Abstract
Background
This review addresses current issues from the daily practice of prostate and bladder diagnostic pathology.
Main text
In the last few years, many recommendations and clarifications were available from 2014 International Society of Urologic Pathology consensus, 2016 World Health Organization blue book and 2017 8th edition of American Joint Committee on Cancer Staging System.
Conclusion
We focus here on nine topics which are relevant based on their common appearance in daily practice, clinical relevance and need to improve communication between pathology reports and clinicians.
Similar content being viewed by others
Background
In the last few years, many recommendations and clarifications were available from 2014 International Society of Urologic Pathology consensus, 2016 World Health Organization blue book and 2017 8th edition of American Joint Committee on Cancer Staging System. We focus here on nine topics which are relevant based on their common appearance in daily practice, clinical relevance and need to improve communication between pathology reports and clinicians.
Prostate pathology
Grade groups
The Grading system originally proposed by Donald Gleason in 1966 (Gleason 1966) for prostatic acinar adenocarcinomas has been adopted worldwide and proved to be an important prognostic factor giving information to guide treatment of patients with prostate cancer. Gleason grading scheme was endorsed by World Health Organization (WHO) blue book in 2004 (Eble et al. 2004). After more than five decades since its introduction, the Gleason system maintained the original concepts of using architectural features to stratify morphologic patterns associated with prognosis and giving a score based on the primary and the secondary patterns within the tumor. Many changes, however, were incorporated in routine diagnostic practice to refine risk stratification and have been widely adopted after consensus meetings organized by the International Society of Urologic Pathology (ISUP) in 2005 and 2014 (Epstein et al. 2005; Epstein et al. 2017; Epstein et al. 2016a; Epstein 2018). In brief, patterns 1 and 2 have been abolished in needle biopsies and are now rarely reported; poorly formed glands, glomeruloid and cribriform glands are diagnostic of pattern 4; and Gleason score in biopsies are calculated by the most common pattern plus the highest pattern present in the biopsy (which is different from the score calculation in prostatectomy specimens). Because of these changes, Gleason pattern 3 is now a more uniform category both on morphology and in its indolent clinical behavior. This is an important issue in an era of growing interest on active surveillance. In contrast, Gleason pattern 4 has become a more heterogeneous group with many different possible morphologies and diverse clinical outcomes. Gleason score 3 + 4 is now the most common grade seen in prostatectomy specimens and this so-called Gleason inflation is attributed to the fact that many morphologic patterns are now considered as Gleason pattern 4 (Danneman et al. 2015). The current scenario of different morphologies and the heterogeneity of Gleason pattern 4 highlight the importance of the three topics below (high grade tumor quantification, sub stratification of Gleason pattern 4 and reproducibility of the diagnosis of poorly formed glands).
Gradual changes in Gleason system created other issues: as patterns 1 and 2 vanished from pathology reports, the score 6 (3 + 3) has become the most indolent tumor eligible for active surveillance. Patients may be confused when they are told to be in the middle of scale from 2 to 10 and yet with the most indolent tumor possible and suitable for active surveillance. Original Gleason score 7 did not split 3 + 4 and 4 + 3 tumors which have different clinical behaviors. Further sum stratifications such as 4 + 5, 5 + 4 and 5 + 5 had no meaning since all these tumors show similar clinical behavior and prognosis. Epstein and colleagues from Johns Hopkins Hospital proposed in 2013 a 5-tiered new grading system in which the categories would regroup Gleason scores ≤6 (group 1), 3 + 4 (group 2), 4 + 3 (group 3), score 8 (group 4) and scores 9 and 10 (group 5). Biochemical recurrence-free progression after prostatectomy could be easily stratified using these five groups avoiding the use of all possible combinations of Gleason scores (Pierorazio et al. 2013) and this finding was validated in an multi-institutional study (Epstein et al. 2016b). The new system has been endorsed by ISUP (Epstein et al. 2016a) and WHO blue book in 2016 (Moch et al. 2016a) with the recommendation that pathology reports should use in conjunction both the new system and the modified Gleason grade. It is believed that in the future the new system, which is simpler and more logical, will replace the Gleason scheme. After public discussion on how the new 5-tiered system should be named (Egevad et al. 2016; Epstein 2016), the terminology of grade groups (GG) has been widely applied by most authors.
High grade tumor quantification
The 2014 ISUP conference and 2016 WHO blue book recommend that tumors with Gleason score 7 should always have the percentage of Gleason pattern 4 quantified both in needle biopsy and prostatectomy specimens (Epstein et al. 2017; Moch et al. 2016a; College of American Pathologists 2018a). The major rationale in reporting percentage of Gleason pattern 4 in needle biopsy is the potential influence on clinical decision for active surveillance. In current practice on most centers, active surveillance is restricted to Gleason 3 + 3 tumors (Amin et al. 2014a). However, a selected group of patients with positive biopsy with limited extent of Gleason pattern 4 may be suitable for conservative therapy specially if extent of Gleason pattern 4 is less than 10% (Chen et al. 2016; Morash et al. 2015; Kwon et al. 2014). In addition, percentage of Gleason pattern 4 in needle biopsy improves prediction of upgrading at prostatectomy, adverse pathological findings at prostatectomy and biochemical recurrence (Cole et al. 2016; Flood et al. 2016). Although not explicit in the 2014 ISUP consensus conference, it is a widely adopted approach to report the percentage of Gleason pattern 4 only in the absence of Gleason pattern 5, since it is believed that the presence of the higher-grade component will be decisive information to guide clinical management.
The same recommendation for high grade tumor quantification is made for prostatectomy specimens. There is no specific method of quantification, however, that has been recommended or widely adopted. The combined percentage of Gleason patterns 4 and 5 within the tumor has been linked to higher stage, adverse pathological findings, metastases and was an independent predictor of cancer-specific survival (Chen et al. 2016). Two large studies showed a continuous increase of the risk of prostate-specific antigen recurrence with increasing percentage of Gleason 4 fractions advocating that such information is much more discriminatory than the 2-tired distinction of 3 + 4 and 4 + 3 tumors (Athanazio et al. 2014; Choy et al. 2016).
A different approach is to report not the percentage of high grade component within the tumor, but the extent of high grade component in the prostate gland. The use of Gleason score, or grade groups, may lead to a misinterpretation on the actual extent of low- and high-grade components within the prostate. In a recent series of prostatectomy specimens, one of the authors and colleagues showed that a considerable rate of GG2 (GS 3 + 4) tumors do indeed have more extensive Gleason pattern 4 than GG3 (4 + 3) tumors: 22.8% of GG2 carcinomas at prostatectomy showed higher percentage of the prostate involved by high grade tumor than the first-quartile value of GG3 tumors, and 20.2% of GG2 carcinomas at prostatectomy showed higher volume of high grade tumor than the first-quartile value of GG3 tumors (Souza et al. 2018). Detailed data on the distribution is seen in Table 1 and show considerable superposition between values of percentage of prostate gland involvement and total volume of high grade component among GG2 and GG3 tumors, especially among intermediate positions (higher quartiles of GG2 and lower quartiles of GG3) (Souza et al. 2018).
