow diagram
Patients were randomized using computer-generated random number into two groups (25 in each group). A local anesthetic mixture, containing 0.5% bupivacaine (15 ml) and 1.5% lignocaine-adrenaline (15 ml) was used for ultrasound guided supraclavicular block in both the groups.
Group C—control group: IV normal saline (2 ml).
Group D—dexamethasone group: IV dexamethasone 8 mg (2 ml).
Inclusion criteria
-
Age between 18 and 60 years
-
Both male and female
-
ASA grade 1 and 2
-
Posted for elective upper limb surgery
Exclusion criteria
-
Patient refusal
-
Patient with h/o bleeding diathesis
-
Infection at the site of block
-
Psychological disorder
-
Allergic reaction to local anesthetics
Preoperative assessment of the patient including history, general examination and systemic examination with all baseline investigations were done before operation. The procedure, advantages, disadvantages were explained to the patient and patient’s relatives.
In operation theatre, all standard monitors including electrocardiogram, non-invasive blood pressure measurement, pulse oxymetry, and temperature were applied. An intravenous assess was secured with 18G or 20 G IV cannula. All patients were premedicated with inj. glycopyrollate 0.2 mg and inj. ondensetron 4 mg intravenously. No sedative agent was administered.
Patients of group C were given NS (2 ml) and patient of group D were given dexamethasone 8 mg (2 ml) intravenously just before giving the supraclavicular brachial plexus block. Patient was positioned to lie in supine with head turned to the opposite side and kept pillow under shoulder. Under aseptic precautions, supraclavicular block was performed by SonoSite M-Turbo USG machine (Sonosite Inc., Bothell, WA, USA) and a 6–13 MHz linear probe with 22 Gauge 5 cm block needle (Stimuplex) was directed to the bundle of hypoechoic round nodules of brachial plexus just posterior and superficial to the subclavian artery and drug was injected. The anesthesiologist providing the IV test drug together with anesthesiologist responsible for the intra and postoperative evaluation were blinded to the identity of the IV drug used.
Patients were assessed at 5 min intervals for 15 min for the development of sensory and motor block. Sensory block was assessed by pinprick method using a blunt 24 G needle along the course of all four major peripheral nerves and graded as.
-
0 = no block (normal sensation)
-
1 = partial block (decreased sensation)
-
2 = complete block (no sensation).
The onset of motor block was considered to the inability of the patient to move his/her fingers or raise hand.
Motor block was assessed by Modified Bromage scale for upper limb and graded
-
0 = full motor power
-
1 = decrease motor power with ability to move the finger only
-
2 = complete motor block with inability to move fingers
Intra-operatively, no analgesic was supplemented.
During surgery, adequate analgesia was assessed by hemodynamic stability, as indicated an increase in heart rate and systolic blood pressure of no more than 15% compared with baseline values obtained just before the surgical incision. An increase in heart rate and systolic blood pressure within 20 min of skin incision indicated failure of block.
The duration of analgesia was assessed by using visual analog scale (VAS) for postoperative pain every hourly for the first 10 h and then every two hours for the next 24 h.
The VAS score > 4 was considered to wear off the analgesic action of the block and injection tramadol 50 mg IV was given as rescue analgesia.
The duration of motor block was considered as the time when the patient was able to move his/her fingers and raise hand.
General anaesthesia was supplemented when the block was inadequate or failed. These cases were not included in the study.
Statistical analysis
In this study, sample size was calculated using formula n = 4pq/E2 which is based on Hardy-Weinbergg principle. In this formula, p is the prevalence of upper limb surgery at our institute.
Statistical analysis was carried out using Microsoft Office Excel 2010 and GraphPad Prism 6.05 (QuickCalc) software (GraphPad Software Inc., La Jolla CA, USA). The analysis of quantitative data was done by using chi-square test with Yates’s correction and Fisher’s exact test (two tailed). The analysis of qualitative data was done by using student’s unpaired’-test. P < 0.05 was considered to be statistically significant.
