Abstract
Background
Spinal anesthesia is the preferred anesthetic method for elective cesarean sections (C.S.) due to considerable risks regarding airway management associated with physiological changes of pregnancy. Hypotension is reported to occur in up to 80% of spinal anesthesia cases. Many approaches have been tried to prevent spinal hypotension, e.g., fluid loading, vasopressors, or both. The aim of this prospective, randomized, double blind study is to compare the administration of intermittent i.v. boluses of norepinephrine and ephedrine to guard against the hypotensive effect of spinal anesthesia during cesarean delivery.
Methods
In the present study, 120 pregnant female undergoing elective CS were randomly divided into “group E” for ephedrine and “group N” for norepinephrine, 60 female in each group. Standard spinal anesthetic technique using 25 spinal needle under complete aseptic technique with injection of 1.8–2.2 ml of heavy bupivacaine 0.5% plus 25 μg of fentanyl according to female height. Group E will receive 10 mg of i.v. diluted ephedrine as hypotension prophylaxis, and group N will receive 16 μg as hypotension prophylaxis at the time of intrathecal block. Measurements of intraoperative episodes of hypotension and their treatment with the same dose of the studied drug in each group, incidence of intraoperative nausea and vomiting, and APGAR score of baby at 1 and 5 min will be recorded.
Results
Compared with ephedrine, norepinephrine maintained maternal blood pressure. Further, it was associated with lower numbers of hypotension episodes, but more frequency of bradycardia during cesarean delivery.
Conclusion
Norepinephrine can be used as an alternative vasopressor to maintain maternal blood pressure during spinal anesthesia for cesarean delivery, with no adverse effect on neonatal outcome.
Similar content being viewed by others
Background
Spinal anesthesia is the preferred anesthetic method for elective cesarean section in obstetric anesthesia practice. Cesarean sections (C.S.) normally require an anesthetic block at T4 level, so hypotension is reported in up to 80% of spinal anesthesia cases (Rollins and Lucero 2012).
Many approaches have been tried to prevent spinal hypotension, e.g., fluid loading, vasopressors, or both. Intravenous fluid protocols have been investigated in many trials to prevent spinal hypotension, with unsatisfactory results (Butwick et al. 2015). In order to solve this problem, investigators have turned their attention to vasopressor protocols to prevent spinal hypotension (Hasanin et al. 2019).
Conventionally, ephedrine was regarded as the first choice drug to maintain maternal blood pressure. Its sympathomimetic stimulant activity on α- and β-adrenergic receptors causes positive inotropic and chronotropic effects, but repeated administration diminishes its vasoconstrictive effect due to tachyphylaxis (Ngan Kee 2017).
Norepinephrine is a weak β-adrenergic and potent α-adrenergic receptor agonist. Therefore, it may be a more suitable option for maintaining maternal blood pressure with less negative effects on heart rate (HR) and cardiac output (Heesen et al. 2015).
This study aims to compare norepinephrine versus ephedrine in controlling hypotension in C.S. under spinal anesthesia. Primary outcome is prevention of hypotension induced by spinal anesthesia and number of incremental doses used of norepinephrine or ephedrine. Secondary outcome is adverse effects and effects on fetal outcome.
Methods
This prospective, randomized, double blind study was conducted after obtaining an approval from the research ethics committee. Written informed consent was taken from all the study participants. Clinical registration number is PACTR202003466791077. The study was carried out on 120 female patients within age range from 21 to 35 years and physical status ASA II undergoing elective C.S. The study adheres to the CONSORT guidelines and fulfills their required criteria.
Females with a known history of allergy to any of the study drugs, bleeding disorders, preeclampsia, and females with vertebral anomalies or any neurological deficits were excluded from the study. Patients were randomized into the two study groups, using computer-generated lists and sealed opaque envelopes.
Sample size
Sample size was calculated using Open Epi program version 13 and according to data from previous study done by Elnabtity and Selim (2018), according to the number of hypotensive episodes in the two studied groups assuming the power of the test to 95%, margin of error accepted to 5%, the power of test to 90%, and ratio between two groups to 1:1; 42 patients per group (total 84 patients) was the minimum sample size required to demonstrate a statistically significant difference between two groups as regards hypotensive episodes and considering the anticipated dropout rate, and 120 patients (60 patients in each group) were included in the study.
