Abstract
Background
Perioperative hypothermia is an unintended decrease in the core temperature of patients. Hypothermia has many proven complications. The aim of this study is to investigate the perioperative temperature monitoring rates and the difficulties encountered during monitoring, particularly in patients undergoing neuraxial anesthesia.
Methods
Two hundred anesthesiologists were included in the study who work in Turkey and actively work in an operating room. A questionnaire was applied to the participants via printed form or e-mail.
Results
In Turkey, the overall temperature monitoring ratio was measured as 5.5%. Temperature monitoring was the most frequently used for cardiovascular surgery patients group. In neuraxial anesthesia, temperature monitoring was only 1.5%. The most common reason for not using a temperature monitor was the lack of appropriate equipment (45%). The most common temperature monitoring area was the axillary zone (48%).
Conclusion
Participants were aware of the importance of temperature monitoring but concluded that it was not sufficient in practice. Where and how to measure core temperature in awake patients is a controversial issue. Furthermore, the accuracy of measurements in neuraxial anesthesia should be discussed. Interestingly, raising awareness about this issue was not effective in the resolution of the problem. Still, in order to keep this issue up to date, the importance of perioperative temperature monitoring should be emphasized more frequently in anesthesia meetings and education programs.
Similar content being viewed by others
Background
Perioperative unintended hypothermia is defined as core temperature falls under 36° between preoperative 1 h and postoperative 24 h period (Sessler 2008). As a result of perioperative hypothermia, the patient’s “thermal comfort” is impaired, oxygen consumption increases with the development of tremors, heart problems that may increase mortality may develop, blood transfusion requirement increases due to increased intraoperative blood loss, the incidence of infection in the surgical wound site increases, and the incidence of postoperative nausea vomiting increases. In addition, the duration of action of hypnotic drugs and neuromuscular blockers is prolonged, and the recovery time after anesthesia is extended (Turkish Society of Anesthesiology and Reanimation (TSAR) 2013). Depending on the results, long-term hospital stay and all complications lead to an increase in mortality, morbidity, and cost (Hart et al. 2011; Billeter et al. 2014).
Although conduction, convection, and evaporation are effective in heat loss, the primary mechanism is radiation (Sessler 2016). Heat loss is commonly seen in patients with general and regional anesthesia combined (Arkiliç et al. 2000; Macario and Dexter 2002). The temperature mentioned in perioperative hypothermia is the core temperature of the patient. It is practical and easier to measure the core temperature in patients under general anesthesia. But this is a challenge in patients undergoing neuraxial anesthesia.
Redistribution via peripheral vasodilatation under spinal anesthesia is already expected (Matsukawa et al. 1995). However, its effects often overlooked. In fact, neuraxial anesthesia patients may be more hypothermic than we think (Allen and Habib 2018). In our study, the attitudes and behaviors of anesthesiologists in general anesthesia and especially in neuraxial anesthesia to prevent perioperative hypothermia were examined.
Material and methods
After the approval of the ethics committee of Bozok University (2017-KAEK-189_2019.01.02_18), 200 anesthesiologists who work in Turkey and actively work in an operating room were included in the study. Informed consent for participation was obtained from all participants. Since the personal data were not published, the consent for publication was not applicable. More than 2000 anesthesiologists and residents are working in Turkey (Turkish Society of Anesthesiology and Reanimation (TSAR) n.d.-b). The number 200 in our study was adjusted to represent about 10% of 2140 anesthesiologists. For our study, a 30-day survey filling period was applied.
The questionnaire includes 3 chapters consisting of a total of 19 questions. These sections aim to measure general approaches to perioperative hypothermia, approaches at neuraxial anesthesia, and attitudes related to measurement techniques. Survey questions are presented in Table 1. In this study, neuraxial anesthesia expression was used for spinal, epidural, and combined spinal-epidural anesthesia applications. The surgical procedures were classified as major and minor. If a mesenchymal barrier is opened (pleural cavity, peritoneum, meninges), the surgery is considered major (Solimeno et al. 2018).
Statistical methods
The minimum number of participants for our study was determined as 200 by power analysis with taking into consideration the previous studies on this subject (İnal et al. 2017). Data obtained in the study were analyzed statistically using the Statistical Package for the Social Sciences software package (SPSS version 20.0, IBM). Data collected were analyzed, and the results expressed as percentages. Our results were compared with previous studies conducted in Turkey and different countries and the current literature.
