Abstract
Background
The incidence estimates for intracranial subdural empyema are 0.1 per 100,000 individuals, making it a rare clinical condition. It is a highly morbid and fatal illness that is most commonly the result of a primary infection somewhere else.
Case presentation
The authors present a young male patient 15 years presented with 1 week history of headache, fever, confusion and seizure attack with initial negative CT head and nearly negative CSF analysis. With few days he developed left sided weakness. MRI brain showed right temporoparietal subdural fluid collection with midline shift. Urgent neurosurgical evacuation was made and revealed subdural empyema. The boy received combination therapy of vancomycin, ceftriaxone, and metronidazole. The culture of the pus was negative but 16S rRNA gene sequencing (bacterial) revealed streptococcus intermedius. He made a good recovery with no recollection or neurological deficit on follow up.
Conclusion
This case highlights the possibility of occurrence of this rare infection in otherwise healthy individuals without obvious precipitating factor. It also indicates the superiority of MRI brain over CT head in detection of subdural collection. The rapid diagnosis and intervention improve the outcome of the patient.
Similar content being viewed by others
Background
A purulent loculated collection between the arachnoid and dura mater, subdural empyema can manifest both intracranially and spinally, albeit the former is more common. With an estimated incidence of 0.1 per 100,000 people, it is an uncommon condition especially in immunocompetent individual [1]. The most frequent predisposing illness for a subdural empyema is paranasal sinusitis. In addition, a direct infection of the subdural space during craniotomy or drainage of a subdural hematoma may exacerbate a subdural empyema during neurosurgical surgery [2]. A number of infectious agents have been linked to subdural empyemas; the Streptococcus milleri family is the most commonly isolated. Most of these empyemas manifest at the convexity of the brain with fever, confusion, and lateralizing neurological signs in some cases [3]. Early diagnosis and management of this neurosurgical emergency is directly correlated with patient’s morbidity and mortality [4]. Here, we discuss a case of subdural empyema in otherwise healthy secondary school student.
Case presentation
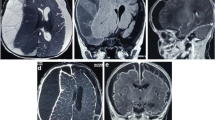
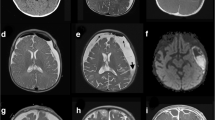
Our patient is a 15-year-old male, otherwise healthy secondary school student, with no previous medical comorbidities. He is the 3rd of 5 siblings who were also healthy with no chronic comorbidities. He is the result of non-consanguineous marriage with negative family history of any neurological disorders. He is left-handed. He presented with 1 weak history of headache, low grade fever and confusion. These were followed by one episode of generalized tonic–clonic seizures after which he presented to the emergency department (ED). Upon arrival to ED, He was confused and agitated, blood pressure 136/86, pulse 75/minute with normal sinus rhythm, feverish 38.3 °C and respiratory rate of 18/minute. Neurological examination was unremarkable with no lateralizing signs, bilateral round regular reactive pupils, no apparent cranial nerve affection, normal tone and reflexes in upper and lower limbs, bilateral equivocal planter response and no meningeal irritation signs. He underwent urgent non-contrast CT head which was unremarkable. His initial laboratory workup including complete blood picture, liver functions, kidney functions and electrolytes were all within normal except for mild neutrophilic leukocytosis (WBCs 12.7). C- reactive protein was elevated (197). An urgent lumbar puncture and CSF analysis was performed. CSF specimen was clear and contained only 8 red cells, 15 white cells, glucose and proteins within normal range. Impression of viral encephalitis was suspected, and he was initiated on acyclovir (15 mg/kg/dose/ 8 h), Ceftriaxone injections (2gm/ 12 h) and levetiracetam (500 mg /12 h). Later on, CSF PCR viral panel (which contains adenovirus, Herpes simplex 1and 2 viruses, EBV, CMV, Parvovirus, enterovirus, human herpes virus 6 and 7 and varicella zoster virus) was negative. The human immunodeficiency virus was negative. QuantiFERON gold test for TB was negative. Pancultures (blood, urine, CSF and sputum) were negative. After 3 days of admission, He was still confused with continuous low-grade fever (between 37.8 and 38.5 °C). EEG was obtained. It showed background activity of delta waves bilaterally with paroxysms of sharp spikes and spike slow waves more prominent on the right hemisphere. On day 4 of admission, he started to develop left sided weakness more prominent in upper limbs (Grade 3/5). Urgent MRI brain with contrast was obtained using 1.5 Tesla Phillips Intera® scanner (United States). It showed elongated frontoparietal subdural fluid collection with maximum diameter of 7 mm. It was associated with right cerebral hemisphere gyriform parenchymal diffusion restriction with adjacent pachymeningeal and leptomeningeal enhancement. There was midline shift to the left with 4–5 mm, Figs. 1, 2, 3. MRV and MRA were normal.
