Abstract
Background
Subdural spinal cord hematomas are very rare condition. They most often occur in patients with primary or secondary blood haemostasis disorders and following lumbar punctures. Early diagnosis and management preserve functional prognosis.
Case description
We report the case of a female 69-year-old patient on oral anticoagulant, Acenocoumarol 4 mg (SINTROM) for previous aortic prosthesis. The patient had undergone surgery for appendicitis under spinal anaesthesia 2 days before her admission in neurosurgery department. She was admitted in emergency for 1/5 central flaccid paraplegia with sensitive umbilical level. A spinal MRI performed showed a collection intradural in intermediate signal in T1 and hyposignal in T2 with echo gradient of 8 mm thickness extended from D8 to L2 compressing the marrow with anomalies of intramedullary signal extended from D8 to the conus medullaris. We retained indication to operate the patient early in emergency because of acute spinal cord compression. We performed T12-L2 laminectomy, durotomy and evacuated hematoma. Postoperative marked by an immediate recovery of sensitivity and an onset of motor recovery from 1/5 to 2/5 and 4/5 follow up at on year with physiotherapy.
Conclusion
Spinal cord compression due to subdural spinal hematomas not often described especially in patients with haemostasis blood disorders due to anticoagulants drugs. In addition, we should pay attention with lumbar puncture in these patients. Emergency surgery allows a good prognosis about recovery of neurological disorders.
Similar content being viewed by others
Introduction
Subdural spinal cord hematomas are very rare condition. They most often occur in patients with primary or secondary blood haemostasis disorders and following lumbar punctures. While spontaneous spinal subdural hematomas most frequently described in association with coagulopathies, iatrogenic causes, or arteriovenous malformations [1, 2], the pathogenesis of spontaneous spinal subdural hematomas largely remains unclear. Rupture of the vasculature within the subarachnoid or subdural space proposed as a potential pathogenic mechanism in certain cases. Options for treatment include surgical decompression, percutaneous drainage, or management with conservative therapies alone [2].
We report this case of a patient on oral anticoagulant, for previous aortic prosthesis who had undergone surgery for appendicitis under spinal anaesthesia 2 days before her admission in neurosurgery department with acute spinal cord compression.
After reporting this case and making a brief review of the literature, we will offer some recommendations in the emergency management of patients on anticoagulants concerning spinal anaesthesia as well as lumbar punctures.
Case description
Clinical description: Patient on oral anticoagulant, Acenocoumarol 4 mg (SINTROM) for previous aortic prosthesis. The patient had undergone surgery for appendicitis under spinal anaesthesia 2 days before her admission in neurosurgery department. On examination, the patient had flaccid paraplegia with grade 1/5 strength in his bilateral upper extremities and grade 1/5 strength throughout his bilateral lower extremities. He noted umbilical sensitive level disorders.
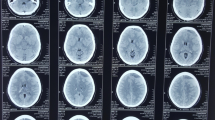
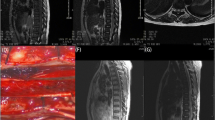
Diagnostic assessment: Magnetic resonance imaging (MRI) T1- and T2-weighted images revealed an intradural, extramedullary heterogeneous subdural T2 and T2* echo gradient hypointense and intermediate signal in T1, signal located ventral to the spinal cord spanning T8 to L2 (conus medullaris) with intramedullary signal. It was looking like subacute or acute spinal subdural hematoma (Figs. 1, 2).
Surgical management: The patient admitted to the operating room urgently for T12-L2 laminectomy, with intradural exploration, and hematoma evacuation. Intraoperatively, a hematoma viewed upon opening and evacuated with gentle suction (Fig. 3). Following evacuation, the spinal cord was visibly free with little stigma of contusions. In addition, inspection of the intradural space did not reveal any apparent abnormalities.
Follow up
Postoperative marked by an immediate recovery of sensitivity and an onset of motor recovery from 1/5 to 2/5 and 4/5 follow up at on year with physiotherapy. He had no bowel or bladder disorders.
Discussion
Epidemiology
Acute spinal subdural hematoma (SSDH) is a rare spinal vascular disorder causing compression of the spinal cord or cauda equina [3]. In a review of 151 patients with non-traumatic spontaneous acute sSDH, 46% of patients either treated with anticoagulation therapy or harboured a coagulopathy attributable to a hematologic disorder [2]. In our case, patient was on oral anticoagulant for previous aortic prosthesis.
In a separate review of 106 cases of non-traumatic acute sSDH, a large proportion of the cases were associated with either bleeding disorders or purely iatrogenic causes, representing 54% and 14% of the cases, respectively [4]. In our present case, had undergone surgery for appendicitis under spinal anaesthesia 2 days before her admission in our neurosurgery department.
Clinical: A typical clinical presentation is sudden onset of spinal or radicular pain, and myelopathy such as paraplegia or sensory level [1]. Our patient had spinal cord compression Grade IV of Mc Cormick classification with flaccid paraplegia with grade 1/5 strength in his bilateral upper extremities and grade 1/5 strength throughout his bilateral lower extremities.