Results
In our survey period, 221 participants completed the questionnaire. Twenty-one of them have been excluded because of missing answers. Forty-one and a half percent of the participants were specialist physicians, 36% were research assistants, and 22.5% were academic staff. The average experience of anesthesia was between 5 and 8 years.
Only 5.5% of the participants stated that they performed routine temperature monitoring for each patient. Those who performed temperature monitoring according to the patient group was 68%. However, 41% of the respondents thought that patients who were not followed up were hypothermic at the end of the operation.
The most frequent monitoring was performed in cardiovascular surgery patients with a rate of 87.5%. This was followed by pediatric patients (25.4%), major surgeries (19.3%), and surgeries longer than 30 min (14%). Geriatric patients were monitored with a rate of 6.5% (Fig. 1).
The nasopharynx was the most commonly used site for core temperature measurement in patients under general anesthesia with 71.5%. It was followed by the tympanic membrane with 34%. The least used were pulmonary arterial catheter and rectal measurements (Table 2). In patients who underwent neuraxial anesthesia, the most common temperature monitoring area was the axilla (48%). It was followed by the forehead (30%), tympanic membrane (26%), and chest skin 12% (Table 2).
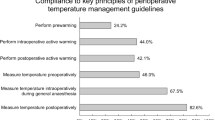
Our participants thought that temperature monitoring is a part of standard monitoring with a rate of 58% of the respondents. However, the rate of temperature monitor usage in neuraxial anesthesia was 1.5%. The participants who did not conduct temperature monitoring for neuraxial anesthesia patients indicated that the most frequent reason was the lack of equipment (45%). Twelve percent of the participants believe that temperature monitoring for neuraxial anesthesia patients was unnecessary. Another important reason was to believe that it was a waste of time (15%). In contrast with the results, 30% of the participants stated that they always adhere to the guidelines.
Discussion
Perioperative hypothermia may cause many complications such as delayed recovery from anesthesia, increased coagulopathy, increased risk of infection, and increased cardiovascular complications (Díaz and Becker 2010).
Consistent with the previous studies in this area, our survey participants did not routinely use temperature monitoring for each patient (Allen and Habib 2018; Frank et al. 1999; Alluri and Wrench 2014). Even so, 58% of the respondents thought that temperature monitoring is a part of standard monitoring. The majority of the participants preferred temperature monitoring according to the characteristics of the patient group under general anesthesia. Temperature monitoring was most commonly used in cardiovascular surgery. Cooling and rewarming periods are important parts of coronary artery bypass graft surgery, so temperature monitoring is essential; 87.5% ratio temperature monitoring can be expected. Although 15% of the participants think that temperature monitoring is a waste of time, monitoring the temperature in general anesthesia will probably take less time than a delayed recovery after surgery.
For patients under neuraxial anesthesia, the most frequent reasons to not fallow temperature perioperative was the lack of equipment (45%). Even if the temperature probe is available in all operating rooms, these probes are only suitable for use in core temperature measurements under general anesthesia. Where and how to measure the core temperature in awake patients is a controversial issue. It is known that skin temperature monitoring is not an acceptable temperature monitoring (Arkiliç et al. 2000). In this case, a practical monitoring method may be needed in neuraxial anesthesia patients. Forty-five percent of the participants stated the the lack of equipment is the reason for not monitoring the temperature in neuraxial anesthesia. However, it is not clear whether the equipment mentioned here is a direct thermocouple or infrared measurement tool which is known to be unreliable. In fact, the presence of equipment that could properly monitor the temperature was perhaps an issue that should be questioned. For neuraxial anesthesia patients, most commonly used site was axilla (48%). The forehead was 30%. The tympanic membrane was 26% and chest skin 12%. For these areas, the tympanic membrane can be the most accurate site for temperature measurements. The axillary temperature measurement is only reliable if it is done with the appropriate technique (Sessler 2016). Infrared aural canal temperature measurement is insufficiently accurate for clinical use. Tympanic membrane temperature can be measured by thermocouples with high accuracy (Merry et al. 2010). Alternatively, a double-sensor thermometer can be used to measure the temperature. It has been emphasized in some studies that the double-sensor thermometer is significantly correlated with core temperature and is an alternative measurement method in neuraxial anesthesia patients (Kimberger et al. 2013). In our survey questions, 45% of the participants emphasized the lack of appropriate equipment for temperature monitoring in patients under neuraxial anesthesia. It is an accepted fact that the measurements made from the external ear by infrared methods are also considered to be low reliability. At this point, it should be mentioned the spot-on core temperature monitor, which has started to be used recently. This device measures from the skin with an adhesive tape, and according to studies, it has a high correlation with the core temperature values. Its use is practical and accurate, especially in patients who are awake, such as neuraxial anesthesia patients, whose internal temperature is difficult to measure (Eshraghi et al. 2014; Boisson et al. 2018).