Study tools
Short beveled spinal needles of 25 G, ephedrine sulfate ampoules (25 mg in 1 ml; product of ‘Misr Company for Pharmaceuticals’), to be diluted in 5 ml normal saline (5 mg/ ml), Levophrine® ampules (norepinephrine, 4 mg in 4 ml, product of ‘Egy-Pharma Company’), to be diluted in 500 ml normal saline (8 μg/ ml).
Study procedures
Pre-operative settings
One hundred and twenty patients scheduled for elective CS were assessed preoperatively including medical history, physical examination, and laboratory investigations. Patients were randomly divided into two groups (n = 60 each):
-
Group N. Norepinephrine (n = 60) received a prophylactic bolus of norepinephrine 16 μg (2 ml) intravenous (i.v.) at the time of intrathecal block.
-
Group E. Ephedrine (n = 60) received a prophylactic bolus of i.v. ephedrine 10 mg (2 ml) at the time of intrathecal block.
Intraoperative setting
On arrival to the operating room, standard monitoring was applied to all patients (ECG, non-invasive blood pressure and pulse oximetry) and a wide pore 18-G i.v. cannula was inserted into dorsum of the hand to infuse 500 ml Ringer’s solution as a preload to all patients before starting spinal anesthesia procedure. Spinal anesthesia was performed under complete aseptic conditions using 25-G spinal needle.
-
1.
Maternal hemodynamic monitoring. Mean blood pressure (MBP) and heart rate (HR) every 2 min after spinal injection until delivery of the baby and then every 5 min till the end of the study period were recorded. The incidence of hypotension (reduction in systolic blood pressure [SBP] > 20% from baseline) was recorded. Hypotension episodes were treated with boluses (2 ml volume) of the study drugs; 10 mg ephedrine or 16 μg norepinephrine according to the study group given by an anesthesiologist who was blinded to the study. Bradycardia (defined as HR < 60 bpm) was recorded and treated with atropine 0.5 mg bolus, up to 3 mg i.v.
-
2.
Vasopressors and atropine boluses. The number (and total dose) of the boluses of vasopressors and/or atropine used was recorded and were considered the primary outcome of the study group.
-
3.
Fetal hemodynamic monitoring. Uterine artery pulsatility index (UtA-PI) and umbilical artery pulsatility index (UA-PI) were measured before spinal anesthesia (baseline) and 5 min after spinal anesthesia.
-
4.
Apgar score after delivery. Apgar score at 1 and 5 min were recorded after delivery by the attending pediatric physician.
-
5.
Incidence of nausea and vomiting. Incidence of nausea and vomiting were recorded and managed accordingly by ondansetron 4 mg i.v. given after delivery of the baby.
Statistical analysis
All collected data were analyzed and compared between both groups to identify any significant differences using Statistical Package for Social Sciences (IBM SPSS 20 for windows). The quantitative data were presented as means and standard deviations; the comparison between two groups regarding quantitative data with parametric distribution were done by using independent t test while the comparison between the two groups regarding non-parametric distribution were done by using Mann-Whitney test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p value was considered significant at the level of < 0.05.
Results
Patient’s characteristics
There were no statistically significant differences between groups as Table 1 shows.
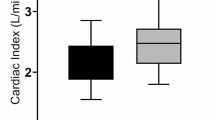
Hemodynamic variables
There was statistically significant higher MBP accompanying the use of norepinephrine while there was statistically significant higher HR with the use of ephedrine starting after 4 min and persisted for 35 min (Figs. 1 and 2).
Number of boluses of vasopressors
Patients in the ephedrine group needed more frequent boluses than those in norepinephrine group (Table 2).
Number of boluses of atropine needed
Patients in the norepinephrine group required more frequent atropine boluses than those in the ephedrine group to maintain HR above bradycardia preset level (Table 2).
Intraoperative maternal complications
While there was no statistically significant increase in the incidence of nausea among patients in the ephedrine group, there was no statistically significant increase in the incidence of vomiting in the norepinephrine group patients.
Fetal Apgar score
There were no statistically significant difference between the norepinephrine group and ephedrine group as regards fetal Apgar score variation (Table 3).
Fetal hemodynamic monitoring
While the umbilical artery Doppler pulsatility (UA-PI) indices showed non-significant changes in both studied groups when compared before and 5 min after spinal anesthesia, the uterine pulsatility indices showed significantly lower values in group N compared to group E (p < 0.001) when measured 5 min after spinal anesthesia. Furthermore, on comparing the average values of UtA-PI 5 min after anesthesia with the baseline readings in the same group, there was no significant difference in group N with p = 0.215, while in group E it significantly increased with p = 0.001 (Table 4).