A recent report by Deng and colleagues reports a size-weighted Gleason score (prostate gland weight × % gland with tumor × % of Gleason pattern 4%), which is expressed in grams and has proven to be a better predictor of biochemical recurrence than the traditional Gleason score. In this report, percentage was assessed by slide drawing and semiquantitative estimation (Deng et al. 2016). Chun and colleagues used a semiquantitative calculation of high-grade tumor volume – based on estimation of percentage per slice and slice thickness – showed that this parameter was an independent predictor of biochemical recurrence in high-risk tumors (Chun et al. 2007). In our practice, we use a modified point count method which allows estimation of percentage of prostate gland involvement both of total tumor and the high grade component (Athanazio et al. 2014; Souza et al. 2018). Such approach avoids the inherit subjectivity of eyeballing and does not add considerable time consuming to tumor quantification. Knowing the prostate volume, the total tumor volume and high-grade tumor component can also be estimated. All of our synoptic pathology reports of radical prostatectomy specimens includes the quantitative information of total tumor volume, percentage of the prostate involved by total tumor, high-grade tumor component volume and percentage of the prostate involved by the high-grade component. We believe this approach is more informative than merely reporting the percentage of high grade patterns within the tumor. Such quantitative information in pathology reports of prostatectomy specimens is of relevance since in the case of prostate cancer most tumors are not grossly identified and are usually multifocal precluding gross estimation of size or identification of index tumor.
Sub stratification of Gleason pattern 4
As mentioned before, the currently used modified Gleason grading is associated with Gleason “inflation”, which means that Gleason pattern 4 is more diagnosed in current practice than before both in needle biopsies and prostatectomies. Gleason score 3 + 4 is now the commonest grade seen in radical prostatectomy specimens and the clinical outcome of this group is heterogeneous. Tumors with Gleason 3 + 4 grade in needle biopsies may be eligible to active surveillance, however, there is a urgent new of consistent predictors of outcome in this settings.
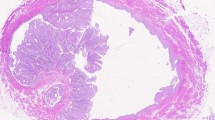
Current accepted morphologies of Gleason pattern 4 includes poorly formed glands (Fig. 1a), cribriform glands (Fig. 1b), glomeruloid glands, fused glands, and ductal invasive carcinoma (Fig. 1). The commonest morphologies detected at needle biopsies are poorly formed glands (57%), fused glands (53%) and cribriform glands (25%) (Gottipati et al. 2012). Such heterogeneity in morphology and clinical outcomes urge new strategies of sub stratification of Gleason pattern 4.
Although it is not a formal recommendation in 2014 ISUP consensus or 2016 WHO blue book, it became common practice to include in pathology reports whether cribriform morphology is present or absence in Gleason pattern 4. Cribriform morphology evolved through decades from acceptable in Gleason pattern 3 to diagnostic of Gleason pattern 4, and now emerges as a subgroup of more aggressive behavior among Gleason pattern 4 morphologies. In patients who underwent radical prostatectomy, cribriform morphology has been an independent predictor of biochemical recurrence (Iczkowski et al. 2011; Kir et al. 2014; Trudel et al. 2014; Dong et al. 2013), metastasis (Dong et al. 2013; Kweldam et al. 2015) and cancer specific death (Kweldam et al. 2015).
A large European study enrolling 1031 subjects showed that 15-year cancer free survival after a diagnosis at needle biopsy of Gleason score 6, score 7 without cribriform invasive or intraductal carcinoma, and score 7 with cribriform invasive or intraductal carcinoma were 99%, 94% and 64%, respectively. Cribriform invasive or intraductal carcinoma were independent predictor of cancer free survival (Kweldam et al. 2016a). The same group has shown that the presence of these features in needle biopsies after prostatectomy, but not percentage of Gleason pattern 4, was an independent predictor of biochemical recurrence. This observation favors the inclusion of the information on the presence of cribriform morphology and intraductal carcinoma in pathology reports of needle biopsies. In addition, it demonstrates that presence of any amount of cribriform morphology should rule out the option of the active surveillance patient management (Kweldam et al. 2017). Strikingly, men with Gleason score 7 and no cribriform invasive or intraductal carcinoma had indistinguishable cancer free survival curves from those men with Gleason score 6 after radical prostatectomy or radiotherapy – a finding supporting the use of absence of this parameter as an important eligibility criteria for including 3 + 4 patients in active surveillance, as long as serum PSA levels and tumor extent are favorable (Kweldam et al. 2016b).
The approach of Kweldam and colleagues to aggregate invasive cribriform and intraductal carcinoma is explained by the fact that both are implicated in aggressive behavior and are usually a mutual differential diagnosis. Intraductal carcinoma (discussed below) usually grows in a dense cribriform pattern with dilated ducts and the distinction from invasive cribriform masses with round contours can only be achieved by immunohistochemical evidence of preserved basal cells. Such strategy avoids the requirement of immunohistochemistry for all cases showing cribriform morphology.
Interestingly, a cytogenetic study published 20 years ago reported that karyotypic alterations of cribriform prostate adenocarcinoma were more closely related to Gleason pattern 5 than to other morphologic patterns of Gleason pattern 4 (Qian et al. 1997). Recently, cribriform invasive prostate carcinoma has been linked to increased genomic instability (Bottcher et al. 2018).
Poorly formed glands
The 2005 ISUP consensus included poorly formed glands in Gleason pattern 4 (Epstein et al. 2005). As a consequence, this morphology is now commonest of Gleason pattern 4 (Gottipati et al. 2012) and, as already mentioned, some 3 + 4 tumors with this finding may not differ in clinical behavior from indolent 3 + 3 tumors (Kweldam et al. 2016b). Besides the discussion on its clinical relevance, the morphology of poorly formed glands is the most problematic in Gleason grading in terms of reproducibility, even among experienced urologic pathologists. The original 2005 consensus publication indeed acknowledged that in some cases both the diagnosis of 3 + 3 or 3 + 4 are acceptable in cases in which tangentially cut well differentiated glands could not be ruled out. Cases with borderline morphology of minor component of poorly formed glands (3 + 3 vs 3 + 4) has become a major problem in consultation series with impact on decision for eligibility for active surveillance (McKenney et al. 2011; Sadimin et al. 2016; Uson et al. 2017).
The potential overdiagnosis has serious practical implication. In four post-2005 large series, the downgrade rate from 3 + 4 to 3 + 3 tumors between needle biopsies and prostatectomies ranged from 0 to 24%. The highest rate was seen in the largest series from the US enrolling 5071 patients (Epstein et al. 2012). In the largest series, a nationwide survey from Sweden (15,598 subjects), the rate of downgrade was 17% (Danneman et al. 2017). This means that some poorly formed glands in small samples may be overvalued while similar foci may be overlooked in the background of extensive Gleason pattern 3 seen in radical prostatectomy specimens. The logical consequence is that Gleason pattern 4 overdiagnosis leads to a scenario where many patients are guided to unnecessary definitive treatments.
Zhou and colleagues worked in a reproducibility study enrolling 17 urologic patologists who gave their opinion whether 23 photomicrographs were diagnostic of Gleason pattern 4 (Zhou et al. 2015). The results allowed the general recommendations to refine the criteria of diagnosing poorly formed glands: only glands without lumens or rarely with lumens should be considered poorly formed glands; the Gleason pattern 4 should be avoided if they are adjacent to well differentiated glands (regardless of the number of poorly formed glands) and if ≤5 poorly formed glands are seem; and, in borderline cases, the pathologist should be conservative and report the lower grade (Zhou et al. 2015).
The 2014 ISUP consensus clarified that occasional poorly formed or fused glands in the background of well-formed glands are insufficient for a diagnosis of Gleason pattern 4, and that in borderline cases the lower grade should be favored (Epstein et al. 2016a).
Intraductal carcinoma
Intraductal carcinoma of the prostate was recognized as new entity in the 2016 WHO blue book (Moch et al. 2016a). Unlike intraductal carcinoma in other sites, it is conceived as the intraductal spread of invasive aggressive carcinomas and not a pre-invasive lesion (at least in most cases). The intraductal component should not be graded. When seen unassociated with high-grade invasive cancer in needle biopsy, the 2014 ISUP consensus recommends that a comment should be added in the pathology report on the invariably association with aggressive invasive carcinoma (Epstein et al. 2016a).
