Abstract
Background
Knowledge of the predisposing risk factors and prompt recognition of the warning signs for heart attack and stroke is fundamental in modification of lifestyle behaviors and an imperative precursor to health-seeking behavior. In view of an existing knowledge gap amidst increasing incidence of heart attack and stroke in Tanzania, we conducted this community-based cross-sectional study among residents of Dar es Salaam city.
Results
A total of 1759 respondents were enrolled in this study. The mean age was 45.4 years, females constituted over a half of participants and over two-thirds had attained at least secondary school education. Regarding risk factors, just over 2% of participants displayed satisfactory awareness and only stress was recognized by at least half of participants. With regard to warning signs, barely 1% of participants had satisfactory knowledge for either of the conditions while nearly three-quarters of participants failed to mention even a single warning sign for heart attack. Recognized by about two-thirds of respondents, sudden numbness or weakness in face, arm or leg was the most acknowledged stroke symptom; however, other symptoms were familiar to less than a third of participants. Although over a half of respondents acknowledged going to a hospital as their first resort, over one-tenth of respondents expressed inappropriate reactions towards heart attack and stroke victims. Old age, higher level of education, positive history of heart attack or stroke, high blood pressure and history of dyslipidemia showed association with both risk factors and warning signs knowledge during bivariate analyses.
Conclusions
Public knowledge of common risk factors and typical warning signs for heart attack and stroke was critically suboptimal. These findings herald an utmost need for public health efforts to increase community awareness of risk factors and typical signs of the two conditions to curb the rising prevalence and associated morbimortality.
Similar content being viewed by others
Background
As the epidemiologic transition continues to transform the disease landscape in low- and middle-income countries, an upsurge of acute coronary syndromes (ACS) and stroke is increasingly realized as an epidemic of public health importance particularly in the sub-Saharan Africa (SSA) region [1,2,3,4,5,6]. Globally, over 200 million people are diagnosed with ischemic heart disease ( ̴3 million succumb to heart attack) while nearly 90 million persons are affected by stroke every year [7, 8]. Apart from being the leading contributors to the global burden of disease, heart attack and stroke top the global mortality list (8.8 million and 7.1 million deaths, respectively) and are projected to remain so coming 2030 [8,9,10]. Despite of mounting evidence for the burgeoning incidence of ischemic heart disease (IHD), Tanzania lacks the respective national representative estimates but a recently published article from the northern part of the country revealed a 59.9% acute myocardial infarction (MI) mortality at 1 year [11, 12]. Moreover, with an annual incidence of up to 316 strokes per 100,000 individuals and a 50% 90-day mortality rate, Tanzania is among the most affected nations [13]. Furthermore, with the estimated global management cost amounting to US$ ̴1 trillion/year, ACS and stroke have considerable economic ramifications among residents of Dar es Salaam city [14, 15].
Heart attack and stroke are medical emergencies that necessitate immediate symptom recognition, rapid emergency transport and prompt management decisions. However, despite remarkable advances in revascularization techniques and stroke therapy, the general public largely remains uninformed about the two conditions and a substantial fraction of heart attack and stroke victims die before accessing medical care [16, 17]. Clinical outcomes of heart attack and stroke are principally time-dependent, however temporal trends suggests that despite improved emergency services and health education programs, prehospital delay constitutes the majority (> two-thirds) of delays to treatment [18,19,20,21]. For instance, despite significant reduction in door-to-balloon time in acute MI management, majority of patients seek medical attention way beyond the optimal time for reperfusion albeit experiencing prodromal symptoms for several hours [22]. While a key public health strategy to curb heart attack and stroke morbimortality is to increase the symptomology knowledge, the awareness of such at the community level is seldom given attention. In view of an existing epidemiological gap regarding the knowledge of heart attack and stroke risk factors and warning signs, we conducted this community-based cross-sectional study.