Results
Twenty-five patients were included for analysis in each group. No statistically significant difference was observed in both the groups regarding age, sex, weight, ASA grade, duration of surgery, and site of surgery (P > 0.05) (Tables 1 and 2).
Primary outcome of study
Onset of sensory and motor block
Time to onset of sensory block was 8.68 ± 1.81 min in group D and 11.0 ± 2.34 min in group C. Time to onset of motor block was 11.12 ± 1.58 min in group D and 13.2 ± 1.65 min in Group C. Onset of action for sensory and motor blockade was significantly earlier in group receiving IV dexamethasone than those not receiving IV Dexamethasone (P < 0.05) (Fig. 1).
Duration of analgesia
Statistically significant difference was observed to prolong duration of analgesia in group D, 12–16 h (mean 895.6 ± 43.98 min) compared to group C, 4–5 h (mean 324.4 ± 27.36 min) (P < 0.001) (Fig. 2).
Duration of sensory and motor block
The duration of sensory and motor block in group D (843.6 ± 62.56 and 576.8 ± 70.40) min were prolonged than to group C (281.28 ± 22.42 and 204.2 ± 12.96) min where P < 0.0001 (Fig. 2).
VAS score
At the end of 4 h, the mean VAS Score was 4.0 ± 0.0 in group C, while it was 0.36 ± 0.480 (almost zero) in group D at the same time. The difference was statistically highly significant. (P < 0.001) (Fig. 3).
Secondary outcomes of the study
There was no statistically significant difference in heart rate and systolic blood pressure in both the groups (Figs. 4 and 5).
Complications
No patient in either group had any side effect or procedure related complications like nausea, vomiting, and pneumothorax, and phrenic nerve palsy, intra-arterial or intravascular placement of drug, neurotoxicity, or cardio toxicity.
Discussion
Regional anesthesia technique in the form of supraclavicular block is widely used to provide analgesia during intraoperative and postoperative period in patients undergoing upper limb surgeries. It avoids the unwanted effect of drugs used during general anesthesia (Murphy 2000), reduces the use of opioids, hospital stay, as well as cost and results in better patient satisfaction (Shrestha et al. 2003). Postoperative pain is an unpleasant outcome in any surgical operation and it may delay the functional recovery of the patients (Gan 2017).
Supraclavicular brachial plexus block is widely used in our institute for arm, forearm and hand surgeries because of simple, safe, and effective technique for upper limb surgery. Perineural dexamethasone provided early onset of block with longer duration of analgesia (Golwala et al. 2009). In another study, it was found to reduce overall pain scores and analgesic requirements with preoperative use of oral as well as IV dexamethasone (Elhakim et al. 2003).
Dexamethasone sodium phosphate is water soluble, so safe for parenteral use. Dexamethasone, synthetic glucocorticoids has a potent anti-inflammatory and immunosuppressant property (Barnes 1998). Analgesic mechanism of dexamethasone may be due to inhibition of synthesis of cyclooxygenase and lipo-oxygenase in peripheral tissues and central nervous system, thus reducing prostaglandin production, plays a main role for pain and inflammation (Hong et al. 2010). In addition, dexamethasone decreases bradykinin also responsible for pain in the inflamed tissues and operated area. According to other theory, analgesic property of dexamethasone may be alteration in the function of potassium channels in the excitable cells by blocking transmission of nociceptive myelinated type C fibers and suppressing ectopic neuronal discharge (Johansson et al. 1990).
Pathak et al. (Pathak et al. 2012) and Shreshtha et al. (Shrestha et al. 2003) had used 8 mg of perineural dexamethasone and found prolongation of the duration of analgesia. Similarly, some studies had reported that intravenous dexamethasone also increases the duration of analgesia in supraclavicular block (Dhanger et al. 2016; Saba and Bhalotra 2020).
Some authors had observed equally prolonged duration of analgesia with 8 mg of perineural and intravenous dexamethasone (Mathew et al. 2019; Aliste et al. 2017; Abdallah et al. 2015).