Defined criteria for intraductal carcinoma are the presence of malignant epithelial cells filling large acini and prostatic ducts (Fig. 2a) with preservation of basal cell layer (Fig. 2b) and: solid or dense cribriform pattern (> 50% of lumen filled by epithelial cells); or loose cribriform or micropapillary patterns if associated with marked nuclear atypia (nuclear size 6× normal) or comedonecrosis (Guo and Epstein 2006). Loose cribriform and micropapillary patterns are also seen in high grade prostatic intraepithelial neoplasia (HGPIN) and must be distinguished because the clinical implications of a HGPIN diagnosis is much less ominous. In current practice, a single focus of HGPIN at needle biopsy may be managed just as a needle biopsy with only benign findings. When multifocal HGPIN (defined as > 1 core) at needle biopsy is seen, there is an increased risk of detecting adenocarcinoma in a subsequent biopsy and, as a consequence, new biopsy should be considered immediately or in a shorter schedule (Fine et al. 2012; Merrimen et al. 2009; Netto and Epstein 2006). In a series including 21 pure intraductal carcinomas (with no concomitant invasive carcinoma) seen at biopsy and with available data from radical prostatectomy, only 2 (10%) had no invasive prostatic carcinoma and most cases had high Gleason scores ≥8 tumors (Robinson and Epstein 2010). Thus, it is mandatory to report the presence of intraductal carcinoma in pathology reports, especially in needle biopsies since its presence may indicate repeated biopsy (Robinson et al. 2012).
Intraductal carcinoma of the prostate in a prostatectomy specimen associated with invasive adenocarcinoma. a HE stain (40×) shows expanded ducts with loose and dense cribriform morphologies surrounded by small infiltrative glands of acinar adenocarcinoma. b Immunohistochemistry of a cocktail using basal cell markers (p63 and high molecular weight cytokeratin, 34BE12) and Alpha-methylacyl-CoA racemase (AMACR) (40×): intraductal carcinoma show preserved basal cell layer while luminal cells of intraductal carcinoma and invasive adenocarcinoma express AMACR. c PTEN immunohistochemistry (100×) shows loss of nuclear and cytoplasmatic express of PTEN protein in intraductal carcinoma while preserved stain is seen in adjacent stroma
Subsequent studies showed that the presence of intraductal carcinoma associated with invasive adenocarcinoma in needle biopsies is associated with decreased cancer-free survival, even in the subgroup of patients with higher Gleason scores ≥8 (Zhao et al. 2015). In intermediate risk patients treated by radical prostatectomy or radiotherapy, intraductal carcinomas at biopsies was predictive of early biochemical recurrence and metastasis (Van der Kwast et al. 2012). Also for patients with intraductal carcinoma associated with invasive adenocarcinoma Gleason 6 at biopsy, most patients had unfavorable prognosis such as metastasis at diagnosis, progression during active surveillance or high-grade and high-stage tumor at prostatectomy. Among 14 available radical prostatectomy specimens, pT2 stage and Gleason score 6 were seen in only 36% and 21%, respectively (Khani and Epstein 2015). Intraductal carcinoma at radical prostatectomy specimens has been also reported to be an independent predictor of biochemical recurrence (Kimura et al. 2014; Miyai et al. 2014) and cancer-specific survival (Kimura et al. 2014). A recent study showed that intraductal carcinoma diagnosed in prostate needle biopsies of patients with metastatic prostate cancer was predictive of early emergence of castration-resistant prostate cancer (Zhao et al. 2017). Taken together, these data indicate that the presence of intraductal carcinoma should be reported in any prostatic specimens: needle biopsy, transurethral resection and prostatectomy specimens.
When dense cribriform or solid variants of prostate intraductal carcinoma are seen, the major differential diagnosis are invasive high-grade acinar adenocarcinoma and urothelial carcinoma – both invasive or spreading into prostatic ducts. In these scenario, immunohistochemistry is helpful to investigate integrity of basal cell layer and distinction between prostatic and urothelial epithelium (Robinson et al. 2012). For loose cribriform or micropapillary variants, the most important differential diagnosis is HGPIN. In borderline cases, loss of cytoplasmic expression of phosphatase and tensin homolog (PTEN) protein by immunohistochemistry favor the diagnosis of intraductal carcinoma (Lotan et al. 2013; Morais et al. 2015) (Fig. 2c). Given the clinical implications of the diagnosis of intraductal carcinoma, it is reasonable to use descriptive terms such as atypical intraductal proliferation when facing a borderline lesions sharing features of HGPIN and intraductal carcinoma. A comment on the difficulty to distinguish HGPIN and intraductal carcinoma and the clinical implications of both diagnoses should be added in the report (Robinson et al. 2012).
Grade concordance between needle biopsy and prostatectomy
Concordance between grades assigned in needle biopsy and radical prostatectomy is not perfect. An obvious reason for discrepancies is sampling. Other sources of variation include: 1) how biopsy grade is picked as the biopsy set grade: it is common practice in Europe and Canada to give a global grade weighing data from different cores while clinicians will typically pick the highest grade from all regions (Athanazio et al. 2017); 2) there is inherit differences between how Gleason score is calculated since the 2005 ISUP consensus: the dominant grade plus the higher among non-dominant patterns in needle biopsy and the dominant grade plus the second most common in prostatectomies (Epstein et al. 2005); Gleason score is given in separate assignments per region in needle biopsy because, in theory, each area could represent different nodules, however, the most common scenario in radical prostatectomy is that there is a multifocal tumor and a single grade will be giving weighing findings from the whole tumor.
Table 2 details findings of the four largest series comparing grades between needle biopsy and radical prostatectomy specimens post-2005 consensus (Epstein et al. 2012; Danneman et al. 2017; Athanazio et al. 2017; Samaratunga et al. 2015). The issue of the relative high rate of downgrade from GG2 to GG1 in some series have been already discussed in the section on “poorly formed glands”. The second issue that emerges from Table 2 is the high rate of upgrade from GG1 to GG2 (ranging from 20 to 48%), a common scenario in clinical practice. In this case, sampling is the most reasonable explanation on why high-grade tumor was missed in biopsies. Using only clinicopathological data, upgrade of biopsy GG1 was associated with age ≥ 60 years, PSA density ≥ 0.2, ≥ positive cores, ≥% core tissue and perineural involvement. Downgrade of biopsy GG2 correlated inversely with age ≥ 60 years, PSA > 10 ng/ml and ≥ 2 positive core (Athanazio et al. 2017). In a recent large series, the overall rate of upgrade was 51% and upgrade from GG1 at biopsy was predicted by age, abnormal digital rectal examination serum PSA density, percentage of positive cores and body mass index (Audenet et al. 2017).
In our practice, most cases upgraded from GG1 to GG2 still shows prostatectomy findings which are predictive of indolent behavior: These tumors showed a low frequency of non-focal extraprostatic extension (3%), extensive positive surgical margins (6%) and seminal vesicle invasion (3%) (Souza et al. 2018). In contrast, Cocoran and collegues showed that pathological findings at prostatectomy and biochemical recurrence curves were similar for those patients with upgrade GG1 to GG2 when compared to concordant tumors with GG2 (3 + 4) at biopsy and radical prostatectomy (Corcoran et al. 2011).