Methods
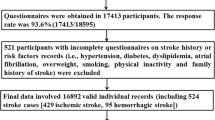
This cross-sectional community-based survey was conducted in Dar es Salaam city between August 2022 and April 2023. Located in the east coast of the country and covering an area of 1393 km2, Dar es Salaam region is the largest city and financial hub of Tanzania. The metro area population of Dar es Salaam as per the 2022 census is 5,383,728 and it encompass 1,550,066 households. A random pre-selection of specific blocks was utilized to select a random sample of 1759 households based on the 2022 Demographic and Health Survey and Malaria Indicator Survey census frame. Within each household, the person aged at least 18 years whose birthday was the earliest in the calendar year was eligible to participate in the study. As a mitigation to minimize potential bias, persons with medical-related occupations were not eligible. Face-to-face questionnaire-based interviews were administered to the participants. This study utilized a validated standardized questionnaire that was developed by Ahmed and colleagues which has been used in numerous scholarly works [23]. The aforementioned data collection tool consists of three domains including sociodemographic and clinical characteristics, awareness of risk factors and knowledge of heart attack and stroke warning signs. Closed-ended questions were used for all knowledge assessments. Each respondent was asked to mention as many (as they can) risk factors and warning symptoms for heart attack and stroke, respectively. Respondents’ verbatim responses were recorded in the respective questionnaire space (using appropriate medical terms) until the respondent declared to know no more. Height and weight measurements were taken using Digital Phoenix Pbmi-200p BMI Machine (India) to calculate body mass index (BMI).
We defined a priori eleven risk factors (aging, smoking, alcoholism, stress, physical inactivity, overweight, unhealthy diet, genetics, hypertension, diabetes, and hypercholesterolemia) for heart attack/stroke; eight heart attack warning signs (chest pain, arms/shoulder pain, neck/jaw/back pain, diaphoresis, shortness of breath, lightheadedness/fainting, epigastric pain, and nausea/vomiting), and six typical symptoms (sudden unilateral numbness/weakness of the face, arm or leg; sudden trouble with walking/loss of balance; sudden trouble with speaking/understanding; sudden severe headache; sudden difficulty in seeing, and nausea/vomiting) of stroke. A respondent could therefore score between 0 and 11, 0 and 8, and 0 and 6, respectively, depending on the correctly identified parameters. As emergency services (like 911, 112, and others), are not readily available in this setting, we regarded “taking the patient to the hospital” as the appropriate response for the action to be taken in case of stroke or heart attack. Owing to the fact that heart attack and stroke are vascular events that necessitate rapid symptom recognition and prompt seeking of medical care, the questions for heart attack and stroke symptoms were grouped on a composite basis for analysis. Nonetheless, respective scores for heart attack and stroke were examined separately by descriptive statistics. A cut off of > 50% was used to denote satisfactory knowledge as well as in comparison of knowledge level among different strata [24].
All statistical analyses utilized STATA v15.0 software. Categorical data are expressed as frequency (percentage), whereas continuous data are displayed as means (standard deviation). Pearson Chi-square and Student’s t-test were employed in comparison categorical and continuous variables, respectively. Factors associated with respective knowledge were assessed by bivariate analyses. We report mean scores and p-values where appropriate. All tests were 2-sided and p < 0.05 was used to signify statistical significance.
Results
A total of 1759 respondents were enrolled in this study. Table 1 displays the social and demographic characteristics of participants. The mean age was 45.4 years and just less than three-quarters of participants were aged less than 55 years. Females constituted over a half (55.3%) of participants and over two-thirds (70%) had attained at least secondary school education. Over three-quarters (80.8%) of respondents had a regular income generating activity and over 84% resided in urban area. About 3% were current smokers, nearly a quarter (24.6%) were alcohol drinkers and 71.7% had excess body weight. With regard to disease history, about a third (31.1%) of participants were hypertensive, 6.9% had history of diabetes, and 11.5% had positive history of hypercholesterolemia.
A total of 118 (6.7%) and 49 (2.8%) respondents had personal history of heart attack and stroke, respectively, while 216 (12.3%) and 518 (29.5%) participants had positive family history of such. Overall, 664 (37.8%) respondents had a perception of being at risk of heart attack or stroke. Although smokers displayed similar risk perception compared to non-smokers (47.3% versus 37.5%, p = 0.14); participants with age ≥ 55 (45.8% versus 34.7%, p < 0.001), positive family history of heart attack (52.8% versus 35.6%, p < 0.001), positive family history of stroke (46.7% versus 34.0%, p < 0.001), history of hypercholesterolemia (58.1% versus 35.1%, p < 0.001), BMI ≥ 25 (40.1% versus 31.7%, p < 0.001), diabetes (53.3% versus 36.6%, p < 0.001) and hypertension (51.0% versus 31.8%, p < 0.001) displayed superior risk perception compared to their respective counterparts.