Discussion
The results of the study showed that when compared with ephedrine, norepinephrine maintained maternal blood pressure with lower number of hypotension and hypertension episodes and frequency of tachycardia during cesarean delivery. Furthermore, the number of boluses of vasopressors used was lower in norepinephrine compared with the ephedrine.
Vallejo and his colleagues randomized 85 parturient who had cesarean section under spinal anesthesia to receive either phenylephrine 0.1 μg/kg/min or norepinephrine 0.05 μg/kg/min using a fixed rate infusion. They found that norepinephrine fixed rate infusion was more effective for preventing maternal hypotension (Vallejo et al. 2017). These results support the concept that was obtained in the present study although in the current study administration of the vasopressors using intermittent i.v. boluses not by a fixed rate infusion.
Onwochei et al. studied the effect of different intermittent i.v. boluses of norepinephrine to prevent maternal hypotension during spinal anesthesia for cesarean section. The results obtained were feasible as they found that effective dose of 5.8 μg by intermittent i.v. boluses was successful to maintain systolic blood pressure at or above 80% of baseline during CS under spinal anesthesia from induction of anesthesia till delivery of fetus, and were not associated with significant maternal or fetal adverse effects (Onwochei et al. 2017). These results are coinciding with the results of the present study.
Amira, in 2019, compared the use of i.v. boluses of norepinephrine (5 μg/ml) or ephedrine (5 mg/ml) for treatment of hypotension after spinal anesthesia. This study had been conducted in patients having spinal anesthesia for lower limb orthopedic surgery. The results revealed that the number of boluses of norepinephrine group were lower than ephedrine group but not statistically significant (Amira 2019), which is different from results of the present study that norepinephrine group had statistically significant lower number of boluses than ephedrine group; this difference may be attributed to the difference in the studied groups.
El Shafei et al. compared norepinephrine with ephedrine to prevent spinal anesthesia induced hypotension in coronary artery disease patients undergoing knee arthroscopy. One hundred patients were randomly allocated to two equal groups to receive either 5 mg of ephedrine or 5 μg of norepinephrine when hypotension occurs. They found that norepinephrine is more effective compared with ephedrine in the maintenance of SBP with reduction in HR, which is useful in coronary artery disease patients (El Shafei et al. 2015). These results are in agreement with the results obtained in the present study. However, they found no difference between the two groups regarding the incidence of hypotension, hypertension, and bradycardia, and this is not coincident with the results of the present study. These differences in results may be attributed to different doses of the studied drugs as they used 5 mg of ephedrine or 5 μg of norepinephrine when hypotension occurred, while in the present study used 10 mg of ephedrine or 16 μg of norepinephrine.
In 2018, Elnabtity and Selim compared norepinephrine bolus 5 μg with ephedrine bolus 10 mg for prevention of maternal hypotension during cesarean section under spinal anesthesia. They demonstrated that norepinephrine bolus group was associated with lower fluctuation of maternal blood pressure and heart rate, and less need for rescue i.v. bolus (Elnabtity and Selim 2018). Their results are coinciding with the results of the present study as regards stability of maternal pressure of norepinephrine group, in spite of different norepinephrine bolus dose as they used 5 μg norepinephrine.
Xu and colleagues compared norepinephrine infusion 4 μg/min with ephedrine infusion 4 mg/min for prevention of maternal hypotension during cesarean section under spinal anesthesia. They demonstrated that norepinephrine infusion was associated with fewer cases of tachycardia, less fluctuation in heart rate, systolic blood pressure and better fetal outcome as evident with higher base excess, and lower lactate values when compared to ephedrine infusion (Xu et al. 2019). As regards fetal outcome, the results of the present study differ from Xu and his colleagues as both norepinephrine and ephedrine groups had similar fetal outcome.
In 2019, Wang et al. (2019) compared norepinephrine bolus 4 μg with ephedrine infusion bolus 4 mg for prevention of maternal hypotension during cesarean section under spinal anesthesia but in preeclamptic. They demonstrated that norepinephrine bolus was associated with fewer episodes of bradycardia, tachycardia, with higher base excess and lower lactate values. In the present study, only bolus doses were satisfactory in both groups but it may be attributed to different female group as preeclamptic parturient were excluded from the study.