There is an urgent need for biomarkers that could predict upgrade or aggressive behaviors in patients with limited Gleason 3 + 3 cancers diagnosed in biopsy specimens. In this field, the most promising marker is again PTEN. Loss of PTEN evaluated by immunohistochemistry was an independent risk factor for upgrading from Gleason score 6 at biopsy to score 7 or higher: with odds ratio of 2.8 and 3.0 in two models (Lotan et al. 2015). In other study, PTEN loss was an independent predictor of upgrade of 3 + 3 tumors in core biopsies with odds ratio of 5.2 (Trock et al. 2016). Loss of PTEN expression by immunohistochemistry is concordant with deletion by fluorescent in situ hybridization (Picanco-Albuquerque et al. 2016). These findings suggest that Gleason pattern 3 adjacent to higher grade components shows already a molecular profile that can be distinguished from morphologic similar Gleason pattern 3 of pure indolent tumors. In other words, PTEN loss in Gleason pattern 3 can predict the presence of un-sampled grade 4 tumor: and the use of this biomarker may prevent enrolling high-risk men for active surveillance. This is a simple test that can be readily adopted in clinical practice giving valuable information that is much less expensive than currently adopted genetic panels. Validation from other centers may give additional argument to implement PTEN immunohistochemistry in the routine practice of active surveillance.
Bladder pathology
Divergent differentiation and aggressive variants of urothelial carcinoma
The 2016 WHO blue book changed the classification of invasive urothelial carcinoma to distinguish tumors with and without divergent differentiation. Urothelial carcinoma is well known to show a wide morphologic plasticity. Some variants are rare and the limited number of cases restricts the evaluation of the clinical impact of all variants. Squamous and glandular differentiation are the commonest variants. The 2016 WHO blue books recognized the patters of micropapillary, plasmacytoid and poorly differentiated as more aggressive variants – and the percentage of each variants should be reported (Moch et al. 2016b; College of American Pathologists 2018b) . Recognizing morphological variants with different clinical behavior is of relevance since, by default, almost all invasive urothelial carcinomas area labelled as high grade (Amin et al. 2015).
Micropapillary and plasmacytoid variants are important because of the clinical implications in prognosis, even in superficially invasive (pT1) tumors. In addition, there are reports suggesting that these variants are commonly missed in daily practice – suggesting an impact on care associated with the implementation of central pathology review (Shah et al. 2013). Overall, 20% of invasive urothelial carcinomas show divergent differentiation and 44% of these variants were not primarily recognized (Shah et al. 2013).
Micropapillary variant may be difficult to recognize because it shares with ordinary invasive carcinomas the appearance of lacunar spaces with epithelial growth within it, which is attributed to retraction artifact in the latter. True micropapillae are delicate filiform process without true fibrovascular core tightly clustered within lacunar spaces. Features suggested to be distinctive of micropapillary variants are multiple epithelial nests within a single lacuna (Fig. 3a and b)or epithelial ring formation (Fig. 3c) (Amin et al. 2015).
Micropapillary morphology is associated with poor prognosis and the percentage of micropapillary morphology in transurethral resections was reported to predict higher stage (Gaya et al. 2010; Samaratunga and Khoo 2004) and cancer specific death (Samaratunga and Khoo 2004; Comperat et al. 2010). Those findings are the main reason to report the presence and the percentage of micropapillary morphology in pathology reports. The association with poorer outcome led some authors to suggest early cystectomy even in pT1 tumors (Kamat et al. 2006). Since some cases treated with early cystectomy still show advanced stage and nodal metastasis, consideration of neoadjuvant chemotherapy has been suggested (Ghoneim et al. 2011), while a recent study suggested benefit of prior chemotherapy only in muscle invasive disease (Fernandez et al. 2017). Other groups, however, do not agree with early cystectomy in tumor without muscle invasive disease especially in cases with low percentage of micropapillary morphology and lack of associated carcinoma in situ (Gaya et al. 2010; Spaliviero et al. 2014).
Plasmacytoid variant is now the term of choice for what has been called in the past signet ring or diffuse variants of urothelial carcinoma (Moch et al. 2016b) (Fig. 3d). It is usually associated with advanced stage at diagnosis and poor survival (Fox et al. 2017). In a trial of muscleinvasive urothelial carcinoma, treated by radical cystectomy and adjuvant cisplatin-based chemotherapy, it was shown that plasmacytoid morphology was an independent predictor of poor survival when compared to ordinary urothelial carcinoma and even to micropapillary variant (Keck et al. 2013). Other recent series did not show the impact of plasmacytoid morphology on outcome (Li et al. 2017). A characteristic clinical feature is the high rate of recurrence with peritoneal spread (Dayyani et al. 2013; Ricardo-Gonzalez et al. 2012). A potential pitfall in cystoscopy is that the tumor may invade muscularis propria without grossly identifiable mucosal tumor (Fritsche et al. 2008). Mirroring the discussion on early cystectomy for the micropapillary variant, some authors also suggest aggressive therapy in pT1 disease with plasmacytoid morphology (Kaimakliotis et al. 2014).
Both micropapillary and plasmacytoid variants commonly show HER2 oncogene alterations including amplification and mutation and, therefore, may be prone to target therapy in the future (Ching et al. 2011; Ross et al. 2014; Schneider et al. 2014; Kim et al. 2016).
The direct role of divergent differentiation (variant morphologies) on treatment decision is a matter of debate. One group recommended a treatment algorithm with earlycystectomy in non-muscle invasive bladder cancer (T1) with micropapillary, plasmacytoid and sarcomatoid morphologies (Willis and Kamat 2015). Although an early surgical treatment is not explicitly recommended in the MD Anderson practice algorithm, patients with micropapillary and sarcomatoid variants may be followed even as T2 tumors; however, early cystectomy should be considered in variant morphologies demonstrating concurrent carcinoma in situ (MD Anderson Cancer Center n.d.). The current National Comprehensive Cancer Network (NCCN) guideline for bladder cancer states that non-muscle invasive bladder cancer with micropapillary, plasmacytoid and sarcomatoid morphologies are at higher risk of progression and more aggressive approach should be considered (National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology n.d.). The American Urological Association (AUA)/ Society of Urologic Oncology (SUO) Guideline mentions that an experienced genitourinary pathologist should review the pathology of a patient with any doubt in regards to variant or suspected variant histology (e.g., micropapillary, nested, plasmacytoid, neuroendocrine, sarcomatoid), extensive squamous or glandular differentiation, or the presence/absence of LVI. (Moderate Recommendation; Evidence Strength: Grade C). Presence of variant histology requires restaging transurethral resection within 4–6 weeks when a bladder sparing approach is considered, or consideration of early cystectomy due to high risk of upstaging (Expert Opinion) (Chang et al. 2016). The European Association of Urology (EAU) guidelines on Non-muscle-invasive Bladder Cancer mentions micropapillary, nested, plasmacytoid, sarcomatoid, microcystic, squamous and adeno variants as associated with poor prognosis (Babjuk et al. 2017).
pT1 substaging
The 2017 8th edition of American Joint Committee on Cancer Staging System (AJCC) did not change the staging system of bladder cancer (Bochner et al. 2017). Both AJCC and the College of American Pathologists (CAP), however, strongly recommends substaging of pT1 disease (College of American Pathologists 2018b; Bochner et al. 2017). The lamina propria is a thick layer of loose connective tissue and pT1 disease may range from a single microscopic invasive focus to large grossly identifiable invasive tumors. Upstaging of pT1 tumors in radical cystectomy to pT2 or higher is common: 48–50% with 33% to nonorgan confined disease (pT3 or positive lymph nodes) (Paner et al. 2017). Such heterogeneity urges the development of strategies that improve risk stratification of pT1 tumors in transurethral resection specimens.