Figure 1 displays the respondents’ knowledge of heart attack and stroke risk factors. Overall the mean score was 17.6% and 38 (2.2%) scored above 50%. Stress (57.5%), unhealthy diet (35.5%) and hypertension (26.6%) were the most recognized risk factors. Other factors including overweight (16.8%), physical inactivity (15.4%), alcoholism (11%), hypercholesterolemia (8.9%), diabetes (8.7%), smoking (5.6%), aging (4.1%) and positive family history (3.1%) were recognized at lesser frequencies. Eight (0.5%) participants mentioned witchcraft as a risk factor for heart attack and stroke while a total of 322 (18.3%) participants failed to correctly mention even a single risk factor.
Figures 2 and 3 display the respondents’ knowledge of heart attack and stroke, respectively. The mean score for knowledge of heart attack warning signs was 4.7% and 12 (0.7%) respondents scored more than 50%. Regarding heart attack, nearly three-quarters (72.7%) of participants failed to mention even a single warning sign. Nevertheless, shortness of breath (15.6%), lightheadedness (11.5%) and chest pain (7.7%) were the most recognized signs followed by diaphoresis (5.5%), arms/shoulder pain (1.9%), neck/jaw/back pain (1.9%), nausea/vomiting (0.6%) and epigastric pain 0.3%. With regard to stroke, over 29% of respondents could not mention a single warning sign. The mean score for knowledge of stroke warning signs was 19.8% and 17 (1.0%) respondents scored more than 50%. Sudden numbness or weakness in face, arm or leg was the most (62.7%) mentioned risk followed by sudden trouble walking or loss of balance (28.8%), sudden trouble speaking or understanding (20%), sudden severe headache (4.7%), sudden trouble seeing (2.2%) and nausea/vomiting (0.2%).
Regarding respondent’s planned response when oneself or closed one succumb to heart attack or stroke, 1035 (58.8%) said they would go immediately to the hospital (Fig. 4). Furthermore, 209 (11.9%) respondents’ expressed inappropriate reactions towards heart attack and stroke victims including; keep victim in open air 84(4.8%), prick the toes to bleed 26(1.5%), hit the victim’s head with slippers 9(0.5%), rub the patient with toilet dirt 7(0.4%), run away 5(0.3%), visit a witch doctor 5(0.3%), oil massage 5(0.3%), pray 4(0.2%) and giving fluid sips 2(0.1%). A total of 515(29.3%) respondents did not know how to respond.
Table 2 displays comparative analysis of risk factors and warning signs knowledge of heart attack and stroke across various subgroups. Although age differences displayed similar knowledge regarding risk factors, those aged 55 year or more displayed superior mean knowledge scores for both heart attack (5.4 versus 4.4, p < 0.05) and stroke (22.4 versus 18.8, p < 0.001) warning signs compared to those aged less than 55 years. Sex differences displayed similar risk factors and stroke signs knowledge, however, females displayed more knowledge of heart attack signs compared to males (5.2 versus 4.1, p = 0.01). With regard to education, respondents with secondary education or higher displayed superior mean knowledge scores in risk factors (5.0 versus 4.1, p < 0.001) and stroke signs (20.7 versus 17.7, p < 0.001) compared to their counterparts with at most primary education. Similarly, non-smokers displayed superior means in risk factors (17.7 versus 12.9, p < 0.01) and stroke signs (20.0 versus 12.7, p < 0.01) knowledge compared to current smokers. Participants with excess body weight had better knowledge mean for risk factors (18.6 versus 15.1, p < 0.001) and stroke signs (20.5 versus 17.9, p < 0.01) compared to respondents with BMI < 25. Participants with hypertension had better means across all knowledge categories [risk factors (19.7 versus 16.6, p < 0.001), heart attack signs (6.8 versus 3.8, p < 0.001) and stroke signs (22.8 versus 18.4, p < 0.001)] compared to normotensive individuals. Although they displayed similar risk factors and stroke signs knowledge, participants with diabetes exhibited better knowledge of heart attack symptoms (6.9 versus 4.6, p < 0.01) compared to diabetes-free individuals. Participants with history of hypercholesterolemia displayed superior knowledge means across all categories [risk factors (13.9 versus 12.6, p < 0.001), heart attack signs (11.7 versus 8.9, p < 0.001), and stroke signs (24.6 versus 19.2, p < 0.001)] compared to their counterparts with negative history. Lastly, participants with positive personal and family history of heart attack, positive family history of stroke and those with self-perception of being at risk for heart attack or stroke displayed superior knowledge means across all groups compared to their respective counterparts.