There is controversy about the dose and route of dexamethasone. Perineural dexamethasone may be more prone for peripheral neurotoxicity in vitro studies (Williams et al. 2011). However, in some studies perineural dexamethasone has been used without any neurotoxicity (Pathak et al. 2012; Shrestha et al. 2003). Single dose of intravenous dexamethasone is widely used for prophylaxis to prevent nausea and vomiting without any systemic toxicity (Elhakim et al. 2003).
In a study, single dose of 10 mg of intravenous dexamethasone has been found effective to prolong the duration of analgesia of supraclavicular block without any systemic toxicity (Saba and Bhalotra 2020).
Hence in our study, we used dose of 8 mg of intravenous dexamethasone along with supraclavicular block. In our study, we found statistically significant difference in onset of sensory block and motor block in group D (8.68 ± 1.81, 11.12 ± 1.58) min and in group C (11.0 ± 2.34, 13.2 ± 1.65) min (P < 0.05). However, Mathew et al. (Mathew et al. 2019) found that patients receiving 8 mg perineural dexamethasone with 25 ml of 0.5% bupivacaine had faster onset of sensory and motor blockade than in patients receiving 8 mg of intravenous dexamethasone with 25 ml of 0.5% bupivacaine in supraclavicular block.
In our study, we also compared the total duration of sensory and motor block in both the groups. The duration of sensory block in group D 843.6 ± 62.56 min was longer as compared to 281.28 ± 22.42 min in group C (P < 0.0001). The motor block in group D was 576.8 ± 70.40 min as compared to 204.2 ± 12.96 min in group C which was also highly significant (P < 0.0001).
Dhanger et al. (Dhanger et al. 2016) had used 2 mg of intravenous dexamethasone with 25 ml of 0.5% bupivacaine and had showed that the mean duration of motor block in group D was 6.12 ± 0.48 h to 4.33 ± 0.47 h in group C (P < 0.05). Godbole et al. (Godbole et al. xxxx) used 0.05 mg/kg of perineural and intravenous dexamethasone with mixture of local anesthetic agents and reported the total duration of motor block was significantly prolonged in BD group 12 ± 2.11 h as compared to BI group 7.17 ± 0.95 h (P < 0.001).
In our study, the duration of motor block was 9–10 h in group D with mixture of local anesthetic agents which was prolonged than other study. Both low (2–4 mg) and high doses (8–10 mg) of intravenous dexamethasone used with local anesthetic agents provided longer duration of motor block.
Mathew et al. (Mathew et al. 2019) found that the duration of analgesia in group DP was 817.2 ± 88.011 min to 858.00 ± 86.168 in group DI and difference was found statistically not significant with a P = 0.104. Similarly Abdallah et al. (Abdallah et al. 2015) and Desmet et al. (Desmet et al. 2013) found comparable results with 8 mg and 10 mg dexamethasone by IV and perineural route in supraclavicular block in terms of prolong duration of analgesia. However in our study, the duration of analgesia in group D was 895.6 ± 43.98 min and 324.4 ± 27.36 min in group C. This difference was found to be statistically significant (P < 0.001).
However, Godbole et al. (Godbole et al. 2019) suggested that low-dose perinueral dexamethasone, when used in supraclavicular block significantly, provides longer duration of analgesia as against IV dexamethasone after supraclavicular block.
Meta-analysis done by Bei et al. (Bei et al. 2021) of twelve RCTs with 1345 patients concluded that perineural dexamethasone is better to IV dexamethasone for prolonging the duration of analgesia, sensory block and motor block. In a meta-analysis done by Baeriswyl et al. (Baeriswyl et al. 2017) in approximately 900 patients, it was concluded that when perineural dexamethasone added with bupivacaine but not with ropivacaine mildly prolong the duration of analgesia as compared to intravenous dexamethasone, without affecting other secondary pain related outcomes.