In the past, some author suggested substratification of pT1 disease based on relationship of muscularis mucosa: lamina propria and submucosa. Such approach is complicated because the presence of muscularis mucosa is variable in different topographies of the bladder – it is present in continuous or discontinuous layer in 40% of the cystectomy sections. The most popular approach in current practice is micrometric size estimation of invasive foci with proposed cutoffs of 0.5 mm and 1.0 mm (Paner et al. 2017).
The CAP protocol acknowledges that substaging methods have been difficult to adopt due to the inherent lack of orientation of the specimen. Pathologists are, however, encouraged to provide some assessment as to the extent of lamina propria invasion (ie, maximum dimension of invasive focus, or depth in millimeters, or by level – above, at, or below muscularis mucosae (College of American Pathologists 2018b). For papillary pT1 disease, there is also evidence that site distinction (invasion of stalk or base of the lesion) has prognostic impact. In the proposed classification of Lawless and colleagues, the base-extensive category (defined as a few microinvasive foci > 1 mm apart, in multiple tissue fragments, or invasion of an area that would not fit within one 20× high power field) showed higher rate of progression (Lawless et al. 2017).
In our practice, we provide in pathology reports of pT1 disease in transurethral resections the maximum dimension of invasive focus and the distinction of invasive foci in stalk only versus base of the lesion.
Staging issues in transurethral resections
The 8th AJCC Staging Manual clearly states that pathological staging of bladder cancer should be performed in cystectomy specimens (Bochner et al. 2017). Although pT classification is not recommended for transurethral resection specimens, there is a widely accepted practice of giving a pT stage in the pathology reports of these materials. Such practice is probably influenced by the fact that many patients are treated with conservative therapy and the pathological examination of transurethral resection specimens will be the only source of anatomic staging. The 8th AJCC Staging Manual did not change the anatomical staging of bladder cancer, however, some important clarifications were provided.
It is well known that muscularis mucosa may be hyperplastic and may mimick muscularis propria (detrusor muscle) in transurethral resection specimens. Muscularis propria is recognized by tight aggregates of large bundles of smooth muscle (Paner et al. 2017). The ISUP does not recommend use of smoothelin to discriminate muscularis mucosae from muscularis propria. Desmin may be used to highlight bundles of smooth muscle in areas of destructive desmoplastic invasive foci, but cannot discriminate those two muscular layers (Amin et al. 2014b). Because of the relevance of this distinction, which is a major guide to decision making, all pathology reports of transurethral resection specimens should clearly state whether muscularis propria is present or absent, and whether muscularis propria is involved. Confounding terms such as “invasion of muscle bundles” should be avoided.
Adipose tissue is seen within lamina propria in 53% and in 100% of muscularis propria (Philip et al. 2000). Consequently, invasion of adipose tissue seen in transurethral resection specimens cannot be diagnostic of pT3 disease. The discrepancy between the imaging studies showing perivesical tissue invasion, and pathologic evaluation of transurethral resection specimen indicating pT2 (muscle invasive) urothelial carcinoma can be a source of confusion at tumor board discussions. It must be noted that in transurethral resection specimens, it is not possible to assign a higher stage than pT2. To avoid confusion, pathology reports should simply assign if muscularis propria is present and involved, or not; or a pathologic stage can be given with a comment that the stage is pT2 or higher (and definitive pathologic stage will depend on radical cystectomy specimen).
The diagnosis of pT4a disease should also be avoided in transurethral resection specimens. In a survey of the European Network of Uropathology in 2008, 74% of the pathologist answered they would assign pT4a disease if prostatic stromal invasion is seen in transurethral resection specimens (Lopez-Beltran et al. 2011). The 8th AJCC Staging Manual clarifies that stromal prostatic invasion could be explained by three routes: direct invasion of a bladder tumor into the prostate (a true pT4a), invasion of a bladder tumor using the path of invasion through perivesical adipose tissue (pT3) or by intraurethral route. A bladder tumor may extend into prostatic urethra and invade prostatic stroma. Alternatively, the patient may harbor two independent tumors in the bladder and in the prostatic urethra. In such cases, the recommendation is to provide two pT stages: one for the bladder and one for the prostatic urethra, in which invasion of prostatic stroma is pT2 (Bochner et al. 2017; Paner et al. 2017). This distinction can only be made in cystectomy specimens. A reasonable approach is to report invasion of prostatic stroma in transurethral resection specimens with a comment that the definitive pathologic stage will depend on radical cystectomy specimen.
Conclusion
Incorporation in pathology reports of the morphological data currently used in risk stratification can improve the care of patients with prostate and bladder cancer. Such information should be provided in a standardized and clear manner to avoid misinterpretation of the reported findings by urologists, clinical oncologists and radiation oncologists.
References
Amin MB, Lin DW, Gore JL, Srigley JR, Samaratunga H, Egevad L, Rubin M, Nacey J, Carter HB, Klotz L et al (2014a) The critical role of the pathologist in determining eligibility for active surveillance as a management option in patients with prostate cancer: consensus statement with recommendations supported by the College of American Pathologists, International Society of Urological Pathology, Association of Directors of anatomic and surgical pathology, the new Zealand Society of Pathologists, and the Prostate Cancer Foundation. Arch Pathol Lab Med 138(10):1387–1405
Amin MB, Smith SC, Reuter VE, Epstein JI, Grignon DJ, Hansel DE, Lin O, McKenney JK, Montironi R, Paner GP et al (2015) Update for the practicing pathologist: the international consultation on urologic disease-European association of urology consultation on bladder cancer. Mod Pathol 28(5):612–630
Amin MB, Trpkov K, Lopez-Beltran A, Grignon D (2014b) Members of the IIiDUPG: best practices recommendations in the application of immunohistochemistry in the bladder lesions: report from the International Society of Urologic Pathology consensus conference. Am J Surg Pathol 38(8):e20–e34
Athanazio D, Gotto G, Shea-Budgell M, Yilmaz A, Trpkov K (2017) Global Gleason grade groups in prostate cancer: concordance of biopsy and radical prostatectomy grades and predictors of upgrade and downgrade. Histopathology 70(7):1098–1106
Athanazio PR, dos Santos AC, de Freitas LA, Athanazio DA (2014) A modified point count method as a practical approach to assess the tumor volume and the percent gland involvement by prostate carcinoma. Pathol Res Pract 210(5):312–317