He noted umbilical sensitive level disorders.
Diagnosis assessment
MRI is considered the gold standard in the evaluation of sSDHs as it is capable of visualizing spinal hematomas as well as other spinal cord pathologies [1]. However, Braun et al. suggest performing spinal angiography when clinical suspicion of vascular malformation exists based on MRI findings [5]. We performed MRI in our case to assess of the diagnosis.
Management and follow up
The exact mechanism of spontaneous resolution of symptom is unclear. Several factors including small volume of hematoma prompt cease of active bleeding, flexibility of spinal cord, and appropriate width of spinal canal may influence on the recovery of the symptom [3].
Three treatment options exist in the management of sSDH: surgical evacuation, conservative medical management, and percutaneous drainage. Early symptoms without significant neurological deficits might considered for conservative management [6]. If only mild deficits are present, conservative management is reasonable. However, in the face of clinical deterioration or severe motor/sensory deficits, surgical evacuation is advised [7]. Percutaneous drainage might considered in cases where the hematoma is located dorsally and there is the absence of coagulopathy [8]. In our case, taking into account the signs of spinal cord compression Mc Cormick Grade IV, and the extent of the compressive hematoma, we retained the indication to operate the patient urgently. We perform laminectomy, durotomy to explore intradural and evacuated hematoma with gentle suction.
The mortality rates in patients with spontaneous non-traumatic sSDH have decreased in recent years and currently reported to be 1.3%. However, the associated morbidity, including serious neurologic deficits, is substantially higher and reported to be 28% [2]. Pereira et al. examined factors that predict outcome in patients with spontaneous no traumatic sSDH. Neurologic status at presentation was the strongest predictor of good outcomes; only 34% of patients with preexisting neurologic deficits had favourable outcomes compared to 83% of patients devoid of neurologic deficits at initial presentation [2]. In our case, patient had an immediate recovery of sensitivity and an onset of motor recovery from 1/5 to 2/5 follow up at on year with physiotherapy marked by recovery of motor deficit on upper to 4/5 and the lower extremities 4/5, he walk with walker help.
Conclusion
Spinal cord compression due to subdural spinal hematomas not often described especially in patients with haemostasis blood disorders due to anticoagulants drugs. In addition, we should pay attention with lumbar puncture in these patients and prefer general anaesthesia than spinal anaesthesia if they need emergency surgery. Emergency surgery allows a good prognosis about recovery of neurological disorders in selective case with compressive hematoma.
Availability of data and materials
Not applicable.
Abbreviations
- sSDH:
-
Spinal subdural hematoma
References
LA Rettenmaier, MT Holland, TJ Abel. Acute, nontraumatic spontaneous spinal subdural hematoma: a case report and systematic review of the literature. Hindawi case reports in neurological medicine, vol 2017, Article ID 2431041. https://doi.org/10.1155/2017/2431041
Pereira BJ, de Almeida AN, Muio VM, de Oliveira JG, de Holanda CV, Fonseca NC. Predictors of outcome in nontraumatic spontaneous acute spinal subdural hematoma: case report and literature review. World Neurosurg. 2016;89:574-577.e7. https://doi.org/10.1016/j.wneu.2015.11.010.
Oh SH, Han IB, Koo YH, Kim OJ. Acute spinal subdural hematoma presenting with spontaneously resolving hemiplegia. J Korean Neurosurg Soc. 2009;45(6):390–3. https://doi.org/10.3340/jkns.2009.45.6.390.
Domenicucci M, Ramieri A, Ciappetta P, Delfini R. Nontraumatic acute spinal subdural hematoma: report of five cases and review of the literature. J Neurosurg. 1999;91(1 Suppl):6573.
Braun P, et al. MRI findings in spinal subdural and epidural hematomas. Eur J Radiol. 2007;64(1):119–25. https://doi.org/10.1016/j.ejrad.2007.02.014.
Manish KK, Chandrakant SK, Abhay MN. Spinal subdural haematoma. J Orthop Case Rep. 2015;5(2):72–4. https://doi.org/10.13107/jocr.2250-0685.280.
Kyriakides AE, Lalam RK, El Masry WS. Acute spontaneous spinal subdural hematoma presenting as paraplegia: a rare case. Spine J. 2007;32(21):E619–22. https://doi.org/10.1097/BRS.0b013e318154c618.
Kang HS, Chung CK, Kim HJ. Spontaneous spinal subdural hematoma with spontaneous resolution. Spinal Cord. 2000;38(3):192–6. https://doi.org/10.1038/sj.sc.3100967.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MD: operate the case and the follow up, writing—original draft preparation. MH: operate the case and supervision for the writing. NEF: supervision. MREM: reviewing and editing, NDAB: writing—original draft preparation—reviewing and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have not any competing interests in this case report and any financial resources.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Denou, M., Bankole, N.D.A., Hamama, M. et al. Acute spinal cord compression due to spinal subdural hematoma after spinal anaesthesia in-patient under anticoagulant drug. Egypt J Neurosurg 36, 42 (2021). https://doi.org/10.1186/s41984-021-00138-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-021-00138-6