Abstract
Background
Alien limb is an involuntary movement that is considered a diagnostic feature of corticobasal degeneration syndrome. Few reports describe this condition in acute stroke, and most of them result from right parietal infarction.
Case presentation
This is a case of acute stroke presenting with a right-sided alien limb that was followed by right-sided weakness and aphasia. Effective management of the stroke was achieved through intravenous thrombolysis with the resolution of most symptoms except for a right-side sensory deficit. Magnetic resonance imaging of the brain showed acute parietal infarction involving the left sensory cortex.
Conclusions
Although very rare, right-sided alien limb can occur due left parietal infarction.
Similar content being viewed by others
Background
The alien hand is a rare clinical presentation that was first described in 1908 by Kurt Goldstein. However, the term “alien hand” was introduced in 1972 by Brion and Jedynak [1]. Clinically, alien hand refers to involuntary goal-directed movements affecting one limb [2] which can be associated with feeling “the hand is foreign” [3]. Alien hand was commonly considered a diagnostic feature of corticobasal degeneration syndrome [4]; however, it was also described with vascular and neoplastic lesions. Most cases described in literature had left alien limbs due to involvement of the right supplementary motor area, parietal cortex, anterior cingulate, corpus callosum, anterior prefrontal cortex, and thalamus [3]. Only a few cases with left hemispheric lesions were reported [4, 5]. Here, we report a stroke patient presenting with a right alien limb due to left parietal infarction.
Case presentation
A right-handed 66-year-old patient, with a history of hypertension and ischemic heart disease for which he was prescribed acetylsalicylic acid, atorvastatin, and bisoprolol. The past history was negative for any other vascular risk factor such as smoking, diabetes, dyslipidemia, hyperuricemia, previous stroke, or transient ischemic attacks. He presented to the stroke unit, within 2 h of symptom onset, with a sudden inability to control his right upper limb as his right upper limb was moving without his control. These involuntary movements lasted for half an hour, followed by severe weakness in his right upper limb. While he was transferred to the hospital, he developed complete right-sided weakness, impaired comprehension of spoken words, and difficulty expressing himself. On examination, he showed aphasia, receptive more than expressive, right-sided hemiplegia [Medical Research Council (MRC) scale grade 0 in upper and lower limb], and right-sided hemianesthesia including the face, right facial weakness, with a total National Institutes of Health Stroke Scale (NIHSS) of 16. Blood pressure on admission was 170/100 mm Hg. Random blood sugar was 121 mg/dl. The electrocardiogram (ECG) showed normal sinus rhythm.
Urgent computerized tomography (CT) scan of the brain using a 128-row MDCT scanner machine (GE 128, Optima 660,USA) was done and it excluded hemorrhage. The patient was diagnosed with acute ischemic stroke and received recombinant tissue plasminogen activator (rTPA) at a dose of 0.9 mg per kg with a total dose of 67.5 units.
The patient showed gradual improvement over the next day, with complete resolution of aphasia and improvement of right side weakness and NIHSS at 24 h was 4 (upper limb weakness grade 4 on MRC, right-sided hemihypesthesia and right facial weakness). There were no reported side effects for the intravenous thrombolytic therapy. Upon asking him about the initial involuntary movements, he stated: “My arm raised involuntarily above my head like a marionette, my right upper limb refused to respond to me, I couldn’t control my upper limb.”
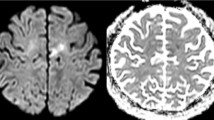
Magnetic resonance imaging (MRI) and angiography (MRA) of the brain were performed using a 1.5 T MR scanner (Achieva and Ingenia, Philips medical system, Eindhoven, Netherlands). The MRI showed a left parietal infarction involving the post-central gyrus (Fig. 1) while the MRA showed patent vessels. Carotid artery duplex was done using high-frequency linear probe 7–15 Mega Hz (Esoate My Lab Five, Italy) showed diffuse atherosclerosis.
The initial ECG showed sinus rhythm, and his subsequent inpatient cardiac monitoring was normal. However, paroxysmal atrial fibrillation needed to be excluded. The patient was scheduled for an outpatient Holter ECG monitoring, yet the Holter date was delayed due to the high demand rate in our hospital. The patient could not comply with the appointed date and did not follow up.
The patient reports improvement in his condition as he could speak and move independently, the main bothering residual symptom after 48 h was the complete loss of sensation over the right half of his body including the face. The patient was discharged after a few days on dual antiplatelet therapy.
The involuntary movements described as alien limbs are clinically categorized into “anarchic hand” a term used to identify the anterior variant, and “alien hand” for the “posterior” variant [3]. The anterior variant is further divided into frontal and callosal subtypes. The frontal subtype results from the affection of the dominant medial prefrontal cortex, supplementary motor area, cingulate cortex, or corpus callosum. It has features of frontal lobe affection such as groping (constant reaching for objects), grasping, or compulsive handling of things and nearby objects [6].
The callosal variant results from callosal injury and can present clinically with inter manual conflict [7] where hands seem to fight.
The posterior variant can result from a lesion affecting the thalamus, posterior parietal, or occipital lobe which can present clinically by less complex ataxic hand movements or involuntary levitation of the hand. These movements are often accompanied by intense sensory components characterized by a feeling of “foreignness” in the arm [5]. Hemianesthesia is a common association, as well [7].