Audenet F, Rozet F, Resche-Rigon M, Bernard R, Ingels A, Prapotnich D, Sanchez-Salas R, Galiano M, Barret E, Cathelineau X (2017) Grade group underestimation in prostate biopsy: predictive factors and outcomes in candidates for active surveillance. Clin Genitourin Cancer 15(6):e907–e913
Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, Hernandez V, Kaasinen E, Palou J, Roupret M et al (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71(3):447–461
Bochner BH, Hansel DE, Efstathiou JA, Konety B, Lee CT, McKiernan JM, Plimack ER, Reuter VE, Sridhar S, Vikram R et al (2017) Urinary bladder. In: Amin MB, Edge SB, Green SL, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC et al (eds) AJCC Cancer staging manual. 8th edn. Springer, Chicago, pp 757–765
Bottcher R, Kweldam CF, Livingstone J, Lalonde E, Yamaguchi TN, Huang V, Yousif F, Fraser M, Bristow RG, van der Kwast T et al (2018) Cribriform and intraductal prostate cancer are associated with increased genomic instability and distinct genomic alterations. BMC Cancer 18(1):8
Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, Pruthi R, Quale DZ, Ritch CR, Seigne JD et al (2016) Diagnosis and treatment of non-muscle invasive bladder Cancer: AUA/SUO guideline. J Urol 196(4):1021–1029
Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR, Morgan SC, Tyldesley S, Haluschak JJ, Tan W et al (2016) Active surveillance for the Management of Localized Prostate Cancer (Cancer Care Ontario guideline): American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 34(18):2182–2190
Ching CB, Amin MB, Tubbs RR, Elson P, Platt E, Dreicer R, Fergany A, Hansel DE (2011) HER2 gene amplification occurs frequently in the micropapillary variant of urothelial carcinoma: analysis by dual-color in situ hybridization. Mod Pathol 24(8):1111–1119
Choy B, Pearce SM, Anderson BB, Shalhav AL, Zagaja G, Eggener SE, Paner GP (2016) Prognostic significance of percentage and architectural types of contemporary Gleason pattern 4 prostate Cancer in radical prostatectomy. Am J Surg Pathol 40(10):1400–1406
Chun FK, Briganti A, Jeldres C, Gallina A, Erbersdobler A, Schlomm T, Walz J, Eichelberg C, Salomon G, Haese A et al (2007) Tumour volume and high grade tumour volume are the best predictors of pathologic stage and biochemical recurrence after radical prostatectomy. Eur J Cancer 43(3):536–543
Cole AI, Morgan TM, Spratt DE, Palapattu GS, He C, Tomlins SA, Weizer AZ, Feng FY, Wu A, Siddiqui J et al (2016) Prognostic value of percent Gleason grade 4 at prostate biopsy in predicting prostatectomy pathology and recurrence. J Urol 196(2):405–411
College of American Pathologists. Protocol for the examination of specimens from patients with carcinoma of the prostate gland, 2018a
College of American Pathologists. Protocol for the examination of specimens from patients with carcinoma of the urinary bladder, 2018b
Comperat E, Roupret M, Yaxley J, Reynolds J, Varinot J, Ouzaid I, Cussenot O, Samaratunga H (2010) Micropapillary urothelial carcinoma of the urinary bladder: a clinicopathological analysis of 72 cases. Pathology 42(7):650–654
Corcoran NM, Hong MK, Casey RG, Hurtado-Coll A, Peters J, Harewood L, Goldenberg SL, Hovens CM, Costello AJ, Gleave ME (2011) Upgrade in Gleason score between prostate biopsies and pathology following radical prostatectomy significantly impacts upon the risk of biochemical recurrence. BJU Int 108(8 Pt 2):E202–E210
Danneman D, Drevin L, Delahunt B, Samaratunga H, Robinson D, Bratt O, Loeb S, Stattin P, Egevad L (2017) Accuracy of prostate biopsies for predicting Gleason score in radical prostatectomy specimens: nationwide trends 2000-2012. BJU Int 119(1):50–56
Danneman D, Drevin L, Robinson D, Stattin P, Egevad L (2015) Gleason inflation 1998-2011: a registry study of 97,168 men. BJU Int 115(2):248–255
Dayyani F, Czerniak BA, Sircar K, Munsell MF, Millikan RE, Dinney CP, Siefker-Radtke AO (2013) Plasmacytoid urothelial carcinoma, a chemosensitive cancer with poor prognosis, and peritoneal carcinomatosis. J Urol 189(5):1656–1661
Deng FM, Donin NM, Pe Benito R, Melamed J, Le Nobin J, Zhou M, Ma S, Wang J, Lepor H (2016) Size-adjusted quantitative Gleason score as a predictor of biochemical recurrence after radical prostatectomy. Eur Urol 70(2):248–253
Dong F, Yang P, Wang C, Wu S, Xiao Y, McDougal WS, Young RH, Wu CL (2013) Architectural heterogeneity and cribriform pattern predict adverse clinical outcome for Gleason grade 4 prostatic adenocarcinoma. Am J Surg Pathol 37(12):1855–1861
Eble JN, Sauter G, Epstein JI, Sesterhenn IA (2004) WHO Classification of Tumours. In: Pathology and genetics of tumours of the urinary system and male genital organs, 3rd edn. IARC, Lyon
Egevad L, Delahunt B, Evans AJ, Grignon DJ, Kench JG, Kristiansen G, Leite KR, Samaratunga H, Srigley JR (2016) International Society of Urological Pathology (ISUP) grading of prostate Cancer. Am J Surg Pathol 40(6):858–861
Epstein JI (2016) International Society of Urological Pathology (ISUP) grading of prostate Cancer. Author's Reply Am J Surg Pathol 40(6):862–864
Epstein JI (2018) Prostate cancer grading: a decade after the 2005 modified system. Mod Pathol 31(S1):S47–S63
Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL, Committee IG (2005) The 2005 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol 29(9):1228–1242
Epstein JI, Amin MB, Reuter VE, Humphrey PA (2017) Contemporary Gleason grading of prostatic carcinoma: an update with discussion on practical issues to implement the 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol 41(4):e1–e7
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, Grading C (2016a) The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40(2):244–252
Epstein JI, Feng Z, Trock BJ, Pierorazio PM (2012) Upgrading and downgrading of prostate cancer from biopsy to radical prostatectomy: incidence and predictive factors using the modified Gleason grading system and factoring in tertiary grades. Eur Urol 61(5):1019–1024
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, Vickers AJ, Parwani AV, Reuter VE, Fine SW et al (2016b) A contemporary prostate Cancer grading system: a validated alternative to the Gleason score. Eur Urol 69(3):428–435
Fernandez MI, Williams SB, Willis DL, Slack RS, Dickstein RJ, Parikh S, Chiong E, Siefker-Radtke AO, Guo CC, Czerniak BA et al (2017) Clinical risk stratification in patients with surgically resectable micropapillary bladder cancer. BJU Int 119(5):684–691
Fine SW, Amin MB, Berney DM, Bjartell A, Egevad L, Epstein JI, Humphrey PA, Magi-Galluzzi C, Montironi R, Stief C (2012) A contemporary update on pathology reporting for prostate cancer: biopsy and radical prostatectomy specimens. Eur Urol 62(1):20–39
Flood TA, Schieda N, Keefe DT, Breau RH, Morash C, Hogan K, Belanger EC, Mai KT, Robertson SJ (2016) Utility of Gleason pattern 4 morphologies detected on transrectal ultrasound (TRUS)-guided biopsies for prediction of upgrading or upstaging in Gleason score 3 + 4 = 7 prostate cancer. Virchows Arch 469(3):313–319
Fox MD, Xiao L, Zhang M, Kamat AM, Siefker-Radtke A, Zhang L, Dinney CP, Czerniak B, Guo CC (2017) Plasmacytoid urothelial carcinoma of the urinary bladder: a Clinicopathologic and Immunohistochemical analysis of 49 cases. Am J Clin Pathol 147(5):500–506
Fritsche HM, Burger M, Denzinger S, Legal W, Goebell PJ, Hartmann A (2008) Plasmacytoid urothelial carcinoma of the bladder: histological and clinical features of 5 cases. J Urol 180(5):1923–1927