There was no significant difference between both groups regarding fetal Apgar score, which may be due to the greater cardiac output that improved uterine blood flow in norepinephrine group although there were no significant differences between both groups as regards the fetal outcome.
Conclusion
Norepinephrine can be used as an alternative vasopressor to maintain maternal blood pressure during spinal anesthesia for cesarean section, with no adverse effect on neonatal outcome.
Availability of data and materials
Confidential patient data can be asked by special request from corresponding author.
Abbreviations
- CS:
-
Cesarean section
- i.v.:
-
Intravenous
- Group E:
-
Group ephedrine
- Group N:
-
Group norepinephrine
- HR:
-
Heart rate
- BPM:
-
Beats per minute
- SBP:
-
Systolic blood pressure
- UtA-PI:
-
Uterine Artery Pulsatility Index
- UA-PI:
-
Umbilical Artery Pulsatility Index
References
Amira AE (2019) Admiistration of ephedrine versus norepinephrine for maagement of post-spinal hypotesion in lower limb orthopedic surgery. Clin Practice 8(1):1–9
Butwick AJ, Columb MO, Carvalho B (2015) Preventing spinal hypotension during Caesarean delivery: what is the latest? Br J Anaesth 114(2):183–186
El Shafei M, El Gendy H, El Fawy D (2015) Norepinephrine versus ephedrine for the prevention of spinal anesthesia-induced hypotension in coronary artery disease patients undergoing knee arthroscopy. Ain-Shams J Anaesthesiol 8(3):424
Elnabtity AM, Selim MF (2018) Norepinephrine versus ephedrine to maintain arterial blood pressure during spinal anesthesia for Cesarean delivery: a prospective double-blinded trial. Anesth Essays Res 12(1):92–97
Hasanin A, Mokhtar AM, Badawy AA, Fouad R (2019) Post-spinal anesthesia hypotension during cesarean delivery, a review article. Egypt J Anaesth 33(2):189–193
Heesen M, Stewart A, Fernando R (2015) Vasopressors for the treatment of maternal hypotension following spinal anaesthesia for elective caesarean section: past, present and future. Anaesthesia 70(3):252–257
Ngan Kee WD (2017) The use of vasopressors during spinal anaesthesia for caesarean section. Curr Opin Anaesthesiol 30(3):319–325
Onwochei DN, Ngan Kee WD, Fung L, Downey K, Ye XY, Carvalho JCA (2017) Norepinephrine intermittent intravenous boluses to prevent hypotension during spinal anesthesia for Cesarean delivery: a sequential allocation dose-finding study. Anesth Analg 125(1):212–218
Rollins M, Lucero J (2012) Overview of anesthetic considerations for Cesarean delivery. Br Med Bull 101:105–125
Vallejo MC, Attaallah AF, Elzamzamy OM, Cifarelli DT, Phelps AL, Hobbs GR et al (2017) An open-label randomized controlled clinical trial for comparison of continuous phenylephrine versus norepinephrine infusion in prevention of spinal hypotension during cesarean delivery. Int J Obstet Anesth 29:18–25
Wang X, Mao M, Liu S, Xu S, Yang J (2019) A comparative study of bolus norepinephrine, phenylephrine, and ephedrine for the treatment of maternal hypotension in parturients with preeclampsia during Cesarean delivery under spinal anesthesia. Med Sci Monit 25:1093–1101
Xu S, Mao M, Zhang S, Qian R, Shen X, Shen J et al (2019) A randomized double-blind study comparing prophylactic norepinephrine and ephedrine infusion for preventing maternal spinal hypotension during elective cesarean section under spinal anesthesia: a CONSORT-compliant article. Medicine (Baltimore) 98(51):e18311
Acknowledgements
Not applicable.
Funding
None
Author information
Authors and Affiliations
Contributions
The idea of the research belongs to AK; also, he shared in writing the manuscript. AE participated in clinical data collection and in writing the manuscript. MIS shared in clinical data collection and statistical analysis. MS shared in clinical data collection and writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MS294/2019; Ain Shams University. Written informed consent was taken from all the study participants. Clinical registration number is PACTR202003466791077.
Consent for publication
Participants accepted publication in a written consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elagamy, A.E., Kamaly, A.M., Shahin, M.I. et al. Norepinephrine versus ephedrine for hypotension prophylaxis during cesarean section under spinal anesthesia. Ain-Shams J Anesthesiol 13, 3 (2021). https://doi.org/10.1186/s42077-020-00124-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00124-4