Another classification grouped them into clinical subtypes as follows; firstly, (i) the ‘Diagnostic dyspraxia’ or intermanual conflict in which the left hand of a right-handed person contradicts or interferes with the actions of the right hand; (ii) the ‘Alien hand sign’ which also involves the left hand more often and in which the patient has the feeling that it’s not really his/her hand; (iii) the ‘Syndrome of the anarchic hand’ or way-ward hand, which affects the hand contralateral to the lesion as it performs goal-directed activity without the patient’s control or will; (iv) the ‘Supernumerary hands’, where the patient describes the sense of having an extra hand. Lastly, a rare presentation described in one case and termed ‘agonistic dyspraxia’ in which the patient would respond to a given command to use his right or left arm by performing it with the arm on the opposite side, with the patient’s subjective feeling that this contralateral arm movement was involuntary and with difficulty controlling it [8].
There are limited functional MRI data explaining the alien hand phenomenon, one study was performed in a stroke patient with parietal infarction [9] and the result of this study and other studies showed primary motor cortex (M1) activation [9, 10].
The left arm is more commonly the ‘alien’ one as most previous reports identify it with right-sided brain lesions [2, 4, 11].
Our patient’s condition mostly fits in the posterior type as he had a left-sided infarction involving the left/dominant parietal lobe. This pattern of the right alien limb is less commonly described in the literature, with only a few cases reported to have left-sided brain lesions [4, 5].
Also, the patient later developed right-sided severe weakness and aphasia, which suggests more involvement of the middle cerebral artery territory. Such a sequence of symptoms was rarely reported in the literature [12]. The patient was successfully treated with thrombolytic therapy and most of his symptoms resolved except for the right-sided hemianesthesia that possibly reflects the infarcted core at the left parietal cortex.
Conclusion
This is a case report that sheds light on one of the rare presentations of acute ischemic stroke, which describes an uncommon presentation of right-sided alien limb followed by a severe form of stroke involving the territory of the left middle cerebral artery. The MRI shows an interesting ischemic stroke that affected mainly the sensory cortex in the dominant parietal lobe. Although the patient improved, residual right-sided hemianesthesia persisted reflecting the ischemic core of the left parietal cortex.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CT:
-
Computerized tomography
- ECG:
-
Electrocardiogram
- MRA:
-
Magnetic resonance angiography
- MRC:
-
Medical Research Council
- MRI:
-
Magnetic resonance imaging
- NIHSS:
-
National Institutes of Health Stroke Scale
- RTPA:
-
Recombinant tissue plasminogen activator
References
Bru I, Verhamme L, Neve P, Maebe H. Rehabilitation of a patient with alien hand syndrome: a case report of a 61-year old man. J Rehabil Med Clin Commun. 2021;4(1):jrmcc0050.
Panikkath R, Panikkath D, Mojumder D, Nugent K. The Alien Hand Syndrome. Baylor Univ Med Center Proc. 2014;27(3):219–20.
Di Pietro M, Russo M, Dono F, Carrarini C, Thomas A, Di Stefano V, et al. A critical review of alien limb-related phenomena and implications for functional magnetic resonance imaging studies. Front Neurol. 2021;9:12.
Graff-Radford J, Rubin MN, Jones DT, Aksamit AJ, Ahlskog JE, Knopman DS, et al. The alien limb phenomenon. J Neurol. 2013;260(7):1880–8.
Kloesel B, Czarnecki K, Muir JJ, Keller AS. Sequelae of a left-sided parietal stroke: posterior alien hand syndrome. Neurocase. 2010;16(6):488–93.
Sarva H, Deik A, Severt WL. Pathophysiology and treatment of alien hand syndrome. Tremor Other Hyperkinet Movem. 2014;4:241.
Josephs KA, Rossor MN. The alien limb. Pract Neurol. 2004;4(1):44–5.
Aboitiz F, Carrasco X, Schröter C, Zaidel D, Zaidel E, Lavados M. The alien hand syndrome: classification of forms reported and discussion of a new condition. Neurol Sci. 2003;24(4).
Assal F, Schwartz S, Vuilleumier P. Moving with or without will: functional neural correlates of alien hand syndrome. Ann Neurol. 2007;62(3):301–6.
Onofrj M, Bonanni L, Delli Pizzi S, Caulo M, Onofrj V, Thomas A, et al. Cortical activation during levitation and tentacular movements of corticobasal syndrome. Medicine. 2015;94(45): e1977.
Demiryürek BE, Gündogdu AA, Acar BA, Alagoz AN. Paroxysmal posterior variant alien hand syndrome associated with parietal lobe infarction: case presentation. Cogn Neurodyn. 2016;10(5):453–5.
Espinosa PS, Smith CD, Berger JR. Alien hand syndrome. Neurology. 2006;67(12):E21–E21.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
NE was accountable for the design and conceptualization of the study, and contributed to scientific writing. MM was responsible for acquisition of clinical data, and critical revision. FF was responsible for interpretation of data, writing the manuscript and critically revising manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee at the faculty of medicine, Ain shams University on the 10th of October, 2023 (Ethical approval number R278/2023). Written informed consent was obtained from the patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El Nahas, N., Maged, M. & Kenawy, F.F. Right-sided alien hand in acute parietal infarction: a case report. Egypt J Neurol Psychiatry Neurosurg 60, 33 (2024). https://doi.org/10.1186/s41983-024-00812-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00812-0