Gaya JM, Palou J, Algaba F, Arce J, Rodriguez-Faba O, Villavicencio H (2010) The case for conservative management in the treatment of patients with non-muscle-invasive micropapillary bladder carcinoma without carcinoma in situ. Can J Urol 17(5):5370–5376
Ghoneim IA, Miocinovic R, Stephenson AJ, Garcia JA, Gong MC, Campbell SC, Hansel DE, Fergany AF (2011) Neoadjuvant systemic therapy or early cystectomy? Single-center analysis of outcomes after therapy for patients with clinically localized micropapillary urothelial carcinoma of the bladder. Urology 77(4):867–870
Gleason DF (1966) Classification of prostatic carcinomas. Cancer Chemother Rep 50(3):125–128
Gottipati S, Warncke J, Vollmer R, Humphrey PA (2012) Usual and unusual histologic patterns of high Gleason score 8 to 10 adenocarcinoma of the prostate in needle biopsy tissue. Am J Surg Pathol 36(6):900–907
Guo CC, Epstein JI (2006) Intraductal carcinoma of the prostate on needle biopsy: histologic features and clinical significance. Mod Pathol 19(12):1528–1535
Iczkowski KA, Torkko KC, Kotnis GR, Wilson RS, Huang W, Wheeler TM, Abeyta AM, La Rosa FG, Cook S, Werahera PN et al (2011) Digital quantification of five high-grade prostate cancer patterns, including the cribriform pattern, and their association with adverse outcome. Am J Clin Pathol 136(1):98–107
Kaimakliotis HZ, Monn MF, Cary KC, Pedrosa JA, Rice K, Masterson TA, Gardner TA, Hahn NM, Foster RS, Bihrle R et al (2014) Plasmacytoid variant urothelial bladder cancer: is it time to update the treatment paradigm? Urol Oncol 32(6):833–838
Kamat AM, Gee JR, Dinney CP, Grossman HB, Swanson DA, Millikan RE, Detry MA, Robinson TL, Pisters LL (2006) The case for early cystectomy in the treatment of nonmuscle invasive micropapillary bladder carcinoma. J Urol 175(3 Pt 1):881–885
Keck B, Wach S, Stoehr R, Kunath F, Bertz S, Lehmann J, Stockle M, Taubert H, Wullich B, Hartmann A (2013) Plasmacytoid variant of bladder cancer defines patients with poor prognosis if treated with cystectomy and adjuvant cisplatin-based chemotherapy. BMC Cancer 13:71
Khani F, Epstein JI (2015) Prostate biopsy specimens with Gleason 3+3=6 and Intraductal carcinoma: radical prostatectomy findings and clinical outcomes. Am J Surg Pathol 39(10):1383–1389
Kim B, Kim G, Song B, Lee C, Park JH, Moon KC (2016) HER2 protein overexpression and gene amplification in Plasmacytoid urothelial carcinoma of the urinary bladder. Dis Markers 2016:8463731
Kimura K, Tsuzuki T, Kato M, Saito AM, Sassa N, Ishida R, Hirabayashi H, Yoshino Y, Hattori R, Gotoh M (2014) Prognostic value of intraductal carcinoma of the prostate in radical prostatectomy specimens. Prostate 74(6):680–687
Kir G, Sarbay BC, Gumus E, Topal CS (2014) The association of the cribriform pattern with outcome for prostatic adenocarcinomas. Pathol Res Pract 210(10):640–644
Kweldam CF, Kummerlin IP, Nieboer D, Steyerberg EW, Bangma CH, Incrocci L, van der Kwast TH, Roobol MJ, van Leenders GJ (2017) Presence of invasive cribriform or intraductal growth at biopsy outperforms percentage grade 4 in predicting outcome of Gleason score 3+4=7 prostate cancer. Mod Pathol 30(8):1126–1132
Kweldam CF, Kummerlin IP, Nieboer D, Verhoef EI, Steyerberg EW, Incrocci L, Bangma CH, van der Kwast TH, Roobol MJ, van Leenders GJ (2016b) Prostate cancer outcomes of men with biopsy Gleason score 6 and 7 without cribriform or intraductal carcinoma. Eur J Cancer 66:26–33
Kweldam CF, Kummerlin IP, Nieboer D, Verhoef EI, Steyerberg EW, van der Kwast TH, Roobol MJ, van Leenders GJ (2016a) Disease-specific survival of patients with invasive cribriform and intraductal prostate cancer at diagnostic biopsy. Mod Pathol 29(6):630–636
Kweldam CF, Wildhagen MF, Steyerberg EW, Bangma CH, van der Kwast TH, van Leenders GJ (2015) Cribriform growth is highly predictive for postoperative metastasis and disease-specific death in Gleason score 7 prostate cancer. Mod Pathol 28(3):457–464
Kwon O, Kim TJ, Lee IJ, Byun SS, Lee SE, Hong SK (2014) Can contemporary patients with biopsy Gleason score 3+4 be eligible for active surveillance? PLoS One 9(9):e109031
Lawless M, Gulati R, Tretiakova M (2017) Stalk versus base invasion in pT1 papillary cancers of the bladder: improved substaging system predicting the risk of progression. Histopathology 71(3):406–414
Li Q, Assel M, Benfante NE, Pietzak EJ, Herr HW, Donat M, Cha EK, Donahue TF, Bochner BH, Dalbagni G (2017) The impact of Plasmacytoid variant histology on the survival of patients with urothelial carcinoma of bladder after radical cystectomy. Eur Urol Focus. https://doi.org/10.1016/j.euf.2017.06.013. In press.
Lopez-Beltran A, Algaba F, Berney DM, Boccon-Gibod L, Camparo P, Griffiths D, Mikuz G, Montironi R, Varma M, Egevad L (2011) Handling and reporting of transurethral resection specimens of the bladder in Europe: a web-based survey by the European network of Uropathology (ENUP). Histopathology 58(4):579–585
Lotan TL, Carvalho FL, Peskoe SB, Hicks JL, Good J, Fedor H, Humphreys E, Han M, Platz EA, Squire JA et al (2015) PTEN loss is associated with upgrading of prostate cancer from biopsy to radical prostatectomy. Mod Pathol 28(1):128–137
Lotan TL, Gumuskaya B, Rahimi H, Hicks JL, Iwata T, Robinson BD, Epstein JI, De Marzo AM (2013) Cytoplasmic PTEN protein loss distinguishes intraductal carcinoma of the prostate from high-grade prostatic intraepithelial neoplasia. Mod Pathol 26(4):587–603
McKenney JK, Simko J, Bonham M, True LD, Troyer D, Hawley S, Newcomb LF, Fazli L, Kunju LP, Nicolas MM et al (2011) The potential impact of reproducibility of Gleason grading in men with early stage prostate cancer managed by active surveillance: a multi-institutional study. J Urol 186(2):465–469
MD Anderson Cancer Center - Urothelial Carcinoma of Bladder and Upper Tract [https://www.mdanderson.org/documents/for-physicians/algorithms/cancer-treatment/ca-treatment-bladder-web-algorithm.pdf]. Accessed 28 Feb 2018.
Merrimen JL, Jones G, Walker D, Leung CS, Kapusta LR, Srigley JR (2009) Multifocal high grade prostatic intraepithelial neoplasia is a significant risk factor for prostatic adenocarcinoma. J Urol 182(2):485–490 discussion 490
Miyai K, Divatia MK, Shen SS, Miles BJ, Ayala AG, Ro JY (2014) Heterogeneous clinicopathological features of intraductal carcinoma of the prostate: a comparison between “precursor-like” and “regular type” lesions. Int J Clin Exp Pathol 7(5):2518–2526
Moch H, Humphrey PA, Ulbright TM, Reuter VE (2016a) Chapter 3 Tumours of the prostate. In: WHO Classification of Tumours of the urinary system and male genital organs. edn. IARC, Lyon, pp 135–183
Moch H, Humphrey PA, Ulbright TM, Reuter VE (2016b) Chapter 2 Tumours of the urinary tract. In: WHO classification of Tumours of the urinary system and male genital organs, 4th edn. IARC, Lyon, pp 77–133
Morais CL, Han JS, Gordetsky J, Nagar MS, Anderson AE, Lee S, Hicks JL, Zhou M, Magi-Galluzzi C, Shah RB et al (2015) Utility of PTEN and ERG immunostaining for distinguishing high-grade PIN from intraductal carcinoma of the prostate on needle biopsy. Am J Surg Pathol 39(2):169–178
Morash C, Tey R, Agbassi C, Klotz L, McGowan T, Srigley J, Evans A (2015) Active surveillance for the management of localized prostate cancer: guideline recommendations. Can Urol Assoc J 9(5–6):171–178
National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology - Bladder Cancer [https://www.nccn.org/professionals/physician_gls/default.aspx]. Accessed 28 Feb 2018.