Discussion
The growing burden of heart attack and stroke are increasingly exposing the unprepared state of most health-care systems in the developing world, more so the SSA region. It is evident that the improved clinical outcomes and survival prospects conferred by percutaneous coronary intervention (PCI) and thrombolysis are time-dependent. Owing to this, knowledge of the predisposing risk factors and prompt recognition of the warning signs for heart attack and stroke is fundamental in modification of lifestyle behaviors and an imperative precursor to health-seeking behavior. Likewise, lack of the aforementioned knowledge inevitably leads to delay in summoning medical attention which potentially leads to ineligibility for prompt intervention ultimately resulting in increased morbidity and premature mortality.
Just like any other non-communicable disease (NCD), the likelihood of occurrence of heart attack or stroke has been linked to the coexistence of modifiable risk factors. Parallel to recent studies [25,26,27,28,29] conducted in this setting, nearly three-quarters of the respondents in this present study had at least one of the three biological risk factors including excess body weight, hypertension or diabetes. However, despite these high rates of biological risk factors, about one-fifth of participants could not mention even a single risk factor for heart attack or stroke. Variable rates (9.4–91.4%) of complete unawareness of risk factors has been reported by previous studies [30,31,32,33,34,35,36,37] and our observed rates are within this wide range which could potentially be explained by the differences in knowledge assessment methods and population characteristics across studies. Nonetheless, in contrast to our expectations, this present study revealed significantly lower knowledge level compared to an earlier study [26] conducted in the same setting. Moreover, similar to the cited earlier local study, a disconnection between knowledge and practice was also observed in this present study. This observation raises serious concerns and warrants concerted public health efforts to increase not only awareness but knowledge retention and practice as well.
As the only risk factor to be mentioned by over a half of participants, stress was the most recognized risk factor in this study. In consonance to our findings, stress (57.3%) was the most familiar risk factor in an Ethiopian study by Workina and colleagues [33]. Although different studies [24, 30,31,32,33,34,35,36,37,38,39,40,41,42] have displayed diverse frequency pattern of acknowledged risks, the documented public knowledge of heart attack and stroke across the globe is largely unsatisfactory. Furthermore, the absence of an obvious pattern of recognized risks among studies implies that educational strategies across different populations ought to be tailored to address respective knowledge deficiencies. Surprisingly, even in this era, witchcraft was among the risk factors mentioned by respondents from a major economic city in the SSA region. Although in none of the reviewed studies from the western world was witchcraft mentioned, it was reported by numerous earlier studies from the African continent including Nigeria, Malawi and Uganda [35, 37, 40, 43]. Such superstitious beliefs particularly in the developing world play a notable role in causing delays in access to care and deter the attainment of Sustainable Development Goals (SDGs) at large.
Following heart attack or stroke, victims’ ability to recognize symptoms and to take appropriate action is central if desirable outcomes are to be achieved. With less than one percent of participants displaying satisfactory knowledge of either heart attack or stroke warning signs, respondents from this study exhibited critically low awareness of typical symptomatology particularly of heart attack (about three-quarters of respondents failed to mention a single sign). Whereas chest pain was the most identified heart attack symptom in literally all previous studies [24, 39,40,41, 44,45,46,47,48,49,50,51], participants of this study recognized shortness of breath and lightheadedness ahead of chest pain an observation which is quite similar to a Hertz and colleagues study [52] from the Northern part of the country. Furthermore, contrary to heart attack where the most recognized warning sign was identified by less than one-fifth of participants; in stroke’s case, sudden numbness or weakness in face, arm or leg was impressively acknowledged by almost two-thirds of the respondents. The observation of unilateral weakness/paralysis as the most familiar stroke sign from this present study echoes findings from numerous preceding studies [32, 33, 38, 44, 45, 47, 48, 50, 51]. Nevertheless, other stroke symptoms in this study were familiar to less than a third of participants. Moreover, corroborating the findings of several previous studies, we found significant differences in knowledge across groups defined by age [30, 31, 34], level of education [30, 31, 33, 35, 36, 38, 39], history of heart attack or stroke [30, 31, 34, 39], hypertension [30] and history of dyslipidemia [30, 34]. In general, these observations indicate the urgent desirability of improving the level of public awareness of heart attack and stroke typical presentations. Furthermore, as the constellation of symptoms differ among patients, it is pivotal that educational messages recognize and address the diversity and variability of the typical signs.