Abdallah et al. (Abdallah et al. 2015) had not observed steroid induced hyperglycemia but found prolong duration of analgesia up to 25 h with 8 mg IV dexamethasone along with long-acting local anesthetic agents in supraclavicular block. Desmet et al. (Desmet et al. 2013) had noticed prolonged duration of analgesia up to 21 h in supraclavicular block with 10 mg IV dexamethasone and association of more incidence of hyperglycemia.
In our study, we found that 8 mg IV dexamethasone with mixture of local anesthetic agents in supraclavicular block prolongs the duration of analgesia up to 15 h respectively but did not notice steroid induced hyperglycemia.
Limitations
Firstly, our findings are limited to the lignocaine-bupivacaine mixture only, future studies are needed for some other local anesthetic drugs. Secondly, it is not yet clear that dose of 8 mg of intravenous dexamethasone or concentration of local anesthetic mixture play a role to prove efficacy of dexamethasone. Third, direct comparison trials between perineural and intravenous dexamethasone administration would also provide clue regarding the better route of administration with possible mechanism of action of this additive.
Conclusions
When a single dose of 8 mg intravenous dexamethasone is administered along with ultrasound guided supraclavicular brachial plexus block using lignocaine-bupivacaine mixture results in prolongation of the duration of analgesia with early onset of sensory and motor block following upper limb surgery without any adverse effects.
Availability of data and materials
The data used/analyzed during this study are available from corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiology
- IV:
-
Intravenous
- USG:
-
Ultrasound
- NS:
-
Normal saline
- G:
-
Gauge
- VAS:
-
Visual analog score
- RCT:
-
Randomized control trial
References
Abdallah FW, Johnson J, Chan V, Murgatroyd H, Ghafari M, Noam Ami N et al (2015) Intravenous dexamethasone and perineural dexamethasone similarly prolong the duration of analgesia after supraclavicular brachial plexus block: a randomized, triple-arm, double-blind, placebo-controlled trial. Reg Anesth Pain Med 40:125–132. https://doi.org/10.1097/AAP.0000000000000210
Aliste J, Leurcharusmee P, Engsusophon P, Gordon A, Michelagnoli G, Sriparkdee C et al (2017) A randomized comparison between intravenous and perineural dexamethasone for ultrasound-guided axillary block. Can J Anesth 64:29–36. https://doi.org/10.1007/s12630-016-0741-8
Baeriswyl M, Kirkham KR, Jacot-Guillarmod, Albrecht E (2017) Efficacy of perineural vs systemic dexamethasone to prolong analgesia after peripheral nerve block: a systematic review and meta-analysis. British Journal of Anaesthesia 119(2):183–91. https://doi.org/10.1093/bja/aex191
Barnes PJ (1998) Anti inflammatory actions of glucocorticoids: molecular mechanisms. Clin Sci (lond) 94(557):72. https://doi.org/10.1042/cs0940557
Bei T, Liu J, Huang Q, Wu J, Zhao J (2021) Perineural versus intravenous dexamethasone for brachial plexus block: a systematic review and meta-analysis of randomized controlled trials. Pain Physician 24:E693–E707
Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H et al (2013) I.V. and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: a prospective, randomized, placebo-controlled study. Br J Anaesth 111:445–52. https://doi.org/10.1093/bja/aet109
Dhanger S, Vaidyanathan B, Rajesh IJ, Vinayagam S, Bahurupi Y, Vimalraj D (2016) Efficacy of low dose intravenous dexamethasone for prolongation of analgesia in supraclavicular block: randomized controlled trial. Indian J Pain 30:194–197. https://doi.org/10.4103/0970-5333.198059
Elhakim M, Ali NM, Rashed I, Riad MK, Refat M (2003) Dexamethasone reduces postoperative vomiting and pain after paediatric tonsillectomy. Can J Anaesth 50(392):7