There was no information on the technique used by the respondents to measure the tympanic membrane. Therefore, we have no idea how much temperature is accurately measured in patients undergoing neuraxial anesthesia. Despite all difficulties, temperature monitoring in neuraxial anesthesia with an acceptable method will reduce the complication rates.
European and American Society of Anesthesiologists guidelines recommended the routine use of temperature monitoring (National Institute for Care and Health Excellence 2008; American Society of Anesthesiologists Guidelines 2015). The Turkish Anesthesia Society recommends the use according to the patient group. It recommends the use in risky patient groups even in operations lasting less than 30 min (Turkish Society of Anesthesiology and Reanimation (TSAR) 2013).
Arkiliç et al. (2000) Investigated hypothermia in neuraxial anesthesia in 120 patients. Seventy-seven percent of these patients were found to be hypothermic. Even in 22%, core temperature was found to be < 35 °C. These results emphasize the high rate of hypothermia in neuraxial anesthesia. The rate of temperature monitor usage in neuraxial anesthesia was found to be 1.5% in our study. This rate was 27% in Arkiliç’s study. In a survey conducted in European countries, the use of temperature monitors was found to be 25% in general anesthesia and 6% in neuraxial anesthesia.
There are a limited number of previous studies on the rate of temperature monitoring in Turkey. In a study conducted in 2017, 26% of the participants stated that they always use temperature monitoring (İnal et al. 2017). In this study, there was no data on the use of temperature monitoring in patients under neuraxial anesthesia. However, we found this rate to be 5.5% under general anesthesia and 1.5% at neuraxial anesthesia. These rates are less than the results of Frank’s survey in 1999. In this study, the rate of conducting temperature monitoring in the USA under regional anesthesia was found to be 33% (Frank et al. 1999). These results show that there has been no improvement in the behavior of anesthesiologists in the last 20 years. This issue should be considered by anesthesiologists.
Limitations
Although the results of our study are similar to those conducted across Europe, the number of participants in this study may not reflect the attitudes of all anesthesiologists in Turkey. However, still it is important to be informative. The lack of an electronic correspondence environment accessible to all specialists made it difficult to reach more participants. With a larger number of participants, a more precise conclusion can be reached.
Conclusion
In our study, the approaches of the anesthesiologist to perioperative hypothermia in neuraxial anesthesia were investigated. It is understood that the anesthesiologists have enough idea about the guidelines and the negative effects of hypothermia. However, although 20 years have passed since important publications on the subject and national and international guidelines emphasized the importance of this issue, no improvement was observed in our approaches.
Many national and international associations have published guidelines on the prevention of perioperative hypothermia and emphasized the importance of the subject. Interestingly, raising awareness about this issue was not effective in the resolution of the problem (Merchant and Chartrand 2016; Checketts et al. 2016; Australian and New Zealand College of Anaesthetists A 2015). Still, in order to keep this issue up to date, the importance of perioperative temperature monitoring should be emphasized more frequently in anesthesia meetings and education programs.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Allen TK, Habib AS (2018) Inadvertent perioperative hypothermia induced by spinal anesthesia for cesarean delivery might be more significant than we think: are we doing enough to warm our parturients? Anesth Analg. 126(1):7–9
Alluri S, Wrench IJ (2014) Enhanced recovery from obstetric surgery: a UK survey of practice. Int J Obs Anesth.
American Society of Anesthesiologists Guidelines (2015) Standards for basic anesthetic monitoring. https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring. Accessed 28 Oct 2019.
Arkiliç CF, Akça O, Taguchi A, Sessler DI, Kurz A (2000) Temperature monitoring and management during neuraxial anesthesia: an observational study. Anesth Analg 91(3):662–666
Australian and New Zealand College of Anaesthetists A. Guidelines on monitoring during anaesthesia. monitoring equipment. 2015. Available from: http://www.anzca.edu.au/documents/ps18-2015-guidelines-on-monitoring-during-anaesthe.pdf. (Accessed July 2019).
Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC (2014) Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surg (United States). 156(5):1245–1252
Boisson M, Alaux A, Kerforne T, Mimoz O, Debaene B, Dahyot-Fizelier C et al (2018) Intra-operative cutaneous temperature monitoring with zero-heat-flux technique (3M SpotOn) in comparison with oesophageal and arterial temperature: a prospective observational study. Eur J Anaesthesiol. 35(11):825–830. https://doi.org/10.1097/EJA.0000000000000822
Checketts M, Alladi R, Ferguson K (2016) Recommendations for standards of monitoring during anaesthesia and recovery 2015: association of anaesthetists of Great Britain and Ireland. Anaesthesia. 71(1):85–93
Díaz M, Becker DE (2010) Thermoregulation: physiological and clinical considerations during sedation and general anesthesia. Anesth Prog. 57(1):25–32
Eshraghi Y, Nasr V, Parra-Sanches I, Van Duren A, Botham M, Santoscoy T et al (2014) An evaluation of a zero-heat-flux cutaneous thermometer in cardiac surgical patients. Anesth Analg. 119(3):543–549. https://doi.org/10.1213/ANE.0000000000000319
Frank SM, Nguyen JM, Garcia CM, Barnes RA (1999) Temperature monitoring practices during regional anesthesia. Anesth Analg. 88(2):373–377
Hart SR, Bordes B, Hart J, Corsino D, Harmon D (2011) Unintended perioperative hypothermia. Ochsner J. 11(3):259–270
İnal MA, Ural SG, Çakmak HŞ, Arslan M, Polat R (2017) Approach to perioperative hypothermia by anaesthesiology and reanimation specialist in Turkey: a survey investigation. Turk J Anesthesiol Reanim. 45(3):139–145
Kimberger O, Saager L, Egan C (2013) The accuracy of a disposable noninvasive core thermometer. Can J Anaesth. 60(12):1090–1096
Macario A, Dexter F (2002) What are the most important risk factors for a patient’s developing intraoperative hypothermia? Anesth Analg. 94(1):215–220
Matsukawa T, Sessler DI, Sessler AM, Schroeder M, Ozaki M, Kurz A, Cheng C (1995) Heat flow and distribution during induction of general anesthesia. Anesthesiology 82:662–673
Merchant R, Chartrand D (2016) Guidelines to the practice of anesthesia - revised edition 2016. Can J Anaesth. 63(1):86–112
Merry A, Cooper J, Soyannwo O, Wilson I, Eichhorn J (2010) International standards for a safe practice of anesthesia. Can J Anaesth. 57(11):1027–1034
National Institute for Care and Health Excellence. Hypothermia: prevention and management in adults having surgery - clinical guideline [CG65]. 2008. Available from: https://www.nice.org.uk/guidance/cg65. Accessed Apr 2019
Sessler DI (2008) Temperature monitoring and perioperative thermoregulation. Anesthesiology 109(2):318–338
Sessler DI (2016) Perioperative thermoregulation and heat balance. Lancet 387(10038):2655–2664. https://doi.org/10.1016/S0140-6736(15)00981-2
Solimeno L, Escobar M, Krassova S, Seremetis S (2018) Major and minor classifications for surgery in people with hemophilia: a literature review. Clin Appl Thromb Hemost. 24(4):549–559
Turkish Society of Anaesthesiology and Reanimation (TSAR) (2013) Practice Guideline for Prevention of Unintentional Perioperative Hypothermia. Turk J Anaesthesiol Reanim 41:188-190. https://doi.org/10.5152/TJAR.2013.64
Turkish Society of Anesthesiology and Reanimation (TSAR). (n.d.-b) Anesthesiologist numbers http://www.tard.org.tr/portal/. Accessed Sept 2019.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AY and GT contributed to the conception and design of the study. ÇÜK and CY performed the data collection and organized the data preparation. All authors actively discussed the manuscript, critically reviewed its comprehensive content, and finally approved the final version to be submitted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Bozok University Research Ethics Committee with reference no. 2017-KAEK-189_2019.01.02_18. All procedures were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The aim of the research was explained to the participants and obtained informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yüksek, A., Talih, G., Kantekin, C.U. et al. Perioperative temperature monitoring in general and neuraxial anesthesia: a survey study. Ain-Shams J Anesthesiol 12, 12 (2020). https://doi.org/10.1186/s42077-020-00065-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00065-y