Regarding the suitable actions for someone suffering from heart attack or stroke, nearly three-fifths of the respondents appropriately said they would go immediately to the hospital. Such observation resonates with numerous other studies where over a half of respondents’ first resort was the hospital [30, 32, 37, 40, 44, 45, 48, 51, 53, 54]. However, given the aforementioned critically low knowledge of risk factors and warning signs, this present study underscore a vivid gap between taking suitable action and ability to spot the typical signs in the first place. Furthermore, these findings raise serious concerns on the methods used by the health-care providers to ensure effective transmission and retention of heart attack and stroke basic knowledge. Perhaps, the most surprising finding of this study was that over one-tenth of the respondents’ expressed inappropriate planned reactions some of which are quite precarious (including prick the toes to bleed, hit the victim’s head with slippers, rub the patient with toilet dirt and run away). The aforementioned reactions have not been reported by any of the previous studies; however, other odd responses including giving fluid sips [45], faith healing [32, 43, 53, 55], oil massage [53, 55] and visiting a witch doctor [55, 56] have been documented. Such myths, particularly in the SSA region remain a stumbling block towards the battle against NCDs and calls for deliberate efforts to debunk cognate health-related misinformation.
The strengths of our study include a sufficiently large sample to estimate the awareness of stroke and heart attack warning signs with adequate precision. Furthermore, we used door-to-door population-based sampling and standardized tools for knowledge assessment to reduce selection and information bias. However, the likelihood of some healthy participation bias and imprecision in the estimates resulting from both open and closed questions cannot be precluded.
Conclusions
Despite portraying an averagely acceptable planned response to heart attack or stroke, public knowledge of common risk factors and typical warning signs was critically suboptimal. These findings have crucial implications for both health policy and further research particularly in this era where heart attack and stroke incidence is rapidly rising in Tanzania and elsewhere. Furthermore, these observations somewhat divulge the incompetency of the health-care system to recognize and educate high risk individuals and general public at large. These findings herald an utmost need for public health efforts to increase community awareness of risk factors and typical signs of the two conditions to curb the rising prevalence and associated morbimortality. A comprehensive mass media campaign, targeted education of high risk groups (including their families), and tailored eHealth interventions will be rewarding in a setting like this one. Moreover, educational endeavors should also target health-care professionals, particularly the primary care providers.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndrome
- BMI:
-
Body mass index
- ECG:
-
Electrocardiogram
- ECHO:
-
Echocardiography
- IHD:
-
Ischemic heart disease
- MI:
-
Myocardial infarction
- NCDs:
-
Non-communicable disease
- PCI:
-
Percutaneous coronary intervention
- SD:
-
Standard deviation
- SDGs:
-
Sustainable development goals
- SSA:
-
Sub-Saharan Africa
References
Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi SKBM, AlKatheeri R, et al. Global epidemiology of ischemic heart disease: results from the Global Burden of Disease Study. Cureus. 2020;12(7): e9349.
Sagui E. Stroke in sub-Saharan Africa. Med Trop. 2007;67(6):596–600.
Ezejimofor MC, Chen YF, Kandala NB, Ezejimofor BC, Ezeabasili AC, Stranges S, et al. Stroke survivors in low- and middle-income countries: a meta-analysis of prevalence and secular trends. J Neurol Sci. 2016;364:68–76.
Adeloye D. An estimate of the incidence and prevalence of stroke in Africa: a systematic review and meta-analysis. PLoS ONE. 2014;9(6): e100724.
Thrift AG, Cadilhac DA, Thayabaranathan T, Howard G, Howard VJ, Rothwell PM, et al. Global stroke statistics. Int J Stroke. 2014;9(1):6–18.
Walker R, Whiting D, Unwin N, Mugusi F, Swai M, Aris E, et al. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. Lancet Neurol. 2010;9(8):786–92.