Urgent neurosurgical consultation was obtained and recommended urgent surgical intervention to evacuate this subdural collection. Intraoperatively, there was huge amount of pus upon opening of the dura. Evacuation and washing of this collection were done, Fig. 4. Sinuses were also explored for possible collection, but they were clear. There were no operative related complications. The patient was started on vancomycin injection (2gm/ 12 h), ceftriaxone injection (2 gm/12) and metronidazole injection (500 mg /8 h).
Next day post-operative, patient regained consciousness fully with slight delayed response. Left sided weakness improved fully with no residual deficit. On the 3rd day post-operative, he started to ambulate. Fever subsided and the patient returned back to his baseline. After 7 days post-operative, the patient underwent his midyears exams during his hospital stay. He was kept on IV antibiotics for 6 weeks. Cultures of the evacuated pus were negative but 16S rRNA gene sequencing (bacterial) revealed streptococcus intermedius. On follow up visit in the outpatient clinic, he was fully conscious with no neurological deficit or toxic manifestations. A follow up CT head was obtained and showed no recollection. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Neurosurgical emergencies such as subdural empyemas need to be recognized and treated quickly in order to preserve a favorable functional neurological outcome. If treatment is not received, these lesions advance quickly with neurological deficit, raise intracranial pressure, and result in coma and death in 24 to 48 h [5]. Subdural empyemas were previously encountered secondary to otitis media, but they are now more commonly observed as a consequence of bacterial sinusitis. They are most common in immunocompromised individuals but rarely occur in immunocompetent persons [6]. In some cases, the primary source cannot be identified. One study estimated that 3% of these empyemas have an unknown originating source. Males are more often than females to be diagnosed with subdural empyema, with average and median diagnosis ages of 46.1 and 49.5 years, respectively; that being said, the age range of patients with documented cases is incredibly wide [1]. Fever and headache are the most commonly reported presenting symptoms, and in this situation, they are linked to both increased intracranial pressure and infection. However, neurological presentations also could include altered mental status, seizures, dizziness, and focal neurological deficits as in our case [7]. When evaluating potential intracranial infectious lesions, CT of the head with intravenous contrast is frequently the first imaging modality of choice due to its accessibility. MRI with gadolinium contrast, as used in our case, is the gold standard imaging technique for subdural empyema diagnosis, though, because it is more sensitive than CT at imaging the dura and sinuses [4]. Although staphylococcus aureus and streptococcus milleri are of the most common organisms causing this condition, a broad-spectrum combination of antibiotics including high-dose vancomycin, high-dose third-generation cephalosporin, and metronidazole, should be used for a good period of time, most commonly 6–8 weeks [7]. Urgent neurosurgical intervention is usually needed for drainage of suppurative collection and to obtain culture material that could help targeting with sensitive antibiotic. Neurosurgical intervention could be either through a bur hole or through craniotomy as done in our case [8]. Subdural empyema reaccumulation after initial drainage is common, affecting up to 50% of patients and frequently requiring repeat surgical evacuation [9]. Patients with subdural empyema have a reported death rate of 6 to 15%, and a neurological disability in those who survive can reach 50 to 55%. Early and prompt management help to improve the outcome [8]. Without recent otitis media, sinusitis, or instrumentation in an otherwise immunocompetent patient, our case notably failed to identify a definitive source of infection; the subacute progressive presentation in an active young secondary school boy highlights the unusual presentation of this potentially fatal condition.