Gan TJ (2017) Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J Pain Res 10(2287):98. https://doi.org/10.2147/JPR.S144066
Godbole MR, Karhade SS, Parihar PP. A prospective study of comparison of analgesic efficacy of dexamethasone as an adjuvant in supraclavicular block with intravenous dexamethasone after supraclavicular block in patients undergoing forearm surgeries. Anesth Essays Res. 2019;13:31–5. https://doi.org/10.4103/aer.AER_11_19
Golwala MP, Swadia VN, Dhimar AA, Sridhar NV (2009) Pain relief by dexamethasone as an adjuvant to local anaesthetics in supraclavicular brachial plexus block. J Anaesth Clin Pharmacol 25(3):285–288
Hong JY, Han SW, Kim WO, Kim EJ, Kil HK (2010) Effect of dexamethasone in combination with caudal analgesia on postoperative pain control in day case paediatric orchiopexy. Br J Anaesth 105(506):10. https://doi.org/10.1093/bja/aeq187
Johansson A, Hao J, Sjölund B (1990) Local corticosteroid application blocks transmission innormal nociceptive C fibers. Acta Anaesthesiol Scand 34(335):8. https://doi.org/10.1111/j.1399-6576.1990.tb03097.x
Mathew R, Radha KR, Hema VR (2019) Effect of perineural and intravenous dexamethasone on duration of analgesia in supraclavicular brachial plexus block with bupivacaine: a comparative study. Anesth Essays Res 13:280–283
Murphy DB (2000) Novel analgesic adjuncts for brachial plexus block: a systematic review. Anaesth Anal 90:1122–1128. https://doi.org/10.1097/00000539-200005000-00023
Pathak RG, Satkar AP, Khade RN (2012) Supraclavicular brachial plexus block with and without dexamethasone. Int J Sci Res Publ 2:2250–3153
Saba S, Bhalotra AR (2020) The effect of intravenous dexamethasone on prolonging analgesia after supraclavicular brachial plexus block: a randomised controlled study. JARSS 28:267–274. https://doi.org/10.5222/jarss.2020.37450
Shrestha BR, Maharjan SK, Tabedar S (2003) Supraclavicular brachial plexus block with and without dexamethasone – a comparative study. Kathmandu Univ Med J (KUMJ) 1(158):60
Talukdar M, Begum H, Shoman MM, Khatun UHS. Anaesthetic and analgesic effects of adding dexamethasone to bupivacaine in supraclavicular brachial plexus block – a comparative study. Journal of Bangladesh College of Physicians and Surgeons. 2013; 31(1).
Wakhlo R, Gupta V, Raina A, Gupta SD, Lahori VU (2009) Supraclavicular brachial plexus block: effect of adding tramadol or butorphanol as an adjuncts to local anaesthetic on motor and sensory block and duration of postoperative analgesia. J Anaesth Clin Pharmacol 25:17–10
Williams BA, Hough KA, Tsui BY, Ibinson JW, Gold MS, Gebhart GF (2011) Neurotoxicity of adjuvants used in perineural anaesthesia and analgesia in comparison with ropivacaine. Reg Anesth Pain Med 36:225–230. https://doi.org/10.1097/AAP.0b013e3182176f70
Acknowledgements
We would like to thanks Department of Orthopaedic Surgery for kind support.
Funding
None.
Author information
Authors and Affiliations
Contributions
NS conceived of the study, wrote and drafted the manuscript, revised the final manuscript, and provided tables. KM conceived of the study, contributed to the manuscript, and contributed to the tables. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
After obtaining local ethical committee approval (B. J. Medical College & Civil Hospital, Ahmedabad, dated 11/3/2019 Reference number EC/Approval/29/2019) written and informed consent was obtained from patients/relative, all surgical procedure was done under supraclavicular block.
Consent for publication
Written informed consent was taken from all the patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Solanki, N.M., Maheshwari, K.P. Efficacy of low-dose intravenous dexamethasone for prolongation of analgesia in supraclavicular block. Ain-Shams J Anesthesiol 14, 96 (2022). https://doi.org/10.1186/s42077-022-00294-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00294-3