Kim SJ. Global awareness of myocardial infarction symptoms in general population. Korean Circ J. 2021;51(12):997–1000.
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–639.
World Health Organization. Projections of mortality and causes of death, 2015 and 2030. Health statistics and information systems. 2013. http://www.who.int/entity/healthinfo/global_burden_disease/GHE_DthGlobal_Proj_2015_2030.xls?ua=1. Accessed 30 Mar 2023.
Adem F, Abdi S, Amare F, Mohammed MA. In-hospital mortality from acute coronary syndrome in Africa: a systematic review and meta-analysis. SAGE Open Med. 2023;11:20503121221143650.
Hertz JT, Madut DB, Rubach MP, William G, Crump JA, Galson SW, et al. Incidence of acute myocardial infarction in Northern Tanzania: a modeling approach within a prospective observational study. J Am Heart Assoc. 2021;10(15): e021004.
Hertz JT, Sakita FM, Kweka GL, Tarimo TG, Goli S, Prattipati S, et al. One-year outcomes and factors associated with mortality following acute myocardial infarction in Northern Tanzania. Circ Cardiovasc Qual Outcomes. 2022;15(4): e008528.
Regenhardt RW, Biseko MR, Shayo AF, Mmbando TN, Grundy SJ, Xu A, et al. Opportunities for intervention: stroke treatments, disability and mortality in urban Tanzania. Int J Qual Health Care. 2019;31(5):385–92.
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18–29.
Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care. 2009;15:S36–41.
Centers for Disease Control and Prevention (CDC). State-specific mortality from stroke and distribution of place of death—United States, 1999. MMWR Morb Mortal Wkly Rep. 2002; 51(20):429–33.
Law MR, Watt HC, Wald NJ. The underlying risk of death after myocardial infarction in the absence of treatment. Arch Intern Med. 2002;162(21):2405–10.
Terecoasă EO, Radu RA, Negrilă A, Enache I, Cășaru B, Tiu C. Pre-Hospital Delay in Acute Ischemic Stroke Care: Current Findings and Future Perspectives in a Tertiary Stroke Center from Romania-A Cross-Sectional Study. Medicina (Kaunas). 2022;58(8):1003.
Chowdhury IZ, Amin MN, Chowdhury MZ, Rahman SM, Ahmed M, Cader FA. Pre hospital delay and its associated factors in acute myocardial infarction in a developing country. PLoS ONE. 2021;16(11): e0259979.
Feng L, Li M, Xie W, Zhang A, Lei L, Li X, et al. Prehospital and in-hospital delays to care and associated factors in patients with STEMI: an observational study in 101 non-PCI hospitals in China. BMJ Open. 2019;9(11): e031918.
Fladt J, Meier N, Thilemann S, Polymeris A, Traenka C, Seiffge DJ, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc. 2019;8(20): e013101.
Rafi A, Sayeed Z, Sultana P, Aik S, Hossain G. Pre-hospital delay in patients with myocardial infarction: an observational study in a tertiary care hospital of northern Bangladesh. BMC Health Serv Res. 2020;20:633.
Ahmed AAA, Al-Shami AM, Jamshed S, Nahas ARF. Development of questionnaire on awareness and action towards symptoms and risk factors of heart attack and stroke among a Malaysian population. BMC Public Health. 2019;19(1):1300.
Khan NS, Shehnaz SI, Guruswami GK, Ibrahim SAM, Mustafa SAJ. Knowledge of warning signs, presenting symptoms and risk factors of coronary heart disease among the population of Dubai and Northern Emirates in UAE: a cross-sectional study. Nepal J Epidemiol. 2017;7(2):670–80.
Pallangyo P, Mkojera ZS, Hemed NR, Swai HJ, Misidai N, Mgopa L, et al. Obesity epidemic in urban Tanzania: a public health calamity in an already overwhelmed and fragmented health system. BMC Endocr Disord. 2020;20(1):147.
Pallangyo P, Komba M, Mkojera ZS, Mayala HA, Bhalia SV, Millinga J, et al. Non-communicable disease risk factors among caregivers of patients attending a tertiary cardiovascular hospital in Tanzania. Int J Gen Med. 2022;15:4685–96.