Conclusion
Due to the possibility of ambiguous early symptoms, intracranial suppurative consequences such subdural empyemas are uncommon and challenging to identify. In order to rule out cerebral spread, patients with sinus infections, worsening headaches, or other neurological impairments should have rigorous evaluations using CT or MRI imaging as indicated. Physicians must be aware of the hazards associated with subdural empyemas and the necessity of emergency neurosurgical intervention because these conditions can have substantial morbidity and mortality if they are not identified and treated promptly.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- ED:
-
Emergency department
- CT:
-
Computed tomography
- WBCs:
-
White blood cells
- CSF:
-
Cerebrospinal fluid
- EBV:
-
Epstein Barr virus
- CMV:
-
Cytomegalo virus
- TB:
-
Tuberculosis
- EEG:
-
Electroencephalogram
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance angiography
- MRV:
-
Magnetic resonance venography
- IV:
-
Intravenous
References
French H, Schaefer N, Keijzers G, Barison D, Olson S. Intracranial subdural empyema: a 10-year case series. Ochsner J. 2014;14(2):188–94.
Dakkak M, Cullinane R, Ramoutar R. Subdural empyema complicating bacterial meningitis: a challenging diagnosis in a patient with polysubstance abuse. Case Rep Med. 2015;12:2015.
Lundy P, Kaufman C, Garcia D, Partington D, Grabb PA. Intracranial subdural empyemas and epidural abscesses in children. J Neurosurg Pediatr. 2019;24(1):14–21.
Mortazavi M, Quadri A, Suriya S, Fard A, Hadidchi S, Adl H, et al. Rare concurrent retroclival and pan-spinal subdural empyema: review of literature with an uncommon illustrative case. World Neurosurgery. 2018;1(110):326–35.
Yang X, Chen B, Zhang Y, Yang Y, Xie S, He L, et al. Development of subdural empyema from subdural effusion after suppurative encephalitis: a case report. World J Clin Cases. 2023;11(10):2315.
Lu F, Yue T, Kung M. Salmonella group D1 subdural empyema mimicking subdural hematoma: a case report. Infect Drug Resist. 2022;1:6357–63.
Gorman J, Randhawa N, Mendelsohn D, Honey CR, Heran MK, Appel-Cresswell S. Subdural empyema. Can J Neurol Sci. 2018;45(5):566–7.
Bridwell E, Larson P, Yoo J, Oliver J. Subdural empyema in an immunocompetent active duty soldier: a case report. Mil Med. 2020;185(7–8):e1326–8.
Rebchuk D, Chang J, Griesdale E, Honey R. Non-contrast–enhancing subdural empyema: illustrative case. J Neurosurg. 2022. https://doi.org/10.3171/CASE22269.
Acknowledgements
The authors acknowledge all staff of Nizwa hospital, Oman for taking care of the patient and being helpful to the treating team. Also, we acknowledge our patient who agreed for publishing this report about his case.
Funding
Self-funding.
Author information
Authors and Affiliations
Contributions
AD contributed with preparing the manuscript. AH followed the patient up. AS collection of materials. WS was the acting surgeon and contributed in preparing the manuscript. ZF followed up the patient.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The case report was approved by the ethical committee of Nizwa hospital, MOH, sultanate of Oman, on 1/2/2024.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors alone are responsible for the content and writing of the paper. No conflict of interest is present.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dahshan, A., Youssef, A.H., Al Subhi, A. et al. The hidden threat: subdural empyema strikes a healthy teen. Egypt J Neurol Psychiatry Neurosurg 60, 74 (2024). https://doi.org/10.1186/s41983-024-00849-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00849-1