Netto GJ, Epstein JI (2006) Widespread high-grade prostatic intraepithelial neoplasia on prostatic needle biopsy: a significant likelihood of subsequently diagnosed adenocarcinoma. Am J Surg Pathol 30(9):1184–1188
Paner GP, Montironi R, Amin MB (2017) Challenges in pathologic staging of bladder Cancer: proposals for fresh approaches of assessing pathologic stage in light of recent studies and observations pertaining to bladder Histoanatomic variances. Adv Anat Pathol 24(3):113–127
Philip AT, Amin MB, Tamboli P, Lee TJ, Hill CE, Ro JY (2000) Intravesical adipose tissue: a quantitative study of its presence and location with implications for therapy and prognosis. Am J Surg Pathol 24(9):1286–1290
Picanco-Albuquerque CG, Morais CL, Carvalho FL, Peskoe SB, Hicks JL, Ludkovski O, Vidotto T, Fedor H, Humphreys E, Han M et al (2016) In prostate cancer needle biopsies, detections of PTEN loss by fluorescence in situ hybridization (FISH) and by immunohistochemistry (IHC) are concordant and show consistent association with upgrading. Virchows Arch 468(5):607–617
Pierorazio PM, Walsh PC, Partin AW, Epstein JI (2013) Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int 111(5):753–760
Qian J, Jenkins RB, Bostwick DG (1997) Detection of chromosomal anomalies and c-myc gene amplification in the cribriform pattern of prostatic intraepithelial neoplasia and carcinoma by fluorescence in situ hybridization. Mod Pathol 10(11):1113–1119
Ricardo-Gonzalez RR, Nguyen M, Gokden N, Sangoi AR, Presti JC Jr, McKenney JK (2012) Plasmacytoid carcinoma of the bladder: a urothelial carcinoma variant with a predilection for intraperitoneal spread. J Urol 187(3):852–855
Robinson B, Magi-Galluzzi C, Zhou M (2012) Intraductal carcinoma of the prostate. Arch Pathol Lab Med. 136(4):418–425
Robinson BD, Epstein JI (2010) Intraductal carcinoma of the prostate without invasive carcinoma on needle biopsy: emphasis on radical prostatectomy findings. J Urol 184(4):1328–1333
Ross JS, Wang K, Gay LM, Al-Rohil RN, Nazeer T, Sheehan CE, Jennings TA, Otto GA, Donahue A, He J et al (2014) A high frequency of activating extracellular domain ERBB2 (HER2) mutation in micropapillary urothelial carcinoma. Clin Cancer Res 20(1):68–75
Sadimin ET, Khani F, Diolombi M, Meliti A, Epstein JI (2016) Interobserver reproducibility of percent Gleason pattern 4 in prostatic adenocarcinoma on prostate biopsies. Am J Surg Pathol 40(12):1686–1692
Samaratunga H, Delahunt B, Gianduzzo T, Coughlin G, Duffy D, LeFevre I, Johannsen S, Egevad L, Yaxley J (2015) The prognostic significance of the 2014 International Society of Urological Pathology (ISUP) grading system for prostate cancer. Pathology 47(6):515–519
Samaratunga H, Khoo K (2004) Micropapillary variant of urothelial carcinoma of the urinary bladder; a clinicopathological and immunohistochemical study. Histopathology 45(1):55–64
Schneider SA, Sukov WR, Frank I, Boorjian SA, Costello BA, Tarrell RF, Thapa P, Houston Thompson R, Tollefson MK, Jeffrey Karnes R et al (2014) Outcome of patients with micropapillary urothelial carcinoma following radical cystectomy: ERBB2 (HER2) amplification identifies patients with poor outcome. Mod Pathol 27(5):758–764
Shah RB, Montgomery JS, Montie JE, Kunju LP (2013) Variant (divergent) histologic differentiation in urothelial carcinoma is under-recognized in community practice: impact of mandatory central pathology review at a large referral hospital. Urol Oncol 31(8):1650–1655
Souza MF, Araujo ALCA, Silva MT, Athanazio DA (2018) The Gleason pattern 4 in radical prostatectomy specimens in current practice - quantification, morphology and concordance with biopsy. Ann Diag Pathol 34:13–17
Spaliviero M, Dalbagni G, Bochner BH, Poon BY, Huang H, Al-Ahmadie HA, Donahue TF, Taylor JM, Meeks JJ, Sjoberg DD et al (2014) Clinical outcome of patients with T1 micropapillary urothelial carcinoma of the bladder. J Urol 192(3):702–707
Trock BJ, Fedor H, Gurel B, Jenkins RB, Knudsen BS, Fine SW, Said JW, Carter HB, Lotan TL, De Marzo AM (2016) PTEN loss and chromosome 8 alterations in Gleason grade 3 prostate cancer cores predicts the presence of un-sampled grade 4 tumor: implications for active surveillance. Mod Pathol 29(7):764–771
Trudel D, Downes MR, Sykes J, Kron KJ, Trachtenberg J, van der Kwast TH (2014) Prognostic impact of intraductal carcinoma and large cribriform carcinoma architecture after prostatectomy in a contemporary cohort. Eur J Cancer 50(9):1610–1616
Uson PLSJ, Macarenco R, Oliveira FN, Smaletz O (2017) Impact of pathology review for decision therapy in localized prostate Cancer. Clin Med Insights: Pathology, vol. 10, First Published November 15, 2017. https://doi.org/10.1177/1179555717740130
Van der Kwast T, Al Daoud N, Collette L, Sykes J, Thoms J, Milosevic M, Bristow RG, Van Tienhoven G, Warde P, Mirimanoff RO et al (2012) Biopsy diagnosis of intraductal carcinoma is prognostic in intermediate and high risk prostate cancer patients treated by radiotherapy. Eur J Cancer 48(9):1318–1325
Willis D, Kamat AM (2015) Nonurothelial bladder cancer and rare variant histologies. Hematol Oncol Clin North Am 29(2):237–252 viii
Zhao J, Shen P, Sun G, Chen N, Liu J, Tang X, Huang R, Cai D, Gong J, Zhang X et al (2017) The prognostic implication of intraductal carcinoma of the prostate in metastatic castration-resistant prostate cancer and its potential predictive value in those treated with docetaxel or abiraterone as first-line therapy. Oncotarget 8(33):55374–55383
Zhao T, Liao B, Yao J, Liu J, Huang R, Shen P, Peng Z, Gui H, Chen X, Zhang P et al (2015) Is there any prognostic impact of intraductal carcinoma of prostate in initial diagnosed aggressively metastatic prostate cancer? Prostate 75(3):225–232
Zhou M, Li J, Cheng L, Egevad L, Deng FM, Kunju LP, Magi-Galluzzi C, Melamed J, Mehra R, Mendrinos S et al (2015) Diagnosis of “poorly formed glands” Gleason pattern 4 prostatic adenocarcinoma on needle biopsy: an Interobserver reproducibility study among urologic pathologists with recommendations. Am J Surg Pathol 39(10):1331–1339
Author information
Authors and Affiliations
Contributions
DAA drafted the manuscript and VSC revised it critically for important intellectual content. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Athanazio, D.A., Souza, V.C. Current topics on prostate and bladder pathology. Surg Exp Pathol 1, 2 (2018). https://doi.org/10.1186/s42047-018-0015-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42047-018-0015-6