Pallangyo P, Mgopa LR, Mkojera Z, Komba M, Millinga J, Misidai N, et al. Obstructive sleep apnea and associated factors among hypertensive patients attending a tertiary cardiac center in Tanzania: a comparative cross-sectional study. Sleep Sci Pract. 2021;5:17.
Pallangyo P, Mkojera ZS, Komba M, Mgopa LR, Bhalia S, Mayala H, et al. Burden and correlates of cognitive impairment among hypertensive patients in Tanzania: a cross-sectional study. BMC Neurol. 2021;21:433.
Pallangyo P, Misidai N, Komba M, Mkojera Z, Swai HJ, Hemed NR, et al. Knowledge of cardiovascular risk factors among caretakers of outpatients attending a tertiary cardiovascular center in Tanzania: a cross-sectional survey. BMC Cardiovasc Disord. 2020;20:364.
Sug Yoon S, Heller RF, Levi C, Wiggers J, Fitzgerald PE. Knowledge of stroke risk factors, warning symptoms, and treatment among an Australian urban population. Stroke. 2001;32(8):1926–30.
Agbetou Houessou M, Hountada H, Yahouédéou B, Choki B, Kossi O, Adoukonou T. Knowledge of stroke risk factors and signs in Parakou, a Northern City of Benin in West Africa. Cerebrovasc Dis. 2021;50(1):88–93.
Osama A, Ashour Y, El-Razek RA, Mostafa I. Public knowledge of warning signs and risk factors of cerebro-vascular stroke in Ismailia Governorate, Egypt. Egypt J Neurol Psychiatry Neurosurg. 2019;55:31.
Workina A, Kebede S, Fekadu C, Wubetie SA. Knowledge of risk factors and warning signs of stroke among patients with heart disease at Tikur Anbessa Specialized Hospital. Open Access Emerg Med. 2021;13:57–66.
Ahmed AAA, Al-Shami AM, Jamshed S, Zawiah M, Elnaem MH, Mohamed Ibrahim MI. Awareness of the risk factors for heart attack among the general public in Pahang, Malaysia: a cross-sectional study. Risk Manag Healthc Policy. 2020;23(13):3089–102.
Nakibuuka J, Sajatovic M, Katabira E, Ddumba E, Byakika-Tusiime J, Furlan AJ. Knowledge and perception of stroke: a population-based survey in Uganda. ISRN Stroke. 2014. https://doi.org/10.1155/2014/309106.
Hickey A, O’Hanlon A, McGee H, Donnellan C, Shelley E, Horgan F, et al. Stroke awareness in the general population: knowledge of stroke risk factors and warning signs in older adults. BMC Geriatr. 2009;5(9):35.
Mvula H, Chisambo C, Nyirenda V, Geis S, Glynn JR, Crampin AC, et al. Community-level knowledge and perceptions of stroke in rural Malawi. Stroke. 2019;50(7):1846–9.
Falavigna A, Teles AR, Vedana VM, Kleber FD, Mosena G, Velho MC, et al. Awareness of stroke risk factors and warning signs in southern Brazil. Arq Neuropsiquiatr. 2009;67(4):1076–81.
Intas G, Tsolakoglou J, Stergiannis P, Chalari E, Eleni C, Fildissis G. Do Greek citizens have minimum knowledge about heart attack? A survey. Health Sci J. 2015;9(5):1–6.
Kolo PM, Ogunmodede JA, Sanya EO, Bello HS, Ghadamosi MS, Dele-Ojo B, et al. Public knowledge of heart attack symptoms and prevalence of self-reported cardiovascular risk factors in Ilorin, Nigeria. Nig J Cardiol. 2015;12:95–100.
Basham K, Aldubaikhi A, Sulaiman I, Alhaider A, Alrasheed A, Bahanan F, et al. Public awareness of early symptoms of acute myocardial infarction among Saudi population. J Fam Med Prim Care. 2021;10(10):3785–90.
Kharbach A, Obtel M, Achbani A, Bouchriti Y, Hassouni K, Lahlou L, et al. Level of knowledge on stroke and associated factors: a cross-sectional study at primary health care centers in Morocco. Ann Glob Health. 2020;86(1):83.
Akinyemi RO, Ogah OS, Ogundipe RF, Oyesola OA, Oyadoke AA, Ogunlana MO, et al. Knowledge and perception of stroke amongst hospital workers in an African community. Eur J Neurol. 2009;16(9):998–1003.
Lee C, Chow CM, Yan AT, Moe GW, Tu JV, Chu JY. Awareness of warning symptoms of heart disease and stroke: results of a follow-up study of the Chinese Canadian Cardiovascular Health Project. CJC Open. 2021;3(6):741–50.
Luan S, Yang Y, Huang Y, McDowell M. Public knowledge of stroke and heart attack symptoms in China: a cross-sectional survey. BMJ Open. 2021;11(1): e043220.
Whitaker S, Baldwin T, Tahir M, Choudhry O, Senior A, Greenfield S. Public knowledge of the symptoms of myocardial infarction: a street survey in Birmingham, England. Fam Pract. 2012;29(2):168–73.
Haq A, Masnarivan Y, Yenti M, Fadhilla N. Assessment of public knowledge of heart attack and stroke in West Sumatra Province. Malay J Public Health Med. 2022;22(3):124–9.
Han CH, Kim H, Lee S, Chung JH. Knowledge and poor understanding factors of stroke and heart attack symptoms. Int J Environ Res Public Health. 2019;16(19):3665.
Abdo Ahmed AA, Mohammed Al-Shami A, Jamshed S, Fata Nahas AR, Mohamed Ibrahim MI. Public awareness of and action towards heart attack symptoms: an exploratory study. Int J Environ Res Public Health. 2020;17(23):8982.
Quah JL, Yap S, Cheah SO, Ng YY, Goh ES, Doctor N, et al. Knowledge of signs and symptoms of heart attack and stroke among Singapore residents. Biomed Res Int. 2014;2014: 572425.
Van Hooser JC, Rouse KL, Meyer ML, Siegler AM, Fruehauf BM, Ballance EH, et al. Knowledge of heart attack and stroke symptoms among US native American adults: a cross-sectional population-based study analyzing a multi-year BRFSS database. BMC Public Health. 2020;20(1):40.
Hertz JT, Madut DB, Tesha RA, William G, Simmons RA, Galson SW, et al. Knowledge of myocardial infarction symptoms and perceptions of self-risk in Tanzania. Am Heart J. 2019;210:69–74.
Pandian JD, Jaison A, Deepak SS, Kalra G, Shamsher S, Lincoln DJ, et al. Public awareness of warning symptoms, risk factors, and treatment of stroke in northwest India. Stroke. 2005;36(3):644–8.
Hertz JT, Madut DB, William G, Maro VP, Crump JA, Rubach MP. Perceptions of stroke and associated health-care-seeking behavior in Northern Tanzania: a community-based study. Neuroepidemiology. 2019;53(1–2):41–7.
Das S, Das SK. Knowledge, attitude and practice of stroke in India versus other developed and developing countries. Ann Indian Acad Neurol. 2013;16(4):488–93.
Al Shafaee MA, Ganguly SS, Al Asmi AR. Perception of stroke and knowledge of potential risk factors among Omani patients at increased risk for stroke. BMC Neurol. 2006;20(6):38.
Acknowledgements
We extend our gratitude to all participants for their willingness, tolerance and cooperation offered during this study.
Funding
This study was sponsored by the PedPal Research Initiative and Jakaya Kikwete Cardiac Institute.
Author information
Authors and Affiliations
Contributions
PP and PRK conceived the study. ZSM, MK, LM, SK, GM, and AN conducted all the interviews, as well as anthropometric and blood pressure measurements. SVB, HAM and EK performed the necessary investigations (i.e., ECHOs and ECGs). HYF conducted nutritional counselling and education. JM, PRK, PP, and SVB participated in patient management. ZSM entered all the data while PP performed all the data cleaning and analysis. The corresponding author (PP) wrote the first draft of the manuscript, and other authors contributed to and approved it. All authors made the decision to submit the manuscript for publication. All authors undertake responsibility for the accuracy and integrity of the analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was submitted to, and approved by the Ethical Committee, of the Jakaya Kikwete Cardiac Institute (JKCI) on May 28th, 2022. Written informed consent was obtained from all study participants. This research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pallangyo, P., Mkojera, Z.S., Komba, M. et al. Public knowledge of risk factors and warning signs of heart attack and stroke. Egypt J Neurol Psychiatry Neurosurg 60, 12 (2024). https://doi.org/10.1186/s41983-023-00780-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00780-x